Translate this page into:
Topical liposomal amphotericin B with surgical debridement in primary cutaneous mucormycosis
Corresponding author: Prof. Mala Bhalla, Department of Dermatology, Venereology and Leprosy, Government Medical College and Hospital, Chandigarh, India. malabhalla@yahoo.co.in
-
Received: ,
Accepted: ,
How to cite this article: Mittal R, Tuknayat A, Singla N, Bhagat R, Bhalla M. Topical liposomal amphotericin B with surgical debridement in primary cutaneous mucormycosis. Indian J Dermatol Venereol Leprol. doi: 10.25259/IJDVL_401_2024
Dear Editor,
Mucormycosis is a rare mycosis that has come under focus since the COVID-19 pandemic due to its emergence in patients who had diabetes and were administered steroids for severe acute respiratory syndrome Coronavirus 2 (SARS-CoV-2) infection.1,2 Cutaneous mucormycosis can be further classified in primary and secondary clinical forms.1,2 Primary cutaneous mucormycosis (PCM) may occur after traumatic fungal implantation or at catheter insertion sites and is associated with a good prognosis.1,2 Secondary cutaneous mucormycosis (SCM) occurs due to the spread from a distant inoculum and is usually associated with a worse prognosis.1,2
Mucormycosis in general, may be a predictor of the worst outcome; thus, a multimodal approach is recommended for its management. Surgical debridement remains the cornerstone of treatment to remove the necrotic contaminated tissue. Medical treatment modalities include systemically administered drugs like liposomal amphotericin-B, posaconazole, isavuconazole, etc.1,3 Treatment with liposomal amphotericin-B gel has been seldom reported in the treatment of cutaneous mucormycosis.4–6
A 73-year-old man presented to the dermatology outpatient department with multiple non-healing ulcers on his left thigh, knee, and leg, of a 6-months duration. The patient, a farmer, frequently experienced unnoticed trauma to his lower limbs from vegetative materials while working in the fields that usually healed within a week. However, six months ago, he developed an ulcer on the anterior aspect of his left knee that gradually increased in size. Two weeks later, several brown-black raised lesions appeared around the ulcer. These lesions spontaneously ruptured to form additional ulcers that continued to grow in size and number.
Cutaneous examination revealed bilateral pitting oedema and multiple ulcers on the left lower limb, extending from the mid-thigh to the ankle. The largest ulcer, located on the anterior aspect of the knee joint, was irregular, approximately 8x6 cm in size with well-defined margins, sloping edges, and necrotic purulent slough on the ulcer floor. Additionally, there were several other ulcers with similar morphology on the left thigh and leg, interspersed with areas of intact, atrophic skin [Figure 1]. The pulsations in the femoral and popliteal arteries were palpable, whereas posterior tibial and dorsalis pedis artery pulsations could not be felt because of the overlying pitting oedema. There was no regional lymphadenopathy. The right lower limb was normal, with normal arterial pulses.

