Translate this page into:
Total serum IgE level in patients of dermatophytosis and its association with various clinical parameters
Corresponding author: Dr. Jignaben Krunal Padhiyar, Department of Dermatology, Venereology and Leprosy, GCS Medical College Hospital and Research Institute, Opp. DRM Office, Near Chamunda Bridge, Ahmedabad - 380 025, Gujarat, India. dr.jignapadhiyar@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Patel NH, Padhiyar JK, Singh R, Patel T. Total serum IgE level in patients of dermatophytosis and its association with various clinical parameters: A study from tertiary care institute. Indian J Dermatol Venereol Leprol 2021;87:290-2.
Sir,
A tremendous increase in the number of cases of dermatophytosis has been observed in India in the last 5 years. Though community-level prevalence is not exactly known, multiple studies have observed an increase in number at tertiary care hospitals. A noteworthy feature of the current epidemic of dermatophytosis in India is the increased number of chronic cases, frequent relapses, and involvement of multiple family members. Though multiple aspects of the present epidemic like the species of fungi and increase in minimal inhibitory concentration to various antifungals have been studied and published by various authors, not much has been published regarding the host immune response to dermatophytes from India.
A detailed and elaborate review on dermatophytosis and host immune interaction was published by Woodfolk in 2005.1 Three distinct types of host immune response were noted after colonization with Trichophyton, which is depicted in Figure 1. Immediate hypersensitivity response to dermatophytosis bears the hallmark of Th2 response in terms of the presence of serum IgE and IgG4 antibodies against Trichophyton antigens. By contrast, delayed-type hypersensitivity is a form of cell-mediated immunity in which the ultimate effector cell is the activated macrophage, mediated by gamma interferon (IFN- γ) secreting CD4+ T lymphocytes (Th1 response). Delayed type hypersensitivity response to Trichophyton extract is associated with lower titers of IgG antibodies to Trichophyton antigens and no IgE or IgG4.2,3 Immediate hypersensitivity is frequently associated with chronic non-inflammatory dermatophytosis; indeed, delayed type hypersensitivity is often absent despite persistent and widespread infection in some individuals. Whether chronic infection results from lack of delayed-type hypersensitivity or presence of immediate hypersensitivity, is yet not fully known. Balogh et al. published a study where they observed higher levels of serum IgE in patients of chronic dermatophytosis, associated with lower number of circulating T cells and increased rate of immediate hypersensitivity reaction to intradermal trichophytin test.4
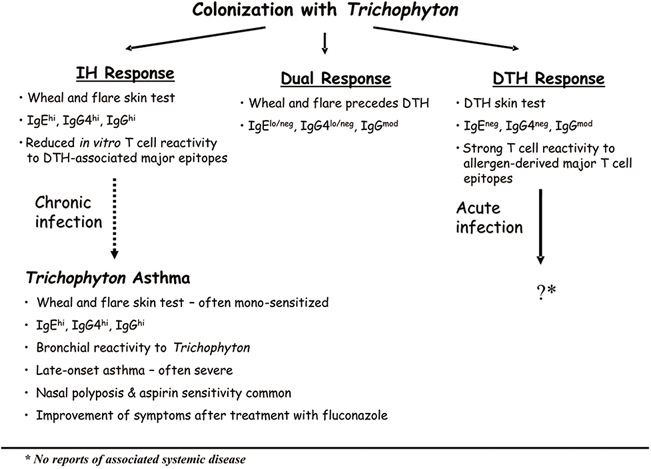
- Immune response subsequent to colonization with Trichophyton, IH: Immediate Hypersensitivity, DTH: Delayed hypersensitivity1
With the above background, we decided to conduct a study to measure the total serum IgE levels in patients of dermatophytosis and assess correlation with various clinical parameters. After ethics committee approval and written consent, 120 patients who presented for the first time to the skin department of GCS medical college, Ahmedabad, with a clinical diagnosis of dermatophytosis involving non-glabrous skin (excluding T. capitis and onychomycosis) showing the presence of fungus on microscopy of skin scrapings mounted with potassium hydroxide, were screened for the study. Thirty-three patients having one or more exclusion criteria like pregnancy, lactation, past or present atopic illness, any medical or surgical comorbidities, and patients having secondary bacterial infections were excluded from the study, remaining 87 patients were enrolled in the study.
