The utility of dermoscopy in pediatric vascular anomalies
Corresponding author: Dr. Neetu Bhari, Department of Dermatology and Venereology, All India Institute of Medical Sciences, Delhi, India. drntbhari@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Bhagwat A, Mehta N, Goyal A, Arava S, Ramam M, Sethuraman G, et al. The utility of dermoscopy in pediatric vascular anomalies. Indian J Dermatol Venereol Leprol. 2025;91:363-8. doi: 10.25259/IJDVL_1053_2023
Abstract
Background
Vascular anomalies show highly variable morphology, making clinical identification difficult. Dermoscopy is a non-invasive tool which can aid in their diagnosis, but studies of dermoscopy in vascular anomalies are limited.
Aim
This study aimed to describe the dermoscopic findings in vascular anomalies in children and evaluate their usefulness over clinical examination alone.
Methods
Consecutive children with congenital or acquired vascular lesions diagnosed by two experienced dermatologists after detailed history and examination were recruited. Predominant dermoscopic findings of a representative lesion were recorded in a pre-designed proforma with a consensus of two dermatologists trained in dermoscopy. In cases of clinical diagnostic uncertainty, suitable histopathological and radiological investigations were done.
Results
Sixty-one patients (33 tumours, 26 malformations, and 2 unclassified anomalies) were recruited. The most observed condition was infantile haemangioma (IH) (37.7%) which showed red lacunae and irregularly branched thick-tortuous and thin-serpentine vessels in mixed haemangiomas (30.4%), prominent lacunae in superficial haemangiomas (34.8%) and only branched vessels in deep and treated/involuting (34.8%) haemangiomas. Lacunae were predominantly seen in superficial haemangiomas (p=0.0498) and were missing in deep and involuting haemangiomas (p=0.0027). Port-wine stain (13.1%) showed irregular reticular vessels along with dots and globules with thickness of the network being proportionate to the darker shade clinically. In all, there were nine (14.75%) cases where there was diagnostic uncertainty using clinical features alone and histopathological/radiological investigations were required to establish the final diagnosis. In them, dermoscopy showed findings (as described in previous literature) suggestive of the correct final diagnosis.
Limitations
Histopathological and radiological investigations were done only in cases where the clinical diagnosis was uncertain.
Conclusion
Dermoscopy is a useful tool in differentiating between different vascular anomalies such as IH and capillary malformations (CMs) which have different management strategies. Dermoscopy may also be useful in differentiating superficial from deep haemangiomas and proliferating from involuting haemangiomas. It can also help in determining the depth of CMs. Thus, it can obviate the need for invasive diagnostic procedures in paediatric vascular lesions and can guide appropriate treatment and prognosis.
Keywords
Vascular tumours
vascular malformations
dermoscopy
infantile hemangioma
capillary malformation
Introduction
Vascular anomalies manifest with a wide range of symptoms and morphology, making clinical identification difficult. The current International Society for the Study of Vascular Anomalies (ISSVA) classification divides them into two categories – vascular tumours and vascular malformations.1 Correct diagnosis is important for treatment and prognostication. The majority can be diagnosed clinically; however, some cases can be atypical or have overlapping features.2,3 Dermoscopy can potentially reduce the need for radiological investigations and biopsies which are difficult to perform in children and require inputs from other specialties. Robust studies on dermoscopic patterns of various vascular anomalies and their differentiation are lacking, especially in skin of colour.4,5 We conducted this study to describe the dermoscopic findings and their relative frequencies in congenital and acquired paediatric vascular anomalies. We also wanted to evaluate correlations between clinical subtypes and dermoscopy findings in paediatric vascular anomalies and to find out if dermoscopy adds to the clinical examination in making the final diagnosis in paediatric vascular anomalies
Methods
All children aged below 18 years with congenital/acquired vascular lesions presenting to the outpatient department of the tertiary referral study centre for over a period of 2 years (July 2020 to June 2022) were recruited in this prospective case-series through consecutive non-probability sampling. Detailed clinical history, examination, and clinical photographs were collected in a standard proforma. A clinical diagnosis was established with a consensus of two experienced paediatric dermatologists, as per the definitions in Supplement 1. In cases with diagnostic uncertainty, histopathological or appropriate radiological investigations (ultrasound/magnetic resonance imaging) were done to establish the final diagnosis. Dermoscopic examination was done over a representative area using Dino-Lite AF4115ZT 5MP, AnMo Electronics Corporation, Taiwan with up to 200× magnification in polarised mode and descriptive findings were recorded as per a checklist which included definitions as per the consensus statements of the International Dermoscopic Society (IDS) [Supplement 2], including those for skin of colour by two experienced dermatologists trained in dermoscopy.6–8 The association between various clinical subtypes and dermoscopy findings were assessed. Statistical analysis was done using Fisher’s exact test for proportional data using R version 4.3.3.
