Translate this page into:
Three cases of suspected chloracne in a family from Pune
Correspondence Address:
Aayush Gupta
B - 402, The Metropolitan, Near Darshan hall, Chinchwad, Pune - 411 033, Maharashtra
India
| How to cite this article: Sharma YK, Dash K, Gupta A, Ankadawar N, Prakash N, Mahajan P. Three cases of suspected chloracne in a family from Pune. Indian J Dermatol Venereol Leprol 2016;82:216-218 |
Sir,
Chloracne is an eruption of acne-like comedones, cysts and pustules following systemic absorption of aromatic hydrocarbons (′chloracnegens′) having a specific molecular configuration containing two benzene rings with halogen atoms occupying at least three of the lateral ring positions. [1],[2] Typically found as trace contaminants during synthesis of industrial chemicals, chloracnegens include dioxins especially 2, 3, 7, 8-tetrachlorodibenzo-p-dioxins, naphthalenes, biphenyls, dibenzofurans, azobenzenes and azoxybenzenes. Von Bettman first reported this eruption secondary to exposure to chlorine. Herxheimer coined the term ′chloracne′ based upon the lesional resemblance to acne vulgaris. However, the term chloracne is a misnomer in view of the characteristic disappearance of sebaceous glands, reduced rate of sebum excretion, xerosis and paucity of Propionibacterium acnes.[3]
A 40-year-old woman employed since 2 months for brushing the dye off clothes in a small cottage industry employing three persons, presented with complaints of reddish, itchy eruptions that appeared sequentially over the face and trunk within 3 weeks. Examination revealed multiple comedones and a few inflammatory papules and pustules involving the forehead and peripheral area of face especially the mandibular area. A few lesions were also present on the chest, axillae and thighs. Cysts were seen mainly over the neck and sternum [Figure - 1]a and b. General physical, ophthalmological and systemic examinations were non-contributory. Liver function tests and lipid profile were normal. Both her children had slaty hyperpigmentation, comedones and inflammatory pustules over forehead, cheeks and submandibular area [Figure - 1]c and d, which were more prominent in her 4-year-old girl than her 3-year-old boy.
 |
| Figure 1: Multiple comedones, inflammatory papules, pustules and occasional cysts over the (a) forehead, lateral side of face, maxillary and mandibular areas imparting a slate gray pigmentation. (b) Chest. Comedones, inflammatory papules and pustules over the lateral face (c) of daughter, (d) son. (e) post treatment residual erythematous macules over face and (f) residual comedones and pustules on the chest of the mother |
Histopathology of the lesion on the chest revealed dilated cystic follicular infundibula filled with keratin. The clinico-pathological picture, history of chemical exposure and unusual age for acne vulgaris prompted a diagnosis of chloracne. In the absence of facility for chemical analysis, it was thought that the amine releasing azo dye could be the probable cause. The patient was advised to seek alternative employment in view of the reported recalcitrance of chloracne. Isotretinoin (0.5 mg/kg daily) was administered considering her persistent demand for treatment. Patient discontinued her job at the dyeing factory and follow up after 6 months revealed appreciable regression with only a few residual lesions present over her chest [Figure - 1]e and f and complete subsidence of lesions in her children. Lesional biopsy from the chest continued to reveal dilated keratin-filled infundibular cyst, and absent sebaceous glands with minimal chronic perifollicular infiltrate [Figure - 2]a and b.
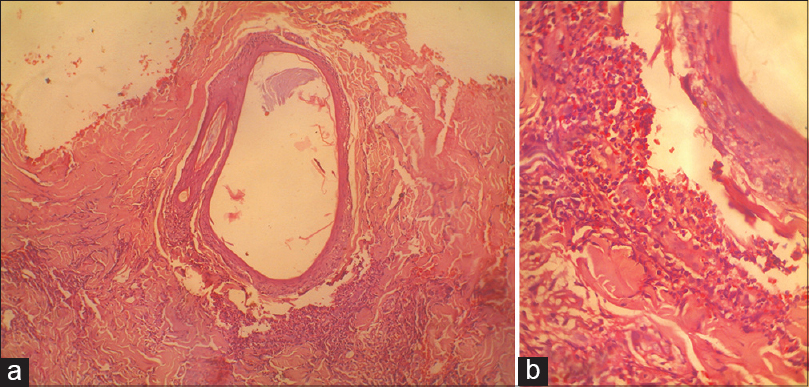 |
| Figure 2: (a) Infundibular keratinous cyst (H and E, ×100). (b) inflammatory infiltrate consisting of neutrophils and eosinophils around the partially ruptured keratinous cyst (H and E, ×400) |
Chloracne, a well-recognized, poorly understood condition, is one of the most sensitive markers of exposure to chloracnegens developing within a few weeks of systemic absorption following bodily contact, inhalation or ingestion. Initial erythema is followed within a few days by fine comedones involving almost every follicle imparting a slate-gray appearance affecting predominantly the malar and retroauricular areas and sparsely the chest, trunk and buttocks. [1] Perioral and ′T′ area are usually spared. Pale yellow cysts, intermingled with comedones, lessen numerically as the condition extends. In more severe cases, the pustular inflammatory lesions are usually more noticeable on the neck. [3]
