Translate this page into:
Tofacitinib for fibrosing alopecia in a pattern distribution
Corresponding author: Prof. Dingquan Yang, Department of Dermatology, China-Japan Friendship Hospital, Chaoyang District, Beijing, China. ydqlx@163.com
-
Received: ,
Accepted: ,
How to cite this article: Wu R, Li Y, Wang L, Yang Z, Liu Q, Yang D. Tofacitinib for fibrosing alopecia in a pattern distribution. Indian J Dermatol Venereol Leprol. doi: 10.25259/IJDVL_655_2024
Dear Editor,
Fibrosing alopecia in a pattern distribution (FAPD) is a distinct entity of lymphocytic primary cicatricial alopecia (PCA). Treatment for FAPD is challenging. Here, we describe a patient with FAPD who was previously misdiagnosed as androgenetic alopecia (AGA) and remained unresponsive to multiple treatment modalities. Clinical improvement was finally achieved with tofacitinib, an oral pan-Janus kinase (JAK) inhibitor. To our knowledge, this therapy has not been previously reported in the treatment of FAPD.
A 33-year-old man presented with progressive hair loss from the top of his scalp for over 5 years along with localised pruritus. Scalp examination revealed a male pattern distribution of alopecia, severe symmetric hair loss in a centroparietal distribution, recession of the frontal hairline, and mild perifollicular erythema within the alopecic area. The hair loss severity was Hamilton-Norwood grade VI [Figure 1a]. Trichoscopic examination demonstrated hair shaft diameter variability, predominance of single hair follicles (HFs), loss of HF ostia, perifollicular whitish spots and patches, perifollicular erythema, reticular pigmentation, hair shaft dystrophy and black dots [Figure 1b]. Skin biopsy revealed the decreased density of HFs and sebaceous glands, miniaturised follicles, lymphocytic interface dermatitis, concentric perifollicular lamellar fibrosis, naked hair shaft surrounded by foreign body granulomatous reaction, and fibrosis [Figures 2a–2d].

- Severe symmetric hair loss in a centroparietal distribution, degeneration of the frontal hairline, and mild perifollicular erythema within the alopecic area.
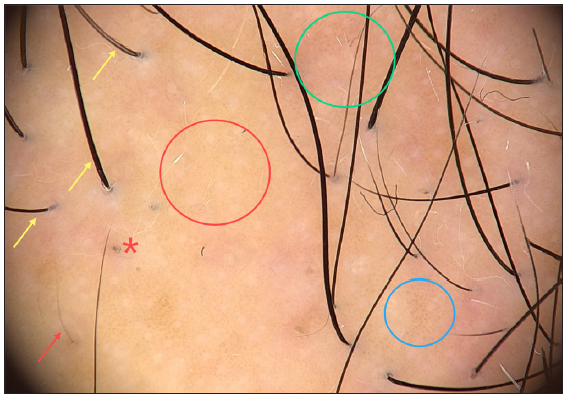
- Hair shaft diameter variability and increased single-hair follicular units (yellow arrow), loss of follicular ostia and perifollicular whitish spots and patches (red circle), perifollicular erythema (green circle), reticular pigmentation (blue circle), hair shaft dystrophy (red arrow) and black dot (red asterisk) (FotoFinder, polarised light, x20).
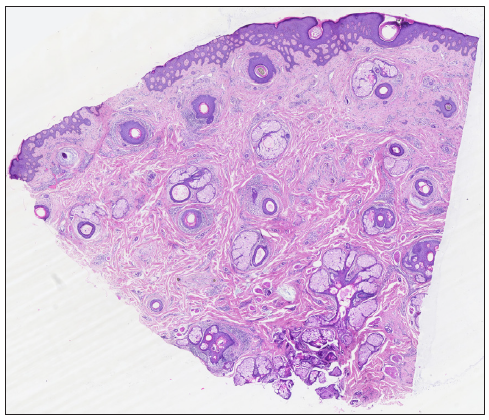
- Decreased density of hair follicles and sebaceous glands, miniaturised follicles, lymphocytic interface dermatitis, and concentric perifollicular lamellar fibrosis (Haematoxylin and eosin, 10x).