For cases with multiple differentials, after establishing the final diagnosis through investigations, the clinical photos and case summary were shown to a blinded dermatologist trained in vascular dermoscopy, who was unaware of the final diagnosis and investigations and was asked for differentials. Afterwards, dermoscopy photos were shown and the blinded dermatologist was asked again for differentials or a single diagnosis if it could be made with reasonable certainty. To find out the utility of dermoscopy, concordance of the diagnosis of the blinded dermatologist after dermoscopy with the final diagnosis was assessed.
Results
Sixty-one children, 28 (45.90%) males, and 33 (54.09%) females, were recruited in the study period. Their mean age was 72.31±69.48 months and median was 36 months. Thirty-three (54.09%) participants had vascular tumours, 26 (42.62%) had malformations, and the rest [2 (3.28%)] were unclassified (one each of angiokeratoma and angioma serpiginosum).
Among the tumours, infantile haemangiomas (IHs) were the commonest, seen in 23 (37.70%) cases. Others included three congenital haemangiomas (CHs) (4.91%), one tufted angioma (TA) (1.63%), two kaposiform haemangioendotheliomas (KHEs) (3.27%) and four pyogenic granulomas (PGs) (6.55%). Malformations included nine cases (14.75%) of venous malformations (VM), eight cases (13.11%) of capillary malformations (CMs), six cases (9.83%) of lymphatic malformations (LMs), one case of (1.63%) veno-LM and two cases (3.27%) of CM with arterio-venous malformation (CM-AVM).
Vascular tumours
IH showed a female preponderance (males-9, 39.13%; females-14, 60.87%). It was divided into superficial, mixed, and deep type clinically based on the depth of the lesion and proliferating and involuting phase based on evolution. On dermoscopy [Table 1], superficial IH (n=8, 34.78%) showed both red lacunae as well as irregularly branched vessels in five (62.5%) cases, red lacunae as an isolated finding in two (25.00%) cases and only irregular branched vessels were seen in one (12.50%) case [Figures 1a, 1b]. Seven (87.50%) cases showed a red-white background and one (12.50%) showed a red background. In mixed-type IH (n=7, 30.43%), both lacunae and irregular branched vessels were seen in three (42.86%) cases, only thick tortuous irregular branched vessels in another three (42.86%) cases, whereas both thick and thin irregular branched vessels were seen only in one (14.29%) case [Figures 1c, 1d]. No case showed lacunae as an isolated finding. Six (85.71%) cases showed a red-white background and one (14.29%) case showed a red background. One case (14.29%) showed haemorrhagic crusting. In deep IH (n=2, 8.70%), irregularly branched vessels were seen in one (50.00%) case and the other (50.00%) showed comma-like vessels with both (100.00%) having a white background [Figures 1e, 1f]. None of the cases showed red lacunae.
