Translate this page into:
Topical steroids: Awareness and misuse among patients, pharmacists and general medical practitioner
Corresponding author: Dr. Pragya Ashok Nair, Department of Dermatology and Venereology, Pramukhswami Medical College, Karamsad - 388 325, Gujarat, India. drpragash2000@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Sheth NK, Nair PA. Topical steroids: Awareness and misuse among patients, pharmacists and general medical practitioner. Indian J Dermatol Venereol Leprol 2021;87:54-9.
Abstract
Aims and Objectives:
(1) To determine the level of awareness among patients, pharmacists and general practitioners about commonly available topical steroids and its combinations.(2) To determine the source of recommendation/prescription of topical steroids and its combination creams.(3) To know and create awareness about the side effects of topical steroids in all the study groups.
Methods:
This was a prospective questionnaire-based study where three study groups, namely patients, pharmacists and general practitioners, were included. This study was approved by the institutional ethics committee. after ethical clearance. The patients who used topical steroids for dermatoses where it is an absolute contraindication, as well as those who developed side effects, were included in the study. ThoroughComplete cutaneous examination was done specifically to detect the side effects of steroids. Seminars were conducted and questionnaires were given to both the pharmacists and general practitioners of nearby areas. The questionnaire consisted of questions regarding their prescription and dispensing practices of topical steroids and its combinations.
Results:
Out of 95 patients seen, the most commonly used steroid molecule was clobetasol propionate 0.05% in 44 (46.3%) patients, the common source of recommendation was general practitioners in 36 (37.8%), the common indication was superficial dermatophytosis in 85 (89%) and the most common adverse effect was recurrence/increase in the extent of the infection in 72 (75.78%) patients. Out of total 44 general practitioners enrolled in the study, 22 (50%) were qualified allopathic medical practitioners and22 (50%) were homeopathic/ayurvedic doctors. Superficial dermatophytosis [19 (43.18%)] was the common dermatosis seen by them. While 29 (65.90%) preferred prescribing topical steroids or its combination, rest of them preferred plain steroid creams. Out of 179 pharmacists, 74 (41.34%) did not have appropriate knowledge of topical steroids, 35 (19.55%) were not aware that steroids are isschedule “H” drugs. Commonest molecule sold over the counterwas clobetasol propionate 0.05% by 74 (41.89%). The limitations of our study were small study group and short duration.
Conclusion:
As dermatologists, it is our responsibility, to correctly educate the society, particularly the non-dermatologist medical fraternity, about ethical and rational use of topical steroids.
Keywords
Clobetasol propionate
dermatophytosis
topical steroids
Introduction
Topical steroids have greatly contributed to the dermatologist’s ability to effectively treat several difficult dermatoses. The available range of formulations and potency gives a dermatologist the flexibility to treat all group of patients, different phases of disease and different anatomic sites. Using them, it has become easy to treat several dermatoses which otherwise were the cause of significant morbidity. This euphoria was lapped up by the pharmaceutical companies. The availability of wide variety of steroids proved to be a source of harm to dermatologists and after the initial honeymoon period the side effects of the drugs gradually became discernable.1 Apart from the well-known indications such as psoriasis, atopic dermatitis, vitiligo, lichen planus, lichen simplex chronicus and discoid lupus erythematosus, topical steroids are being used for conditions such as acne, melasma, urticaria and even undiagnosed skin rash by dermatologists and even general practitioners.2 Topical steroids are highly susceptible to misuse by patients, pharmacists and physicians themselves as shown by several studies.3-5 If not properly counseled, patients may not return for a follow-up and may continue to use the topical steroids for prolonged period. Such improper use can have devastating consequences, both local and systemic, in the long run.6 The responsibility lies with dermatologists, as these drugs are a strong weapon to fight against many skin diseases. We need to correctly educate the society, including the non-dermatologist medical fraternity, about ethical and rational use of topical steroids.