The biological mechanisms of chloracne induction are still elusive. Chloracne has recently been attributed to the accelerated exit of activated stem cells from the bulge region, shifting the committed differentiation of their progeny from pilosebaceous to epidermal pattern. This results in epidermal/infundibular hyperplasia and hyperkeratinization, diminished sebaceous glands and diminished inferior portion of the follicles. Most of the effects of dioxin toxicity appear to be mediated by the aryl hydrocarbon receptor pathway. [4]
The severity of chloracne depends on the intensity and duration of exposure, chloracnegenic potency of the compound and the individual susceptibility. However chloracne may develop even in the unexposed relatives of the affected individual by imbibing trace amount of chloracnegens either through direct contact or through contact with their work clothes and tools, as was the case in the children of our patient. [1] There is lack of knowledge regarding the lower limit of exposure to chloracnegens below which the disease is certain not to occur as well as the exposure level above which it is certain to occur. [5]
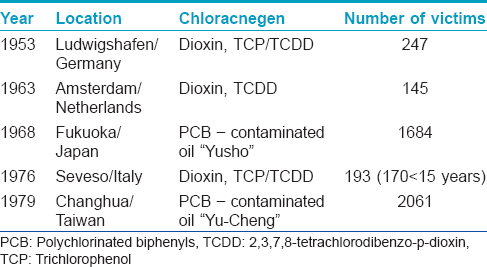
Histopathologically, miniaturization/disappearance of sebaceous glands and appearance of superficial/deeper epidermal cysts-now known as ′metabolizing acquired dioxin-induced skin hamartomas′-are considered as specific, almost diagnostic signs of chloracne. [6],[7] Since its first description in 1897 [Table - 1], many large scale dioxin poisonings have been reported, although none of them have been from India. Viktor Andriyovych Yushchenko, a former president of Ukraine, was sensationally poisoned with 2, 3, 7, 8- tetrachlorodibenzo-p-dioxin in 2004. [4]
Treatment necessitates removal of the individual from the site where he/she is being exposed to the toxin. Oral retinoids can provide some relief in this otherwise recalcitrant condition. Olestra, a synthetic dietary fat substitute, that binds to chloracnegens and accelerates their faecal excretion may prove to be a prospective therapy. [4]
The absence of previous reports from India of either an outbreak or even a sporadic case could possibly be due to lack of awareness. As per point 18, schedule III of the Factories Act (1948) of India, physicians coming across oil acne in factories with 10 or more employees, if consuming power, or 20 or more employees, if not consuming power should notify the same to the factory inspectors statewise. [8] In factories having fewer employees as in our case, the likely recourse is to intimate the factory owner as well as the municipal corporation, as was done by us. The owner of the factory confirmed discontinuation of and burning of the toxic dye. However, ideally dioxins should be incinerated in a unit that assures 99.99% destruction.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
| 1. |
Panteleyev AA, Bickers DR. Dioxin-induced chloracne - reconstructing the cellular and molecular mechanisms of a classic environmental disease. Exp Dermatol 2006;15:705-30.
[Google Scholar]
|
| 2. |
McDonnell JK, Taylor JS. Occupational and environmental acne. In: Handbook of occupational dermatology. In: Kanerva L, Elsner P, Wahlberg JE, Maibach HI, editors. 1 st ed. Berlin Heidelberg: Springer Verlag; 2000. p. 225e33.
[Google Scholar]
|
| 3. |
McDonagh AJ, Gawkrodger DJ, Walker AE. Chloracne - study of an outbreak with new clinical observations. Clin Exp Dermatol 1993;18:523-5.
[Google Scholar]
|
| 4. |
Ju Q, Yang K, Zouboulis CC, Ring J, Chen W. Chloracne: From clinic to research. Dermatologica Sinica 2012;30:2-6.
[Google Scholar]
|
| 5. |
Report by the Industrial Injuries Advisory Council in accordance with Section 171 of the Social Security Administration Act 1992 considering prescription for occupational chloracne. Occupational chloracne. Available from: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/224136/occupational-chloracne-report-iiac.pdf. [Last accessed on 2015 Feb 01].
[Google Scholar]
|
| 6. |
Passarini B, Infusino SD, Kasapi E. Chloracne: Still cause for concern. Dermatology 2010;221:63-70.
[Google Scholar]
|
| 7. |
Saurat JH, Sorg O. Chloracne, a misnomer and its implications. Dermatology 2010;221:23-6.
[Google Scholar]
|
| 8. |
List of chief inspectors of factories. Available from: http://www.dgfasli.nic.in/cif.htm. [Last accessed on 2015 Feb 01].
[Google Scholar]
|
Fulltext Views
4,718
PDF downloads
1,773