| Only lacunae | Only irregular- branched vessels | Both | Comma shaped | Vessel arrangement | Background | |
|---|---|---|---|---|---|---|
| Superficial (n=8) | 2 |
T= 1 S= 0 T,S= 0 |
L+T= 1 L+S= 1 L+T,S= 3 |
0 | Irregular |
Red-white = 7 Red = 1 |
| Mixed (n=7) | 0 |
T= 3 S= 0 T,S= 1 |
L+T= 1 L+S= 1 L+T,S= 1 |
0 | Irregular |
Red-white = 6 Red = 1 |
| Deep (n=2) | 0 | T=1 | 0 | 1 | Irregular | White = 2 |
| Involuting/on long-term treatment (n=6) | 0 |
T= 2 S= 0 T,S= 4 |
0 | 0 | Irregular |
Red-white = 4 White = 1 White with brownish lines = 1 Red-white with brownish lines = 1 |
| Total, n=23 | L- 2 |
Only T = 7 Only S = 0 Both = 5 |
L+T = 2 L+S = 2 L+T,S = 4 |
1 | Irregular = 23 |
Red-white = 17 Red = 2 White = 2 Red-white with brown lines = 1 White with brown lines = 1 |
T: Tortuous/thick vessels, S: Serpentine/thin vessels, L: Lacunae
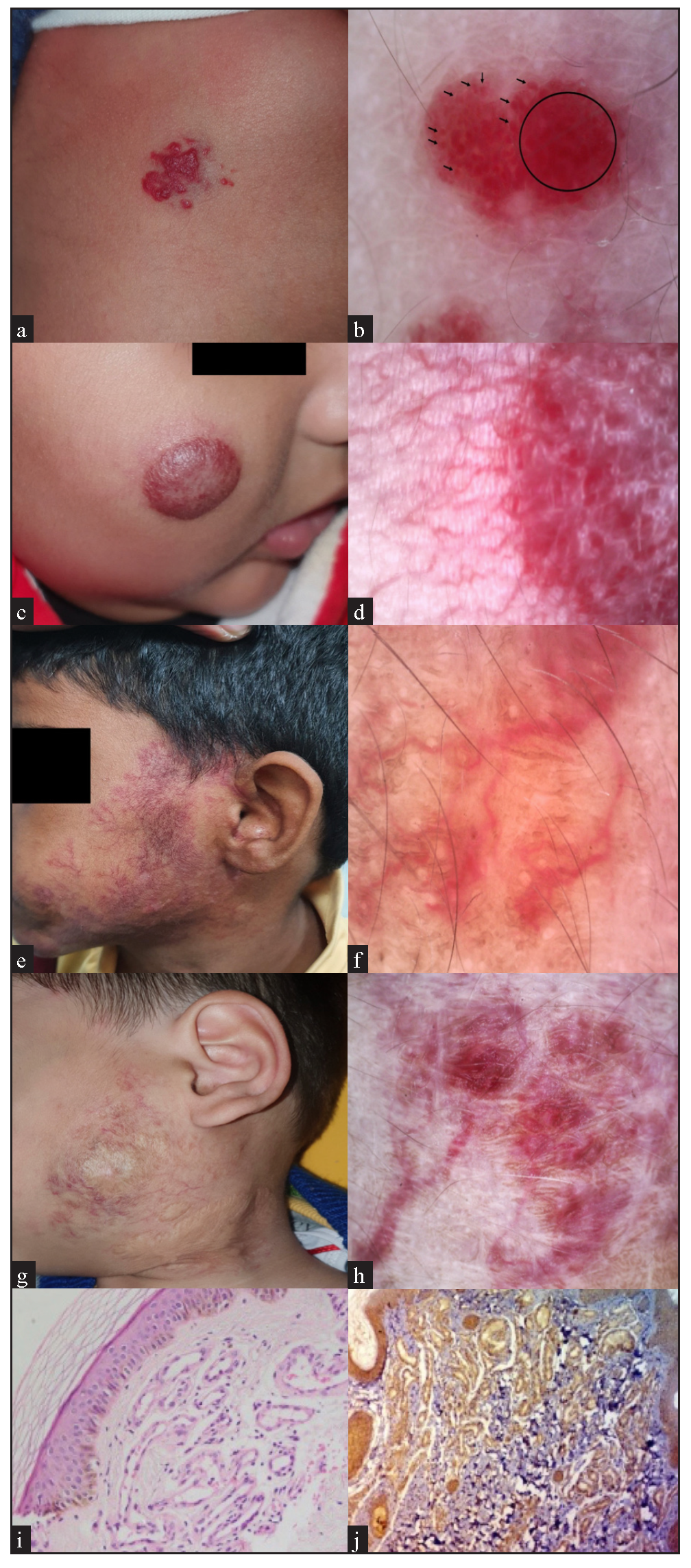
- Infantile hemangioma (IH) (a) Superficial IH- clinical, and (b) dermoscopy, showing red structureless area (circle) and red lacunae (arrows). (c) Mixed IH- clinical, and (d) dermoscopy showing red structureless area, few red lacunae, along with linear branched vessels with a red-white background. (e) Deep IH- clinical, and (f) dermoscopy showing linear vessels without any lacunae. (g) Involuting IH- clinical, and (h) dermoscopy showing linear irregular branched vessels with brown lines (Dino-Lite AF4115ZT 5MP, variable magnification 120-160x, b, d, f- polarised, h- non-polarised). (i) Histopathology of IH in involuting phase showing proliferation of capillaries with plump endothelial cells (Haematoxylin and eosin, 200x), and (j) Glucose transporter 1 (GLUT1) positivity on immunohistochemistry.