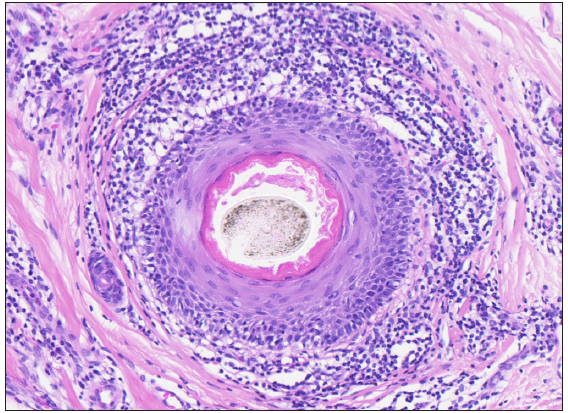
- Lymphocytic interface dermatitis (Haematoxylin and eosin, 200x).
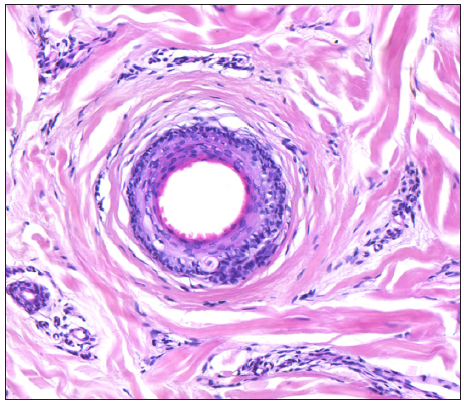
- Concentric perifollicular lamellar fibrosis (Haematoxylin and eosin, 200x).
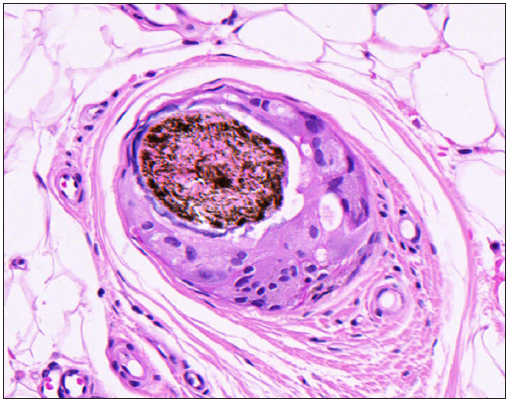
- Naked hair shaft surrounded by foreign body granulomatous reaction and fibrosis (Haematoxylin and eosin, 400x).
For the past 2 years, the patient had received diagnoses of AGA and was treated with finasteride (1 mg, once daily), minoxidil 5% solution (1 mL, twice daily), and microneedle therapy (0.5 mm depth, once weekly) for 6 months without any clinical improvement. FAPD was diagnosed on the basis of clinical, trichoscopic, and histopathological findings,
Being refractory to prior treatments, we initiated oral tofacitinib (5 mg, twice daily) following a full health assessment including complete blood count, biochemical tests, and screenings for tuberculosis, hepatitis B and C, HIV/AIDS, and syphilis. After three months on tofacitinib, the patient’s scalp pruritus resolved, and hair growth improved significantly [Figure 3].

- After 3 months of treatment, significant clinical improvement was observed.