- Multiple ulcers over the left lower limb extending from mid-thigh to ankle with intervening areas of intact, atrophic skin.
We considered the differential diagnoses of deep fungal infection, vasculitis, and pyoderma gangrenosum. The patient was subsequently investigated, and a potassium hydroxide wet mount revealed the presence of broad, aseptate fungal hyphae [Figure 2a]. Fungal culture demonstrated the growth of Rhizomucor species, identified morphologically as belonging to the mucormycetes group. On histopathology, dermis and subcutaneous tissue showed numerous foreign body giant cells along with moderate to dense mixed inflammatory cell infiltrate and the presence of broad, aseptate fungal hyphae that stained positive with Periodic acid-Schiff stain [Figures 2b and 2c], conforming to the diagnosis of mucormycosis. All other biochemical and haematological investigations and chest skiagram were within normal limits. A final diagnosis of primary cutaneous mucormycosis in an immunocompetent host was thus made and the patient was planned for surgical debridement and intravenous liposomal amphotericin B administration. However, because of the ongoing second wave of the COVID-19 pandemic, the intravenous amphotericin had to be deferred, and the patient was discharged after surgical debridement with the advice of daily dressing after the application of 0.1% liposomal amphotericin B gel once daily.
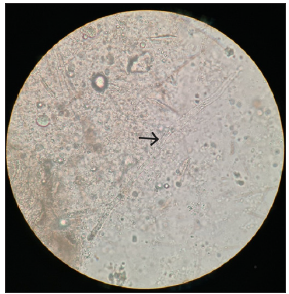
- Potassium hydroxide wet mount showed the presence of broad, aseptate fungal hyphae (black arrow). (KOH; 400x). (KOH: Potassium hydroxide).
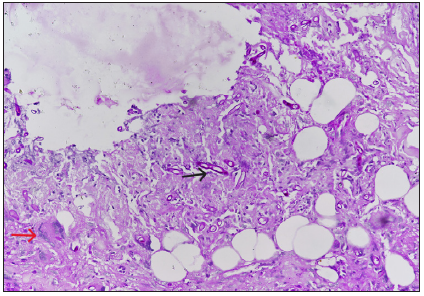
- On histopathology, dermis, and subcutaneous tissue showed numerous foreign body types of giant cells (red arrow) along with moderate to dense mixed inflammatory cell infiltrate and broad, aseptate fungal hyphae (black arrow). (Haematoxylin and Eosin; 400x).
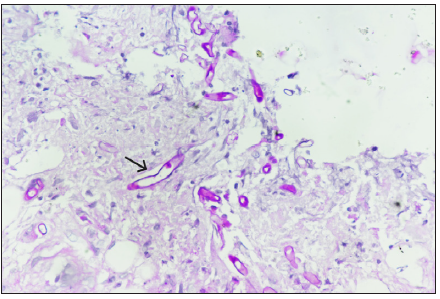
- Positive Periodic acid-Schiff stain conforming to the morphology of mucormycosis (black arrow). (Periodic acid schiff; 40x).
On subsequent follow-up, the patient showed marked improvement [Figures 3a and 3b]. Given the cost, increased side effects, and potential toxicity associated with intravenous liposomal amphotericin B and marked clinical improvement, the patient was continued on topical liposomal amphotericin B. Most of his lesions resolved completely within 15 weeks with areas of scarring [Figure 3c] and no recurrence at the 2-years follow-up.

- Healing ulcers with red granulation tissue at the base and sloping margins at 4 weeks.

- Healing ulcers with red granulation tissue at the base and sloping margins at 8 weeks.

- Complete resolution of ulcers at 15 weeks.
Depending on the agent, host, and environmental factors, cutaneous mucormycosis can have varied atypical clinical presentations.3 Thus, a high level of suspicion should be exercised.3 As per the available literature, topically applied amphotericin at a concentration of 50 mcg/mL exceeds the suggested epidemiological cut-off values (minimum inhibitory concentrations) to kill the organism at the site of pathology for the majority of Mucorales species (1–2 mcg/mL).4 Also, with the advent of technology, newer formulations of topical amphotericin, like liposomal nanoparticles with reduced molecular size, are available, enhancing the drug’s percutaneous absorption. In addition, amphotericin B applied topically to the debrided wound bypasses the need for absorption across the stratum corneum thus facilitating maximal tissue concentration.4,7
Surgical debridement and topical liposomal amphotericin B may be a viable therapeutic option in immunocompetent patients with localised cutaneous mucormycosis, given the high toxicity of systemic therapy, in selected patients.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that no artificial intelligence (AI)-assisted technology was used to assist in the writing or editing of the manuscript, and no images were manipulated using AI.
References
- Cutaneous mucormycosis: Mycological, clinical, and therapeutic aspects. Current Fungal Infection Reports. 2015;9:11.
- [CrossRef] [PubMed] [Google Scholar]
- Cutaneous mucormycosis. An Bras Dermatol. 2017;92:304-11.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Cutaneous mucormycosis: Report of five cases and review of the literature. J Plast Reconstr Aesthet Surg. 2009;62:434-41.
- [CrossRef] [PubMed] [Google Scholar]
- Use of topical amphotericin in a case of refractory sino-orbital angioinvasive mucormycosis. Med Mycol Case Rep. 2021;33:21-5.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- A case report: Utilization of topical amphotericin in postoperative mucormycosis. HCA Healthc J Med. 2021;2:187-9.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Mucomycosis in a severe trauma patient treated with a combination of systemic posaconazole and topical amphotericin B-case report. Antibiotics (Basel). 2023;12:1489.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Liposomal amphotericin B (AmBisome®): A review of the pharmacokinetics, pharmacodynamics, clinical experience, and future directions. Drugs. 2016;76:485-500.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]