In involuting IH (n=6, 26.09%), irregular branched vessels, both thick-tortuous and thin-serpentine, were seen. The background was predominantly red-white to white with two cases (33.33%) having brown lines in addition [Figures 1g, 1h].
On comparing subtypes, lacunae were consistently seen in superficial (7/8, 87.5%) vs other haemangiomas (3/9, 33.33%) (p=0.0498) and were not seen in deep (0/2) or involuting/on-treatment haemangiomas (0/6), compared to superficial (7/8, 87.5%) or mixed (3/7, 42.9%) haemangiomas in the proliferative phase (p=0.0027).
Histopathological examination was done for one (4.35%) mildly elevated lesion over the lip. It showed multiple thin- and thick-walled capillaries showing plump endothelial cells and glucose transporter type 1 (GLUT-1) positivity [Figures 1i, 1j]. On ultrasound examination, three clinically doubtful cases showed heterogeneous echotexture, solid morphology, and increased colour vascularity compatible with IH.
Based on history and clinical examination, three (4.91%) children were diagnosed with CH, two (66.67%) of whom were of partially involuted type while one (33.33%) was of the non-involuting type. In the non-involuting type, dermoscopy showed both thick- and thin-branched vessels arranged irregularly with a red-white background. Partially involuted CH showed only thin-branched vessels arranged irregularly with red-white background and brown lines in one case; and both red lacunae and thick- and thin-branched vessels arranged irregularly with brown background in the other.
Histopathological examination was done for one (33.33%) clinically doubtful case of CH. It showed haphazardly arranged vessels with plump endothelial cells, dissecting the collagen bundles. Ultrasound examination done for another doubtful case showed mild increased vascularity with few prominent vessels in the subcutaneous tissue, consistent with a vascular tumour.
On dermoscopic examination, a case of TA and two cases of KHE showed findings of branched linear irregular vessels against a red-white background, similar to those of IH (Figure 2a,b). Histopathological examination of a patient with suspected TA revealed a ‘cannon-ball’ appearance of the lobules of proliferating endothelial cells.