Clinically, FAPD affects the androgen-dependent areas with sparing of the occipital scalp which is often misdiagnosed as AGA.1 Trichoscopy is helpful to distinguish FAPD from AGA and may help in selecting the biopsy site. Trichoscopic features of AGA can be seen in FAPD, such as hair diameter variability and the predominance of single HFs. Moreover, FAPD is characterised by the loss of HF ostia, perifollicular erythema, and perifollicular hyperkeratosis.1
Histopathologically, FAPD has overlapping features with AGA and lichen planopilaris (LPP). AGA is characterised by a progressive miniaturisation of HFs and mild, non-specific microinflammation.2 In contrast, FAPD is characterised by HF miniaturisation, perifollicular inflammatory infiltration, interface dermatitis involving the HF epithelium, and concentric perifollicular lamellar fibrosis.1 A comparison of FAPD and AGA is summarised in Table 1. So, it has been hypothesised that the pathogenesis of FAPD is the collapse of the HF bulge immune privilege, resulting in a lichenoid reaction caused by lymphocyte attack on the upper HF, leading to HF miniaturisation and fibrosis.3 Another alternate theory suggests that FAPD results from a lichenoid reaction in HFs induced by unknown antigenic stimulation in immunogenetically susceptible AGA patients.4,5
| Fibrosing Alopecia in a Pattern Distribution (FAPD) | Androgenetic Alopecia (AGA) | |
|---|---|---|
| Clinical Presentation |
|
|
| Trichoscopy |
|
|
| Histopathology |
|
|
In FAPD, the hair loss progression is slow and typically asymptomatic. Due to its insidious nature, patients with FAPD are often diagnosed at a late stage or misdiagnosed which seriously reduces the possibility of hair regeneration. To date, treatment options for FAPD have been reported in a few retrospective series and case reports. To our knowledge, treatments such as hair growth-promoting, anti-inflammatory, and anti-androgen agents can prevent the hair loss process of FAPD. However, no therapy has been shown to stimulate hair regrowth.3
Tofacitinib, a pan-JAK inhibitor drug, may be considered a potential therapeutic agent for FAPD. FAPD is regarded as a variant of LPP, and there is little evidence suggesting that tofacitinib can lead to measurable improvement in recalcitrant LPP.6 The JAK signalling pathway, crucial for cell proliferation, differentiation, and apoptosis and implicated in autoimmune and inflammatory diseases, may be key in FAPD’s pathogenesis.7 Its overactivity could undermine the hair follicle’s immune privilege and damage stem cells. We speculate that tofacitinib, by inhibiting JAK 1/2/3, may reduce immune and inflammatory reactions, thereby potentially aiding in the control of fibrosis in FAPD and promoting hair growth.
The treatment goal for FAPD is to prevent the destruction of follicles, arrest progression, and promote hair regrowth. Cicatricial alopecia if detected early, can have a better outcome with early reduction of the inflammatory response and slowing down of fibrosis This is the first case of oral tofacitinib in the treatment of FAPD which provides a new therapeutic strategy. More studies are required to assess its long-term benefit and safety profile.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Fibrosing alopecia in a pattern distribution. J Am Acad Dermatol. 2021;85:1557-64.
- [CrossRef] [PubMed] [Google Scholar]
- Androgenetic alopecia in males: A histopathological and ultrastructural study. J Cosmet Dermatol. 2009;8:83-91.
- [CrossRef] [PubMed] [Google Scholar]
- Clinicopathological characteristics and treatment outcomes of fibrosing alopecia in a pattern distribution: A retrospective cohort study. J Eur Acad Dermatol Venereol. 2021;35:2440-7.
- [CrossRef] [PubMed] [Google Scholar]
- Fibrosing alopecia in a pattern distribution: patterned lichen planopilaris or androgenetic alopecia with a lichenoid tissue reaction pattern? Arch Dermatol. 2000;136:205-11.
- [CrossRef] [PubMed] [Google Scholar]
- Is there a pathogenetic link between frontal fibrosing alopecia, androgenetic alopecia and fibrosing alopecia in a pattern distribution? J Eur Acad Dermatol Venereol. 2018;32:e218-e220.
- [CrossRef] [PubMed] [Google Scholar]
- Tofacitinib for the treatment of lichen planopilaris: A case series. Dermatol Ther. 2018;31:e12656.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Janus-kinase inhibitors in dermatology: A review of their use in psoriasis, vitiligo, systemic lupus erythematosus, hidradenitis suppurativa, dermatomyositis, lichen planus, lichen planopilaris, sarcoidosis and graft-versus-host disease. Indian J Dermatol Venereol Leprol. 2024;90:30-40.
- [CrossRef] [PubMed] [Google Scholar]