Aims and objectives
To determine the awareness among outpatient department patients, pharmacists and general practitioners (MBBS, Ayurvedic and Homeopathic) about commonly available topical steroids and its combinations and their side-effects
To find the source of recommendation/prescription of topical steroids and its combinations which will help to sensitize, counsel and educate patients regarding its proper use
To create the awareness about side effects of topical steroids in pharmacists and medical practitioners.
Methods
This was a prospective questionnaire-based study that included three study groups, namely patients, pharmacists and general medical practitioners (MBBS/Ayurvedic/Homeopaths). The study enrolled patients coming to dermatology outpatient department at Shri Krishna Hospital, Karamsad over a period of 3 months from May 2017 to July 2017 after clearance from institutional ethics committee. Only those patients were selected who had:
Brought the sample of the steroid/steroid combination cream they had used
History of topical steroid abuse in dermatological conditions where steroids are contraindicated or if indicated, the dose, frequency of application and/or the duration of application was not appropriate
Presented with at least one of the following adverse effects as chief complaint: steroid induced or aggravated acne or acneiform eruption, facial hypertrichosis, plethoric face and telangiectasia, cutaneous atrophy, striae, hyper/hypopigmentation, tinea incognito or steroid modified tinea, perioral dermatitis, infantile, gluteal granuloma and pyoderma.
The second group included pharmacists who either practice in an institution or have private clinics. The third group included general practitioners (MBBS, ayurvedic and homeopathy practitioners) practicing in nearby locality. The study excluded those patients who used topical steroids for dermatosis where they were first line of treatment and did not develop any steroid-induced skin conditions. Systemic adverse effects due to topical steroids were also excluded. Patients were interviewed using a detailed pre-validaged self-designed questionnaire after informed, written and valid consent. The questionnaire covered their personal details, indications, duration and frequency of application of topical steroids. They were also asked about who had prescribed/ recommended the treatment. A full skin examination was performed to detect any dermatosis related with the abuse of topical steroids. Most of the diagnoses were exclusively clinical. In suspected cases of dermatophytosis, potassium hydroxide mount of skin scrapings was done which was then examined for presence of fungal hyphae microscopically. Patients were advised to avoid any kind of self-medication and counseled to continue 4–6 weeks treatment for fungal infection.
The other two groups were also analyzed based on self- designed questionnaires. Health seminars using audio–visual lectures were conducted for each study group and all the participants were educated regarding common aspects of topical steroid abuse.
Results
Out of the 95 new patients seen during the study period, the most common steroid molecule used by 44 (46.3%) patients was clobetasol propionate 0.05% [Table 1]. Most 50 (50.6%) patients had used steroid cream for 1–1.5 months duration. Ninety-three (97.9%) patients had no idea about the adverse effects of topical steroids and 93 (97.9%) had not read the leaflet provided by the manufacturer. None of the patients knew the dosage, i.e. how much of the drug had to be used per body surface area. The number of applications varied from once daily to 3–4 times a day. Topical steroid creams were recommended by friends to 25 (26.30%) and by family members to 6 (6.31%) patients respectively [Table 1].The most common adverse effect seen in the study was either recurrent dermatophytosis or aggravation of inflammatory symptoms along with steroid modified picture in 72 (75.78%) patients [Figure 1a-c, Figure 2].