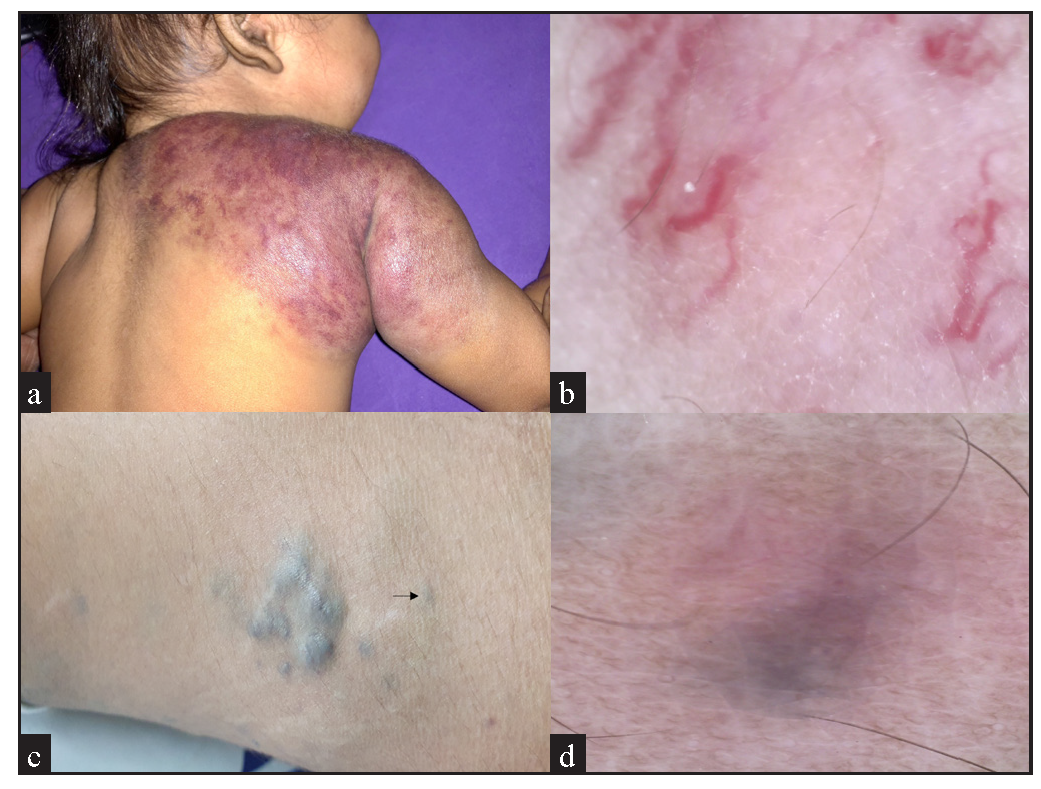
- (a) A child with kaposiform hemangiothelioma showing Kasabach-Merritt phenomenon, over the shoulder, presenting as a dusky red ill-defined swelling, and (b) its dermoscopy, showing irregular vessels, similar to the ones seen in infantile hemangiomas or tufted angiomas. (Dino-Lite AF4115ZT 5MP, magnification 160x, polarised). (c) A venous malformation, presenting as discrete and linear bluish-green compressible swellings, and dermoscopy of one of the lesions (arrow) (d) showing a bluish structureless area (Dino-Lite AF4115ZT 5MP, magnification 160x, polarised).
Vascular malformations
Out of 26 cases of vascular malformations, VM was seen most frequently (n=9, 34.62%). On dermoscopic examination, VM showed violaceous ill-defined areas with branched linear irregular vessels (Figure 2c,d).
The second most common malformation seen was the port-wine stain (PWS) type of CM (n=8, 30.77%). The dermoscopic findings were classified as dots and globules and a broken network of thick and/or thin vessels. Both broken networks of thick and thin vessels along with red dots/globules were seen in three (37.50%) patients. Only a broken network of vessels was seen in three (37.50%) patients with one (12.50%) patient each of thick, thin, and both thick and thin vessels. There was the presence of dots/globules with thin vessels in one (12.50%) patient and dots/globules with thick vessels in another (12.50%). No patient showed dots/globules as an isolated finding. Thicker sausage-shaped vessels, along with a more prominent but less broken network, were seen in darker and hypertrophic PWS [Figures 3a-f]. Six (75%) patients showed a brown background while the rest two (25%) had a red-white background. The clinical shade of the lesions and thickness of the vessels on dermoscopy were graded as grade 1/2/3 – the higher number indicating darker shade and thicker vessels, respectively, using the consensus of two investigator dermatologists. The thickness of the network (graded as 1,2,2,2,1,3 and 2 for the seven cases) were proportionate to the clinically darker shade (graded as 1,2,2,2,1,3 and 1, respectively).