In addition to screening hematological and biochemical investigations, quantitative assessment of serum IgE was performed using chemiluminescent immunoassay using Elecsys© and Cobase Analyser (Roch Diagnostic); where normal laboratory reference value for total serum IgE for a healthy adult was 0 to 240 ng/mL. Epidemiological data like age, sex and presence of family history were collected. Clinical parameters like body surface area involvement using the rule of nine, site of involvement, duration of disease, morphological presentation, history of use of topical, oral and injectable steroids were evaluated. Chronic dermatophytosis was defined as the as dermatophytosis in a patient of more than 6 months duration, with or without recurrence, in spite of being treated. Dermatophytosis was considered to be recurrent when there was re-occurrence of the disease (lesions) within less than 6 weeks after completion of the treatment.5 Less than 6 week clinical remission between recurrence in old lesion or appearance of new lesions was recorded as continuous disease period, relapse beyond 6 week was recorded as new episode of dermatophytosis and duration of that particular episode was captured. Intensity of itch was recorded in patient-reported scale (0 = no itching, 1 = mild itching, 2 = moderate itching, 3 = severe itching.).
Out of the total 87 patients enrolled in this study, with ages ranging from 18 to 64 years (mean age-32.7 years, SD 11.8 years) male to female ratio stood at 2.2:1, in favor of males. Out of the total 87 patients studied, only 10 had total serum IgE levels within the normal laboratory range, rest 77 (88.05%) had high IgE levels. We also observed that 57.4% (n = 50) of the patients had total serum IgE levels four times above the normal laboratory reference range. Eleven patients in the study (12.6%) had IgE levels equal to or above 6000 ng/ml, which was the highest measurable range for undiluted serum. The mean serum IgE levels in males compared to female subjects were significantly higher (mean in males = 2126.6; mean in females = 1226.7;P = 0.04).
Table 1 shows the association of serum IgE levels with various clinical parameters. Figure 2 shows the correlation of serum IgE with the body surface area involved. Figure 3 shows the correlation of serum IgE with the duration of the disease.
| Variable | Response | n | Median | Range | P |
|---|---|---|---|---|---|
| Use of topical steroid | Yes | 32 | 1107.0 | 71.0-6000.0 | 0.552 |
| No | 55 | 1133.0 | 102.0-6000.0 | ||
| Use of oral steroid | Yes | 29 | 1751.0 | 198.0-6000.0 | 0.040 |
| No | 58 | 1006.5 | 71.0-6000.0 | ||
| Patient reported itch severity | Mild | 10 | 1034.5 | 243.0-1751.0 | 0.683 |
| Moderate | 42 | 1000.5 | 71.0-6000.0 | ||
| Sever | 34 | 1151.0 | 110.0-6000.0 | ||
| Family member involvement | Yes | 49 | 1038.0 | 71.0-6000.0 | 0.401 |
| No | 38 | 1204.0 | 102.0-6000.0 | ||
| Number of anatomical sites | Single | 37 | 911.0 | 71.0-6000.0 | 0.169 |
| More than one | 50 | 1172.0 | 111.0-6000.0 | ||
| Prior use of topical antifungal | Yes | 32 | 1212.0 | 110.0-6000.0 | 0.088 |
| No | 55 | 965.0 | 71.0-6000.0 |
Detailed statistical analysis using Mann-Whitney U test of association of serum IgE level with various parameters
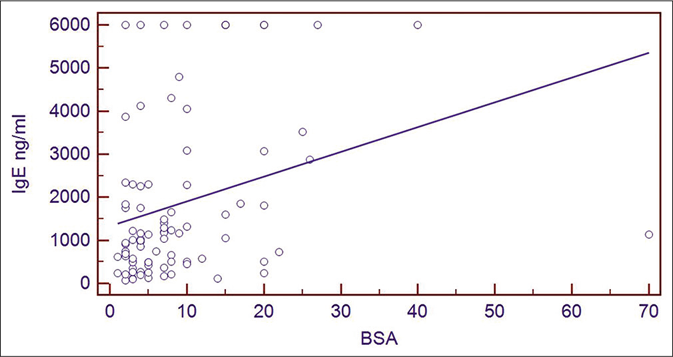
- Scatter diagram depicting association of body surface area with total serum IgE levels (r = 0.345, P = 0.001, n = 87 Spearman’s rho)
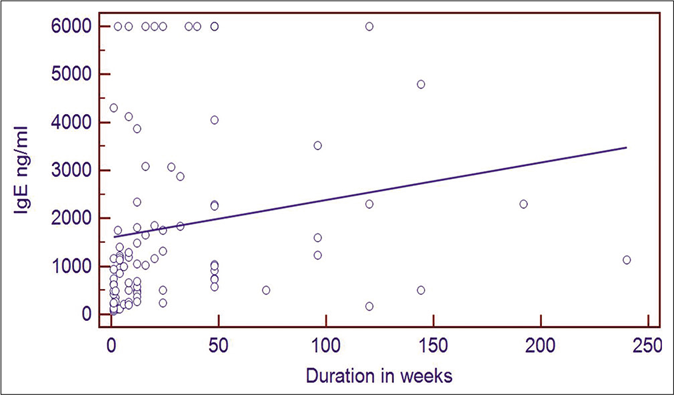
- Scatter diagram depicting association of duration of diseases (weeks) with total serum IgE levels (r = 0.433, P = 0.0001, n = 87 Spearman’s rho)
With the present epidemic of dermatophytosis in India, not only there is an increased incidence of cases, but also these are characterized by chronicity, recalcitrant disease, frequent relapses, wide-spread skin lesions and involvement of multiple family members. For effective eradication of any infection along with appropriate antifungal medication, intact host immune response is equally important.