| Parameter | Number of patients (n=95) |
|---|---|
| Steroid molecule used | |
| Clobetasol propionate 0.05% | 44 (46.3) |
| Beclomethasone dipropionate 0.12% | 16 (16.84) |
| Betamethasone valerate 0.05% | 16 (16.84) |
| Mometasone furoate 0.1% | 7 (7.36) |
| Flucinolone acetonide 0.005% | 6 (6.31) |
| Hydrocortisone 1% | 3 (3.1) |
| Halobetasol propionate 0.05% | 3 (3.1) |
| Source of recommendation | |
| General medical practitioners | 36 (37.8) |
| Friends | 25 (26.3) |
| Pharmacists | 25 (26.3) |
| Family members | 6 (6.31) |
| Dermatologists | 3 (3.1) |
| Dermatosis for which steroid was used | |
| Superficial dermatophytosis | 85 (89) |
| Urticaria | 2 (2.10) |
| Itching | 2 (2.10) |
| Fixed drug reaction | 2 (2.10) |
| Acquired ichthyosis | 1 (1.05) |
| Melasma | 1 (1.05) |
| Herpes zoster | 1 (1.05) |
| Folliculitis | 1 (1.05) |
| Dermatological adverse effect | |
| Recurrent dermatophytosis/steroid modified tinea/tinea incognito | 72 (75.78) |
| Steroid induced hypopigmentation | 16 (16.84) |
| Acneform eruption | 2 (2.10) |
| Allergic contact dermatitis (due to steroid molecule or the preservative content) (patch test not performed) [Figure 2] | 4 (4.21) |
| Purpura | 1 (1.05) |
| Duration of usage (months) | |
| <1 | 50 (52.6) |
| 1-3 | 20 (21.05) |
| 3-6 | 19 (20) |
| >6 | 6 (6.3) |
| Number of total applications/day(times/day) | |
| 1-2 | 67 (70.5) |
| 2-3 | 24 (25.2) |
| >3 | 4 (4.2) |
| Not read the instruction leaflet provided with the topical preparation | 93 (97.8) |