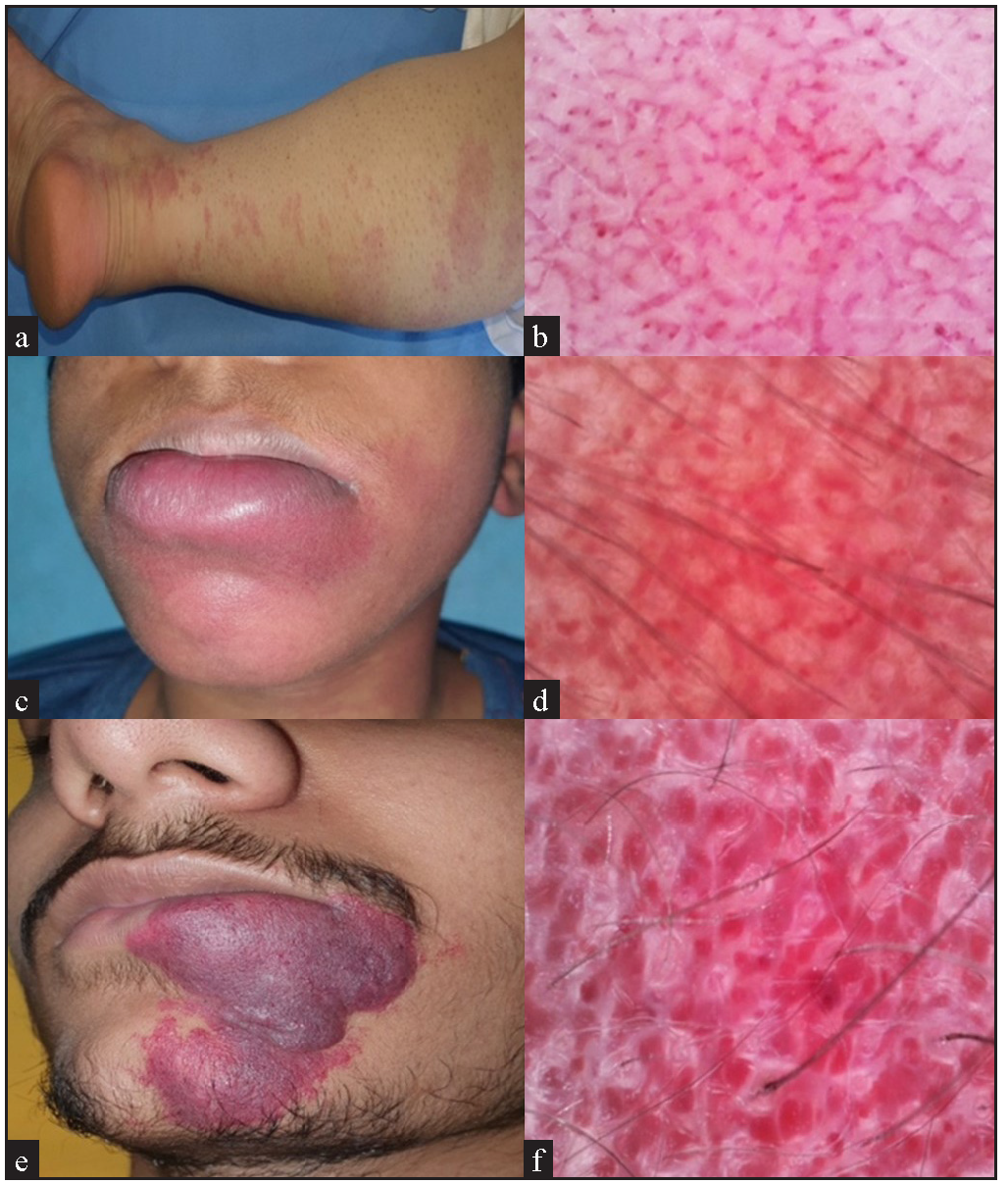
- Clinical and dermoscopic images of capillary malformation/port-wine stain showing (a) faint pink colour clinically corresponding to (b) dots and globules and broken network of thin vessels in dermoscopy, and (c) dark red colour showing (d) broken network of thick vessels, and (e) dark purple hypertrophic port-wine stain showing (f) sausage-shaped very thick vessels in a mostly intact network on dermoscopy (Dino-Lite AF4115ZT 5MP, magnification 160x, polarised).
