Translate this page into:
Tick bite
2 Department of Dermatology, University of Osnabrueck, Osnabrueck, Lower Saxony, Germany,
Correspondence Address:
Min Zheng
Department of Dermatology, Second Affiliated Hospital, Zhejiang University School of Medicine, Hangzhou - 310009, Zhejiang Province, China
| How to cite this article: Liu CC, Landeck L, Zheng M. Tick bite. Indian J Dermatol Venereol Leprol 2014;80:269-270 |
Sir,
A 23-year-old girl presented to our department with a 1 month history of an embedded tick on her right clavicle. The patient had no fever, chills or other systemic symptoms. Physical examination revealed a live tick that was stuck very firmly to the skin of the right clavicle area and was seen to swing its feet [Figure - 1]a. Erythema was noticed around the attachment site [Figure - 1]a. Initial laboratory investigations were unremarkable. To avoid leaving the mouthparts of the tick embedded in the skin, a limited skin surgical excision including epidermis and dermis of diameter and depth of 4 mm to 6 mm of the entire area around the bite was performed to remove it completely. Histopathological examination showed a tick body full of blood with the mouthpart embedded in the upper dermis, with necrotized skin tissue around it [Figure - 1]b. Vessel dilatation and neutrophil infiltrate in the dermis were also observed [Figure - 1]b.
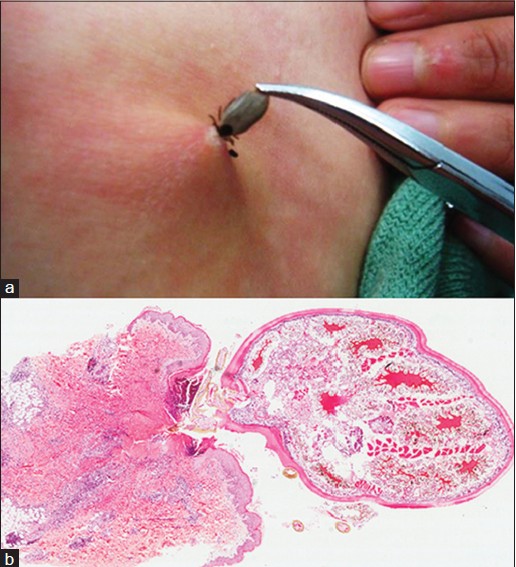 |
| Figure 1: (a) A live tick stuck to the skin of right clavicle area (b) Histological examination of the tick in the skin (H and E, ×4) |
Ticks are blood feeding external parasites which can cause local and systemic complications, including Lyme disease, tick-borne-encephalitis, tick-borne lymphadenopathy, secondary bacterial skin infection, reactive manifestations against tick allergens and granuloma formation. [1] During 3 months of follow-up, our patient did not show any systemic symptoms indicating that she just suffered a tick bite but did not acquire any tick-transmitted diseases.
Any tick found should be immediately and completely removed alive. Many methods of tick removal have been reported in the literature. Topical application of 2% erythromycin and 3% tetracycline preparations are ineffective in eliminating Borrelia burgdorferi from the tick bite site or in preventing dissemination to other tissues. [2] Limited surgical excision is an appropriate and safe tick removal technique and could remove the tick completely [3] without provoking the escape of infective body fluids from the tick into the wound site.
Persons who have undergone tick removal should be monitored for up to 30 days for signs and symptoms of tick-borne diseases. Tick numbers and tick-borne diseases should be regularly monitored in areas with a high risk of tick attacks.
| 1. |
Roupakias S, Mitsakou P, Nimer AA. Tick removal. J Prev Med Hyg 2011;52:40-4.
[Google Scholar]
|
| 2. |
Wormser GP, Daniels TJ, Bittker S, Cooper D, Wang G, Pavia CS. Failure of topical antibiotics to prevent disseminated Borrelia burgdorferi infection following a tick bite in C3H/HeJ mice. J Infect Dis 2012;205:991-4.
[Google Scholar]
|
| 3. |
Roupakias S, Mitsakou P, Nimer AA. Surgical tick removal. Wilderness Environ Med 2012;23:97-9.
[Google Scholar]
|
Fulltext Views
5,312
PDF downloads
2,113