| No idea about adverse effect of topical steroids | 93 (97.9) |
| Recommended the creams used by them to other family members | 16 (16.84) |

- Tinea faciei

- Recurrent dermatophytosis
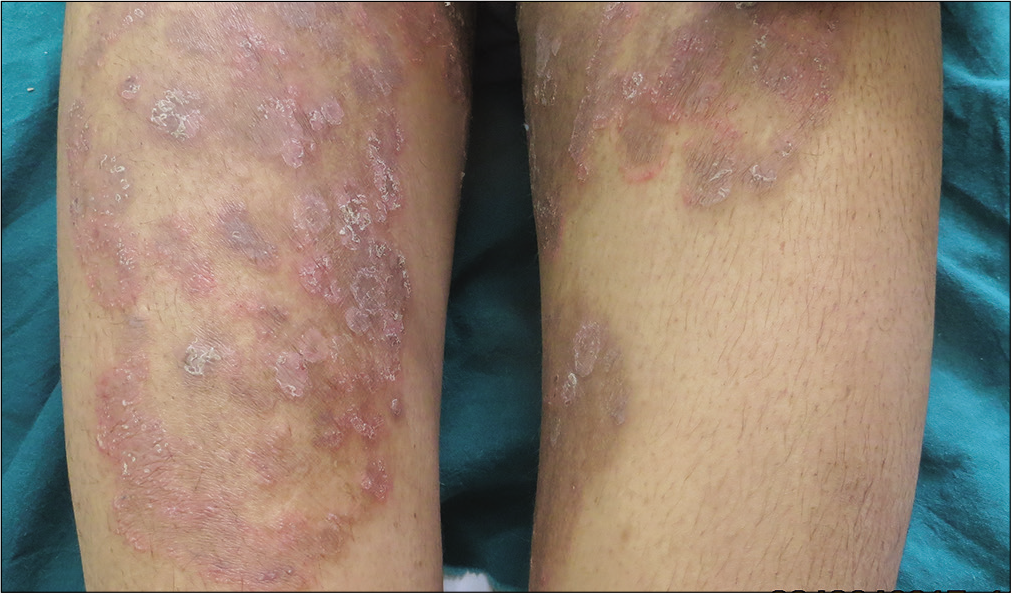
- Tinea incognito
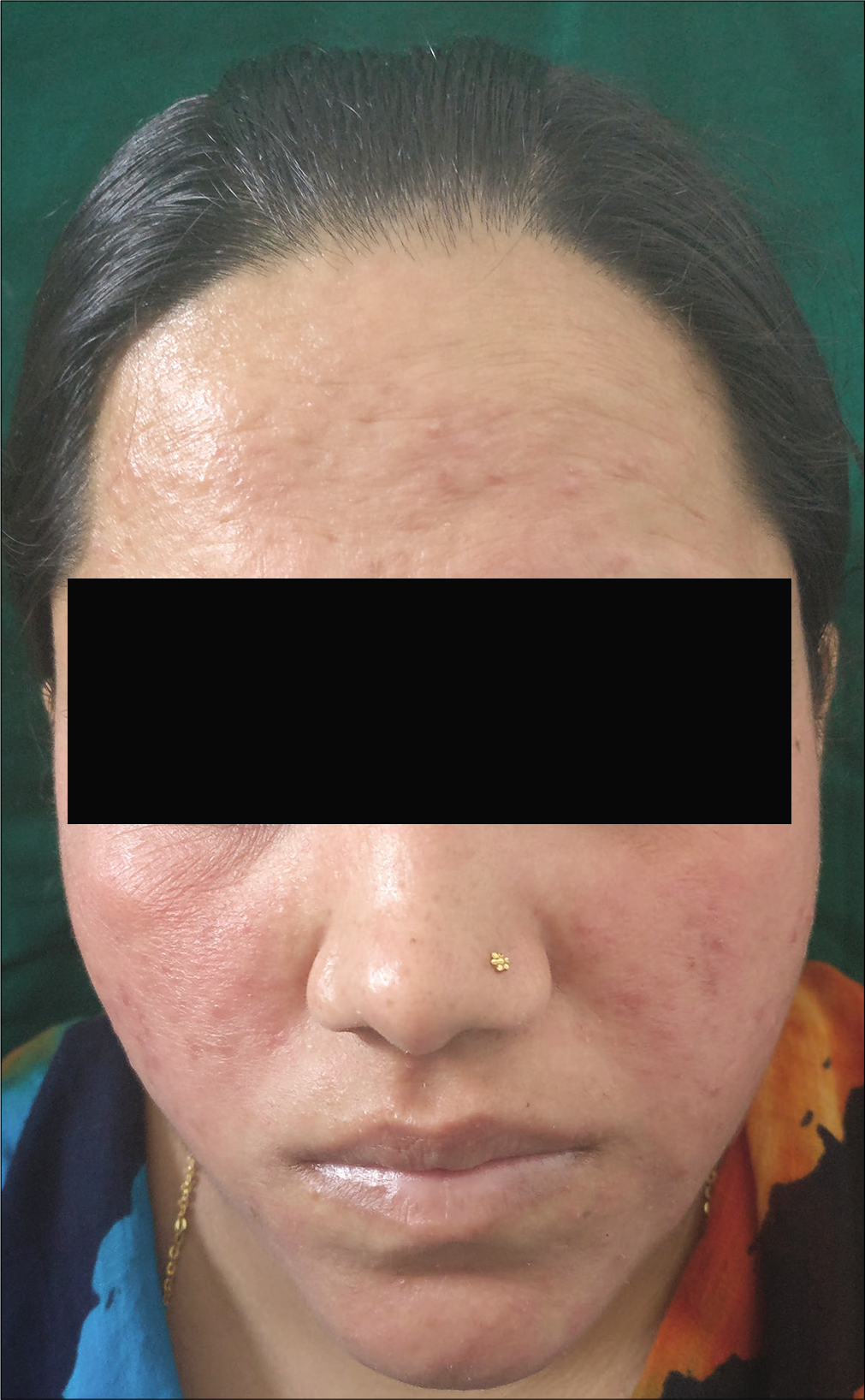
- Contact irritant dermatitis on face
Out of 44 general practitioners enrolled in the study, 22 (50%) were qualified medical practitioners and 22 (50%) were homeopathic or ayurvedic practitioners. The average number of patients with skin diseases seen by them per day was around 30%.Three (6.81%) practitioners were unable to tell skin condition they come across during their consultation, indicating that they are not familiar with dermatological conditions but are still prescribing topical steroids. Combination creams were preferred by 29 (65.90%) general practitioners, while 15 (34.09%) preferred prescribing plain steroid creams. Out of 29 prescribing topical steroids in combination, 18 were homeopathic/ayurvedic practitioners and 11 were MBBS doctors. Out of 15 practitioners prescribing plain steroid molecule, 11 were MBBS doctors and four were homeopathic/ayurvedic practitioners. The most common dermatosis for which topical steroid was prescribed was superficial dermatophytosis 19 (43.18%) [Table 2]. Almost half of the practitioners 23 (52.27%) did not have any knowledge regarding the adverse effects of topical steroids, of which eight were MBBS doctors and 15 were homeopathic/ ayurvedic practitioners.