In nine (14.75%) cases, the diagnosis could not be made on clinical grounds alone and additional investigations (radiological/histopathological) were done to reach the final diagnosis. Clinical pictures, a combined list of clinical differentials by two independent blinded investigators, and pictures of dermoscopic findings were shown to a third dermatologist trained in dermoscopy, who was blinded to the results of the investigation. The third dermatologist was asked to select a single preferred diagnosis out of the differentials or to propose a single new diagnosis. In all these nine cases, the preferred/added diagnosis obtained by the addition of dermoscopy to the clinical list of differentials was the same as the final diagnosis made after the relevant investigations [Table 2].
| Number | Clinical differentials | Diagnosis by the blinded dermatologist after reviewing dermoscopy pictures |
Additional investigations (HPE/Radiological) |
Final diagnosis |
|---|---|---|---|---|
| 1. | CM, IH | IH | HPE-IH | IH |
| 2. | CM, CH | CM-AVM | USG-CM with underlying AVM | CM-AVM |
| 3. | CVM | IH | USG-Vascular tumour, possibly IH | IH |
| 4. | CVM | IH | USG-Vascular tumour | IH |
| 5. | CVM | CM-AVM | USG-CM with underlying AVM | CM-AVM |
| 6. | Klippel-Trenaunay syndrome, CVM, VVM | VVM | HPE-VVM | VVM |
| 7. | Veno-lymphatic malformation, Plantar wart, Callosity | Angiokeratoma | HPE-angiokeratoma | Angiokeratoma |
| 8. | CM, Angioma serpiginosum | Angioma serpiginosum | HPE-angioma serpiginosum | Angioma serpiginosum |
| 9. | CM, CH | Haemangioma |
USG-haemangioma HPE-haemangioma |
CH |
HPE: Histopathological examination, USG: Ultrasonography, IH: Infantile haemangioma, CH: Congenital haemangioma, CM: Capillary malformation, AVM: Arterio-venous malformation, CM-AVM: Capillary malformation with arterio-venous malformation, CVM: Capillary venous malformation, VVM: Verrucous venous malformation
Discussion
Dermoscopy is a useful tool in classifying various congenital and acquired vascular lesions in children.9 Although various case series on dermoscopy in IH exist, different findings based on the depth of IH have not been elaborated before.5,10–12 Linear vessels in IH can be classified both as branching and curved as per consensus terminologies, as they divide into smaller diameter vessels and also show multiple bends and curvatures.6,7 The number of bends/curvatures was large enough for them to be called tortuous (if thick) or serpentine (if thin) by us. Presence/absence of red linear vessels has been used to subdivide IH into mixed and superficial IH in previous studies.13 In our study, isolated red lacunae were seen in two (25%) cases of superficial IH, none in mixed/deep IH. This can be used to subclassify IH based on depth using dermoscopy. Similarly, none of the involuting lesions showed lacunae which were observed either in isolation or in combination in proliferating lesions. Involution of IH likely begins with the disappearance of lacunae showing that the superficial component of IH resolves first.
It is difficult to differentiate IH from CH as both show similar dermoscopic findings. Dermoscopic findings of TA have been described before in a few case reports as telangiectasias or red lacunae separated by whitish thin septae with a red background and perifollicular brown areas.14,15 Patients with TA and KHE already on treatment usually present as faint erythema which may be mistaken for CM. In these cases, dermoscopy shows features suggestive of a haemangioma rather than malformation, as described in our study [Figure 2a-b].
In dermoscopy of CM, red globules corresponding to superficial vertical papillary vessels, red linear vessels corresponding to deeper horizontal subpapillary capillaries, and sausage-shaped vessels in thick CM have been described.9,16 However, in our study, we found that these dots/globules and linear vessels were part of a broken network rather than individual round/linear vessels. There was a network of multiple interconnected polygonal units of vessels with almost similar diameter (in contrast with IH where vessels branch to lesser-diameter branches) which resembled a normal skin vasculature pattern. However, it was broken at places and exaggerated/thickened at places (forming the sausage-shaped vessels) and red dots/globules were mostly seen at the angles of the polygons [Figure 3a-f]. These findings reflect the malformation process in the normal vasculature. This broken/irregular reticular arrangement pattern has not been emphasised in previous studies, possibly due to the lesser magnification (10–20×) of the hand-held dermoscopes used in them, compared to the video-dermoscopy used in this study.5,17
The strengths of this study are prospective design, the inclusion of multiple conditions together to better gauge differences, clinical-dermoscopic correlation, and verification of diagnosis through histopathology/radiology in doubtful cases. We were able to establish the practical relevance of dermoscopy over clinical examination alone, since in 14.75% cases where additional investigations were needed, dermoscopy could have prevented their use. A limitation was that histological and radiological investigations were done only for cases with doubtful clinical diagnosis. Another limitation was that the clinical shade of the lesions and thickness of the vessels on dermoscopy were defined using subjective consensus of non-blinded investigator dermatologists rather than objective measures which could lead to a potential bias.