Defense against dermatophytes depends on both innate and acquired immune mechanisms.6 The presence of elevated IgE in particular, is associated with chronicity.7 In our study, we observed elevated total serum IgE levels in 88.5% of the patients which is in agreement with another recent study from India by Tigga et al. which showed 77% patients having higher IgE levels.8 Multiple studies on chronic dermatophytosis have observed that localization of host immune response to the humoral arm is an important determinant of chronicity.9-11 Our study also showed a strong correlation between the duration of disease and serum IgE levels. The second significant observation of higher IgE levels seen with greater extent of body surface area involvement can also be attributed to the absent or incomplete cell-mediated immune response which is a pre-requisite for restricting the infection at the site of inoculation. In our study, we did not observe any strong correlation between serum IgE levels and the severity of itching, but this aspect needs to be tested in studies with bigger sample sizes. We compared the serum IgE levels in those patients who had used topical steroids versus those who had never used topical steroids and the difference was insignificant. The role of initial exposure to topical or systemic steroids after infection in preventing the development of cell mediated immune response, which eventually evolves into ineffective humoral type, requires further investigation in an Indian context. Studies specifically designed for investigating the effect of steroid exposure on serum IgE levels in patients of dermatophytosis are needed. However, this kind of study is likely to face ethical hurdles as topical or systemic steroids are not recommended treatment for dermatophytosis.
Our study had certain limitations being that-total serum IgE can only be considered a surrogate biomarker of humoral immune response to Trichophyton antigen; further studies using Trichophyton specific IgE and other biomarkers for cell-mediated immunity and humoral immunity (like IL4 and INF-gamma) can throw more light on this less explored aspect of dermatophytosis in India. Additionally, case-control studies with carefully selected, matched controls would be helpful in validating the findings. Detailed analysis of the effect of topical corticosteroid usage on immune response to dermatophytes using multiple biomarkers of immunity and comparative study between steroid-naive and treated patients is also warranted.
To conclude, total serum IgE levels maybe considered a marker of humoral immune response against dermatophyte infection. We found a significant correlation between total serum IgE, duration of disease, and the extent of body surface area involvement in dermatophytosis.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Trichophyton tonsurans allergen, I. Characterization of a protein that causes immediate but not delayed hypersensitivity. J Immunol. 1991;147:96-101.
- [Google Scholar]
- Definition of a Trichophyton protein associated with delayed hypersensitivity in humans: Evidence for immediate (IgE and IgG4) and delayed type hypersensitivity to a single protein. J Immunol. 1996;156:1695-1701.
- [Google Scholar]
- Serum IgE level and T-cell count in chronic dermatophytosis. Mykosen. 1981;24:84-9.
- [CrossRef] [PubMed] [Google Scholar]
- Expert consensus on the management of dermatophytosis in India (ECTODERM India) BMC Dermatol. 2018;18:6.
- [CrossRef] [PubMed] [Google Scholar]
- Fungal infections In: Griffiths C, Barker J, Bleiker T, Chalmers R, Creamer D, eds. Rook's Textbook of Dermatology (9th ed). Chichester: Wiley Blackwell; 2016. p. :32-21.
- [Google Scholar]
- Immune responses of patients with tinea imbricata. Br J Dermatol. 1983;108:581-9.
- [CrossRef] [PubMed] [Google Scholar]
- Burden of chronic dermatophytosis in a tertiary care hospital: Interaction of fungal virulence and host immunity. Mycopathologia. 2018;183:951-9.
- [CrossRef] [PubMed] [Google Scholar]
- Immediate hypersensitivity and serum IgE antibody responses in patients with dermatophytosis. Asian Pac J Allergy Immunol. 2012;30:40-7.
- [Google Scholar]
- Failure of treatment in chronic dermatophyte infections. Postgrad Med J. 1979;55:608-10.
- [CrossRef] [PubMed] [Google Scholar]