| Parameter | Number of general medical practitioners (n=44), n (%) |
|---|---|
| Qualification of the practitioner | |
| MBBS | 22 (50) |
| Homeopathic/ayurvedic | 22 (50) |
| Steroid molecule prescribed | |
| MBBS (n=22) | |
| Clobetasol | 9 (40.90) |
| Betamethasone | 6 (27.27) |
| Fluticasone | 4 (18.18) |
| Beclomethasone | 3 (13.63) |
| Homeopathic/ayurvedic practitioners (n=22) | |
| Clobetasol | 9 (40.90) |
| Betamethasone | 7 (31.81) |
| Beclomethasone | 5 (22.72) |
| Fluticasone | 1 (4.54) |
| Dermatosis for which topical steroid was prescribed | |
| Superficial dermatophytosis | 19 (43.18) |
| Eczema | 18 (40.90) |
| Facial dermatosis/fairness | 4 (9.09) |
| Undiagnosed dermatosis | 3 (6.81) |
| Preferred giving combination steroidpreparation | 29 (65.90) |
| MBBS | 18 (40.9) |
| Ayurvedic/homeopathic | 11 (25) |
| Preferred giving plain steroid preparation | 15 (34.09) |
| MBBS | 11 |
| Ayurvedic/homeopathic | 4 |
| Did not have knowledge regarding adverse effect of topical steroids | 23 (52.27) |
| MBBS | 8 |
| Ayurvedic/homeopathic | 15 |
Out of 179 pharmacists enrolled in the study, 74 (41.34%) did not have knowledge regarding adverse effects of topical steroids, and 35 (19.55%) did not know that it is a schedule “H” drug. An important highlight of the study was that all the pharmacists in the study sold steroid and steroid combination creams over the counter. The most common indication for which topical steroids were recommended and sold was for dermatosis involving the extremities and trunk, 76 (43.01%), followed by cosmetic and fairness purpose, 60 (34.07%) [Table 3]. Forty-four pharmacists (25.13%) were recommending topical steroids to their friends and family members. The common molecule sold was clobetasol propionate 0.05%74 (41.89%), though it was not clear as to whether it was sold as a plain drug or as combination cream [Table 3].
| Parameter | Number of pharmacists (n=179), n (%) |
|---|---|
| No knowledge regarding topical steroids | 74 (41.34) |
| Did not know that topical steroids are schedule H drug | 35 (19.55) |
| Indication for which topical steroid was sold | |
| Dermatosis on extremities or trunk | 76 (43.01) |
| Cosmetic or fairness purpose | 60 (34.07) |
| Facial dermatoses | 40 (22.90) |
| Not able to answer | 3 (1.67) |
| Steroid molecule sold | |
| Clobetasol | 74 (41.89) |
| Betamethasone | 73 (40.78) |
| Mometasone | 13 (7.2) |
| Beclomethasone | 12 (6.7) |
| Fluticasone | 4 (2.23) |
| Hydrocortisone | 3 (1.67) |
| Recommending steroids to friends and family members | 44 (25.13) |
Discussion
Topical steroids are among the most commonly used medications in dermatology clinics. They are highly efficacious drugs used for the treatment of varied autoimmune and inflammatory dermatological conditions for their anti-inflammatory, antiproliferative and immunosuppressive properties.7 However, several factors must be considered before the drug is prescribed, such as (a) the site of application, (b) the potency of the drug, (c) age of the patient, (d) duration of application and (e) indication for usage. Faltering on any of these counts can lead to its misuse. Application of potent or highly potent topical steroids in children, on the face or for prolonged duration would lead to disastrous consequences.6 Prescription of topical steroids has become ubiquitous with dermatologists and concerns have also been raised regarding its misuse for off-label indications. Side effects of topical steroids may vary from local effects, such as atrophy, striae, telangiectasia, hypertrichosis and acneiform eruptions to more serious systemic side effects due to hypothalamo-pituitary axis suppression. An upcoming latest trend that has been noticed is the rise in the superficial dermatophytosis. The abuse of topical steroids for the treatment of superficial dermatophytosis is thought to be one of the major contributory factors to this menace. Most of the patients blindly follow advertisements on television which misguide them, and thus they clinically present with tinea incognito or steroid modified tinea. The easy availability of topical steroids creams over the counter at the pharmacy stores and the practice of Indian chemists to dispense these drugs without prescription or multiple refills on the same prescription has led to its misuse by the community. The concern which is even more serious is its inappropriate use in conditions such as acne, bacterial and fungal infections, undiagnosed skin rash and as fairness cream by nonregistered practitioners, on advice of pharmacist at chemist shops or recommended by friends and family members. There is a tendency to reuse old prescription for recurrent or new lesion. Prescription sharing with relatives and friends on the presumption that similar-looking skin problems can be self-treated by simple prescription copying is also common.