Conclusion
Dermoscopy can be used to accurately differentiate between IH/CH from CM. Dermoscopy may also be useful in differentiating between superficial and deep haemangiomas and between proliferating and involuting haemangiomas in determining the depth of CM, all of which has a bearing on therapeutic strategies, counselling, and prognostication. Dermoscopy can thus reduce the need of invasive and costly investigations in the diagnosis of vascular anomalies.
Ethical approval
The research/study was approved by the Institutional Review Board at All India Institute of Medical Sciences, Delhi, India, number IECPG-276, dated 22.07.2020.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Classification | International Society for the Study of Vascular Anomalies [WWW Document]. URL https://www.issva.org/classification [last accessed on 27 June 2023].
- PHACE syndrome misdiagnosed as a port-wine stain. BMJ Case Rep. 2015;2015:bcr2015209889.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of terminology for vascular anomalies in current literature. Plast Reconstr Surg. 2011;127:347-51.
- [CrossRef] [PubMed] [Google Scholar]
- Dermatoscopy of inflammatory diseases in skin of color. Indian Dermatol Online J. 2021;12:45-57.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Dermoscopic analysis of vascular malformations and tumors based upon dominant vascular dermoscopic features: A retrospective analysis from a tertiary care center of East India. Cureus. 2022;14:e26292.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Standardization of terminology in dermoscopy/dermatoscopy: Results of the third consensus conference of the International Society of Dermoscopy. J Am Acad Dermatol. 2016;74:1093-106.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Standardization of dermoscopic terminology and basic dermoscopic parameters to evaluate in general dermatology (non-neoplastic dermatoses): An expert consensus on behalf of the International Dermoscopy Society. Br J Dermatol. 2020;182:454-67.
- [CrossRef] [PubMed] [Google Scholar]
- International Dermoscopy Society (IDS) criteria for skin tumors: validation for skin of color through a delphi expert consensus by the “Imaging in Skin of Color” IDS task force. Dermatol Pract Concept. 2023;13:e2023067.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The dermoscopic features in infantile hemangioma. Pediatr Dermatol. 2011;28:591-3.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical, dermoscopic, and histopathologic features in a case of infantile hemangioma without proliferation. Pediatr Dermatol. 2011;28:66-8.
- [CrossRef] [PubMed] [Google Scholar]
- Dermoscopic features of infantile hemangioma during treatment with topical propranolol. JAAD Int. 2020;1:121-3.
- [CrossRef] [PubMed] [Google Scholar]
- Dermoscopic appearances in the superficial and deep type of infantile hemangioma. J Cosmet Dermatological Sci Applications. 2012;2:212-3.
- [CrossRef] [Google Scholar]
- Tufted angioma with coagulopathy: A dermoscopic evaluation and successful treatment. Int J Dermatol. 2021;60:e379-81.
- [CrossRef] [PubMed] [Google Scholar]
- Tufted angioma presented with segmental hyperpigmented plaque in a young Chinese woman. J Dermatol. 2010;37:190-2.
- [CrossRef] [PubMed] [Google Scholar]
- Dermoscopic features of port-wine stains: A study of 264 cases. Australas J Dermatol. 2021;62:e201-6.
- [CrossRef] [PubMed] [Google Scholar]
- Dermoscopy of cutaneous vascular lesions: An observational study. Clinical Dermatology Review. 2024;8:14-25.
- [CrossRef] [Google Scholar]






