The sonographic and histopathologic correlation study of solitary nevus lipomatosus cutaneus superficialis
Corresponding Author: Dr. Chun-Yu Cheng, Department of Dermatology, Chang Gung Memorial Hospital and Chang Gung University College of Medicine, Taoyuan, Taiwan. b9102028@stmail.cgu.edu.tw
-
Received: ,
Accepted: ,
How to cite this article: Tsai Y, Cheng C. The sonographic and histopathologic correlation study of solitary nevus lipomatosus cutaneus superficialis. Indian J Dermatol Venereol Leprol 2022;88:819-22.
Sir,
Nevus lipomatosus cutaneus superficialis (NLCS) is a rare type of connective tissue nevus, first described in 1921 by Hoffman and Zurhelle.1 It has been classified into two clinical types: multiple (classic) and solitary. The classic type is characterised by papules or plaques commonly located on the lower back, buttocks and thighs. The solitary type usually presents with a solitary nodule or papule. There are only limited studies describing the image features of this condition and no study investigating the ultrasonographic characteristics.2 Therefore, we conducted the present study to analyse the sonographic and histopathologic correlation of this entity.
In the present study, we collected four cases of histopathology confirmed nevus lipomatosus cutaneus superficialis at Chang Gung Memorial Hospital, Taoyuan branch, from 1st January 2020 through 31st May 2021. All the sonographic examination was performed by one dermatologist (C.Y.C.) using Acuson ×150TM ultrasound system (Siemens Medical Solutions USA, Mountain View, CA). Digital images were reviewed by two of the authors (C.Y.C. and Y.W.T.), and the sonographic features were confirmed only if the two evaluators reached a consensus.
All four cases were women with a mean age of 60 ± 6.4 (51–69) years. The affected areas included thighs (n = 3, 75%) and back (n = 1, 25%) and the mean size was 10 ± 2.8 (range: 8.0–14.8) mm. All cases were solitary type of nevus lipomatosus cutaneus superficialis [Figures 1a–d]. The characteristics of sonographic findings were demonstrated in [Figures 1e–h]. In the ultrasonographic examination, all tumours were located in the dermis to subcutis and exhibited heterogeneous texture and ovoid shape. [Table 1] Most cases were isoechoic (n = 3, 75%), while one case was hyperechoic. Focal hypoechoic areas and posterior acoustic shadows were seen in all cases. The histopathological features were characterized by the proliferation of ectopic mature adipocytes with the thickening of collagen bundles in the dermis. [Figures 1i–l].
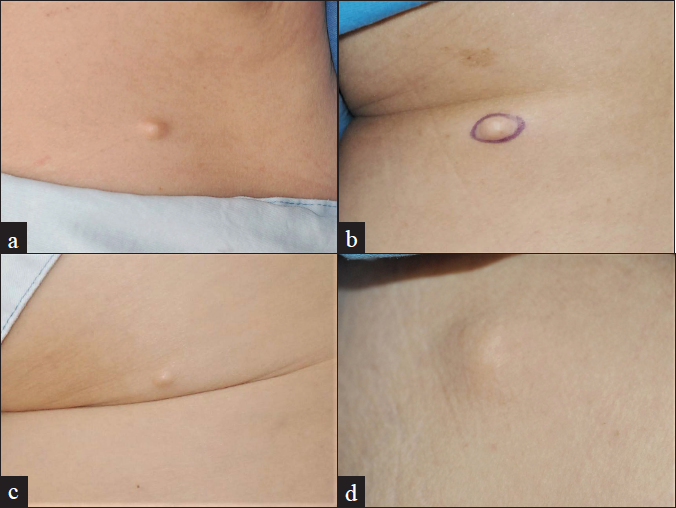
- (a) A skin colored nodule on the back of case 1; (b) A skin colored nodule on the right thigh of case 2; (c) A skin colored nodule on the right thigh of case 3; (d) A skin colored nodule on the left thigh of case 4
![Ultrasonography of case 1–3 showed a heterogeneous isoechoic mass with the focal hypoechoic area (white arrowheads) and posterior acoustic shadow [Ultrasound frequency: 11.4 MHz]. Ultrasonography of case 4 showed a hyperechoic lesion with the central hypoechoic area (white arrowhead) and posterior acoustic shadow [Ultrasound frequency: 11.4 MHz]](/content/126/2022/88/6/img/IJDVL-88-6-819-g002.png)
- Ultrasonography of case 1–3 showed a heterogeneous isoechoic mass with the focal hypoechoic area (white arrowheads) and posterior acoustic shadow [Ultrasound frequency: 11.4 MHz]. Ultrasonography of case 4 showed a hyperechoic lesion with the central hypoechoic area (white arrowhead) and posterior acoustic shadow [Ultrasound frequency: 11.4 MHz]
| Case | Gender | Age (yrs) | Location | Size (mm) | Sonographic features | Clinical differential diagnosis | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Location | Echogenicity | Homogeneity | Focal hypoechoic area | Posterior acoustic shadow | ||||||
| 1 | Female | 60 | Back | 14.8×5.8×6.5 | Dermis to subcutis | Isoechoic | Heterogeneous | Present | Present | NLCS, NF |