Apart from its anti-inflammatory effect, topical steroids also have potent anti-pruritic, atrophogenic, melanopenic, sex-hormone like and immunosuppressive effects on the skin, leading to significant local adverse effects which are directly related to its potency.
There are studies which have tried to highlight the various side effects and harm caused by misuse of topical steroids and its combinations. These studies have tried to bring to the notice of regulatory authorities about the damage caused by the free availability of these creams. One of the new emerging concerns is its use as fairness cream.
A comparison of our study with other similar studies has been shown in Table 4.4,8-11 Interestingly, in our study, 85% patients used topical steroid cream for superficial fungal infection and the most common molecule used was clobetasol propionate 0.05% in 46.3% patients, followed by beclomethasone dipropionate 0.12% and betamethasone valerate 0.05% in 16.84% patients each. This indicates the about free and easy availability of these drugs over the counter. Recurrent fungal infection and aggravation of symptoms was the most common adverse effect, seen in our study due to repeated use of steroids. Lack of knowledge about the disease and the molecule use resulted in chronic use of these drugs by patients. This is one of the cause of the alarming scenario of fungal resistance, as an epidemic in the community. Because the rational treatment with antifungals runs a prolonged course of 4–6 weeks, compliance is also a factor that drives the patients toward seeking a quick cure but at the same time resulting in resistance. Resistant superficial dermatophytosis is now seen as the tip of an iceberg where majority of the causes lie underneath and cannot be identified with topical steroids abuse being one. Our study thus tries to highlight the magnitude of this problem that has now become probably the root cause of widespread resistance.
| Parameter | Rathod et al.8 | Nagesh and Akhilesh9 | Dey10 | Jha et al.11 | Saraswat et al.4 Multicentric |
Our study |
|---|---|---|---|---|---|---|
| Year | 2011 | 2016 | 2010-2011 | 2013-2014 | 2008 | 2017 |
| Study period | 2 months | - | 1 year | 1 year | 4 months | 3 months |
| Total number of patients | 142 prescriptions containing topical steroids | n=1000 | n=379 | n=410 | n=433 | n=95 |
| Total number of pharmacists | - | - | - | - | - | n=179 |
| Total number of GPs | - | - | - | - | - | n=44 |
| M/C steroid molecule of abuse | Fluocinolone-acetonide | Betamethasone: 77.6% | Mixed: 39.84% | Betamethasone valerate: 20.4% | Betamethasone valerate: 58.9% | Clobetasol propionate: 46.3% |
| Duration of use | Not specified in prescriptions | Variable | - | - | Variable | <1 month |
| M/C indication for use | Not mentioned in 85% prescriptions | Acne: 30.2% | Fairness: 50.39% | Fairness: 35.6% | Fairness/general face cream: 29% | Superficial dermatophytosis |
| M/C source of recommendation | Dermatologists | GPs: 49.5% | Pharmacists: 35.36% | Pharmacists: 42.9% | Nonphysicians: 59.3% | GPs: 37.8% |
| M/C adverse effect | - | Aggravation of symptoms: 40% | Facial acne: 37.99% | Acne: 42.9% | Acne: 57.5% | Aggravation of symptoms and extension of infection: 73.6% |
M/C: Most common, GP: General practitioner
The pharmacists were unable to answer the source of prescription of topical steroids or its combination. It indicates that either these drugs are sold without any legal prescription by general practitioners or sold on older prescriptions. Almost 19.55% pharmacists did not know that topical steroids are schedule H drugs. According to the pharmacists in this study, the second most common indication for which patients (34.07%) used steroid cream was for fairness purpose. This shows the level of misuse of these drugs among pharmacists to earn benefits and blind faith of the community on television advertisements.
Another highlight of our study was the lack of awareness regarding steroids in medical practitioners. The most common steroid molecule prescribed by general practitioners, was clobetasol propionate 0,05% (40.90%), while superficial dermatophytosis (43.18%) was the most common indication for which it was given. This shows how the medical fraternity lacks awareness about the use of topical steroids and the basic knowledge about common skin diseases.
Hence the three factors that contribute to antifungal resistance in the community are: patients unaware of side effects of topical steroids, pharmacists selling over the counter drugs without proper prescription and the general practitioners who lack basic knowledge about common skin diseases. Thus, we have compiled all these three in a single study to highlight the missing links that prevail at various levels.
Conclusion
Dermatologists need to take keen interest in creating awareness among patients about the use of topical steroids, counseling them for proper follow-up and avoid self-medication. The government should take strict actions against unlawful sale of the topical steroid creams. More and more health education seminars are required to be conducted for the pharmacists and the general practitioners to create awareness regarding safe use of topical steroids. Proper follow-up of patients to whom steroids have been prescribed is needed. Counselling them to avoid self-medication should be done.
The limitation of our study was small study population and short duration. More studies, preferably multicentric, especially covering the pharmacists, general practitioners and the patients in large numbers need to be conducted.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Atrophic striae in patients with inguinal intertrigo. Arch Dermatol. 1963;87:450-7.
- [CrossRef] [Google Scholar]
- Abuse of topical steroid as cosmetic cream: A social background of steroid dermatitis. Indian J Dermatol. 2006;51:154-5.
- [CrossRef] [Google Scholar]
- Topical corticosteroid abuse on the face: A prospective, multicenter study of dermatology outpatients. Indian J Dermatol Venereol Leprol. 2011;77:160-6.
- [CrossRef] [PubMed] [Google Scholar]
- Steroid-induced rosacea-like dermatitis: Case report and review of the literature. Cutis. 2009;83:198-204.
- [Google Scholar]
- Guidelines of care for the use of topical glucocorticosteroids, American Academy of Dermatology. J Am Acad Dermatol. 1996;35:615-9.
- [CrossRef] [Google Scholar]
- Abuse of topical corticosteroids in India: Concerns and the way forward. J Pharmacol Pharmacother. 2016;7:1-5.
- [CrossRef] [PubMed] [Google Scholar]
- Prescribing practices of topical corticosteroids in the outpatient dermatology department of a rural tertiary care teaching hospital. Indian J Dermatol. 2013;58:342-5.
- [CrossRef] [PubMed] [Google Scholar]
- Topical steroid awareness and abuse: Aprospective study among dermatology outpatients. Indian J Dermatol. 2016;61:618-21.
- [CrossRef] [PubMed] [Google Scholar]
- Misuse of topical corticosteroids: A clinical study of adverse effects. Indian Dermatol Online J. 2014;5:436-40.
- [CrossRef] [PubMed] [Google Scholar]
- Misuse of topical corticosteroids on the face: A cross-sectional study among dermatology outpatients. Indian Dermatol Online J. 2016;7:259-63.
- [CrossRef] [PubMed] [Google Scholar]