| 2 | Female | 51 | Right thigh | 8.1×4.2×4.0 | Dermis to subcutis | Isoechoic | Heterogeneous | Present | Present | NLCS, NF |
| 3 | Female | 69 | Right thigh | 9.2×5.0×4.3 | Dermis to subcutis | Isoechoic | Heterogeneous | Present | Present | NLCS, NF |
| 4 | Female | 60 | Left thigh | 8.0×5.0×4.6 | Dermis to subcutis | Hyperechoic | Heterogeneous | Present | Present | NLCS, NF |
NF: Neurofibroma, NLCS: Nevus lipomatosus cutaneous superficialis
![The histopathology of case 1–3 revealed characteristic proliferation of ectopic mature adipocytes with thickening of collagen bundles present in the dermis [H and E ×20]. The histopathology of case 4 revealed closely packed adipocytes intermingled with collagen bundles [H and E, ×40]](/content/126/2022/88/6/img/IJDVL-88-6-819-g003.png)
- The histopathology of case 1–3 revealed characteristic proliferation of ectopic mature adipocytes with thickening of collagen bundles present in the dermis [H and E ×20]. The histopathology of case 4 revealed closely packed adipocytes intermingled with collagen bundles [H and E, ×40]
The present study demonstrated that the ultrasonographic features of nevus lipomatosus cutaneus superficialis were mainly heterogeneous isoechoic ovoid shape with focal hypoechoic area and posterior acoustic shadow. We suppose that adipose tissue interposed into the dermis and intermingled with collagen bundles results in heterogeneity in sonography. The isoechoic structure was the dilated collagen bundles caused by the interspersion of adipocytes, while the hypoechoic area was the adipose tissue within the tumour. Additionally, the acoustic impedance of the dermis is higher than fatty tissue. Therefore, when the ultrasonic wave re-enters from the adipose tissue of the nevus into the dermis, some of the acoustic energy may reflect and the transmission is reduced, resulting in acoustic shadow.
Clinically, solitary nevus lipomatosus cutaneus superficialis should be differentiated from lipoma, neurofibroma, angioleiomyoma, neuroma and dermatofibroma. Ultrasonography can be applied to differentiate from these tumours. Lipoma and angioleiomyoma are mostly located in subcutis, while this is mainly located in the dermis.2 In addition, the sonographic features of angioleiomyoma are mainly homogeneous hypoechoic lesion with protrusions on one or both ends along with posterior acoustic enhancement.2 Neurofibroma is mostly a homogenous hypoechoic lesion without posterior acoustic shadow, whereas this nevus is a heterogeneous isoechoic lesion with posterior acoustic shadow.3 Neuroma and dermatofibroma are hypoechoic lesions in the dermis.4,5
In conclusion, we demonstrated the sonographic features of nevus lipomatosus cutaneus superficialis and analysed the sonographic and histopathologic correlation. Sonography is a noninvasive and real-time diagnostic tool, valuable in assisting the diagnosis of nevus lipomatosus cutaneus superficialis.
Declaration of patient consent
Patient consent is not required as the patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest
References
- Nevus lipomatosus cutaneous superficialis: An unusual presentation. Indian Dermatol Online J. 2012;3:196-8.
- [CrossRef] [PubMed] [Google Scholar]
- Angioleiomyoma of the extremities: Findings on ultrasonography and magnetic resonance imaging. J Med Ultrasound. 2019;38:1201-8.
- [CrossRef] [PubMed] [Google Scholar]
- Sonographic differentiation between schwannomas and neurofibromas in the musculoskeletal system. J Ultrasound Med. 2015;34:2253-60.
- [CrossRef] [PubMed] [Google Scholar]
- Utility of high-frequency ultrasonography in the diagnosis of benign and malignant skin tumors. Indian J Dermatol Venereol Leprol. 2017;83:162-82.
- [CrossRef] [PubMed] [Google Scholar]
- Usefulness of ultrasound for the diagnosis of dermatofibroma. Med Ultrason. 2016;18:132-3.
- [CrossRef] [PubMed] [Google Scholar]





