Translate this page into:
Traction alopecia secondary to obsessive-compulsive disorder
Corresponding author: Hicran Dogru, Assistant Professor, Department of Child and Adolescent Psychiatry, Atatürk University School of Medicine, Erzurum, Turkey.
-
Received: ,
Accepted: ,
How to cite this article: Dogru H. Traction alopecia secondary to obsessive-compulsive disorder. Indian J Dermatol Venereol Leprol 2023;89:592–4.
Dear Editor,
Traction alopecia, which is an underreported form of hair loss in children, is caused by prolonged tension on the hair follicle and dermal papilla.1 The clinical presentation may vary from decreased hair density to patchy or complete alopecia. To the best of our knowledge, traction alopecia secondary to obsessive-compulsive disorder has not been previously reported in English literature, according to Web of Science and PubMed literature searches conducted on March 5, 2022 (search keywords: “traction alopecia” and “obsessive-compulsive disorder”; language, “English”).
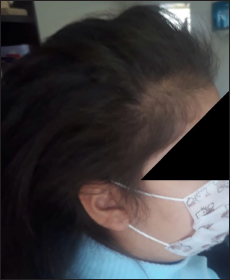
A 10-year-old Caucasian girl was admitted to the Atatürk University Hospital with complaints of symmetrical thinning of scalp hair above both ears for 18 months. Scalp biopsy performed at another institution was interpreted as cicatricial alopecia. There was involvement of the frontal and temporal scalp of the patient. The girl has been wearing her hair in a tight bun every day of the week since the last 18 months [Figure 1]. On a detailed history, her mother reported some intrusive and repetitive behaviours in the child which were also affecting her relationships with the family. After a psychiatric evaluation, we learned that she has been wearing a tight bun with the belief that something bad would happen to her if the strands were left out. Although the child admitted that the thought was illogical, absurd and bizarre, she reported that she was unable to control it. Apart from this compulsion, there were also other compulsions of the hoarding type (especially hair ties, and buckles), eating type (eating quickly, in large amounts and without getting hungry), and repeating type (repetitive questioning and saying the same sentence over and over). On assessment using the Yale-Brown Obsessive-Compulsive Scale and Clinical Global Impression-Severity and Improvement scales and through a structured interview, she met the Diagnostic and Statistical Manual of mental disorders, fifth edition (DSM-5) diagnostic criteria for obsessive-compulsive disorder.

- The first clinical presentation of the girl with traction alopecia
The Yale-Brown Obsessive-Compulsive Scale is an assessor-rated scale including 10 items.2 These items are scored on a four-point scale (0 = “no symptoms” to 4 = “extreme”). It assesses the severity of obsessive-compulsive disorder with scores ranging from 0 to 40 (moderate,16-23; severe, 24-31; and extreme, 32-40). The Clinical Global Impression is a clinician-rated scale that measures disease severity at admission and improvement or worsening after treatment.3 Both Clinical Global Impression-Severity and Clinical Global Impression-Improvement are rated on a Likert scale from 1 to 7. The Clinical Global Impression-Severity assesses the severity of the disease with scores ranging from 1 to 7 (normal to extremely sick). The Clinical Global Impression-Improvement evaluates response to treatment (1: very much improved, 7: very much worse).
Yale-Brown Obsessive-Compulsive Scale score was 35 and the Clinical Global Impression-Severity score was 7, pointing at severe symptoms on both scales. The patient was initiated on sertraline treatment with a starting dose of 1 mg/kg/day after a brief psychoeducational intervention. One month later, aripiprazole augmentation with a dose of 0.1 mg/kg/day was added and titrated up to 0.2 mg/kg/day. Although the patient’s traction alopecia-related problems improved within four months, the patient was followed up for six months with a monthly clinical assessment [Figure 2]. Afterwards, the drugs were tapered off. The end-of-treatment Yale-Brown Obsessive-Compulsive Scale scale score was 5 (the subclinical range is between 0 and 7) and the Clinical Global Impression-Improvement score was 2 (indicating much improvement).
- Post-treatment appearance of the child at the 4th-month follow-up
We present a case of traction alopecia with associated obsessive-compulsive disorder whose clinical findings improved after treatment of the latter.
Traction alopecia, also called “alopecia groenlandica,” was first reported in 1907.4 Since then, this entity is believed to be underreported.5 Although it is most commonly observed in women of African descent due to the preferred hairstyles, it has also been observed in children. A study including 1042 school-aged children (aged 6-21) found that traction alopecia was more common in girls, with a prevalence of 17.1%.6 Thus, raising clinical awareness of this condition is critical, especially for paediatric dermatologists as also other healthcare providers. Some hairstyles that cause the hair to be pulled tightly can increase the risk of traction alopecia, such as buns, tight ponytails or the use of hair extensions, hair pins and hair weaves.7 Also, applying tension to thermally straightened or chemically relaxed hair may further increase the risk for traction alopecia. Marginal traction alopecia, which is the most prevalent form, generally affects the frontal and temporal scalp and is typically accompanied by a “fringe sign.”7 This sign was also seen in our case [Figure 1].
Obsessive-compulsive disorder is a debilitating disorder which also affects children and adolescents with an estimated rate of 1-2%.8 It is characterised by excessive or repetitive behaviours, avoidance of certain situations or acceptance of intrusive thoughts or ideas.8 Children with obsessive-compulsive spectrum disorders are often referred to dermatology outpatient clinics for accompanying skin or hair problems.9 Thus, detailed questioning regarding behavioural changes is vital for optimal intervention. Effective treatment options include symptomatic treatment, behavioural therapy and/ or psychopharmacotherapy.9 In our case, aripiprazole augmentation of sertraline appeared to be an efficacious option to control symptoms of obsessive-compulsive disorder and traction alopecia.
An important differential diagnosis to take into account is trichotillomania which is listed as an obsessive-compulsive and related disorder according to the DSM-5 (American Psychiatric Association, 2013).10 Trichotillomania, one of the critical causes of acquired alopecia among children, is a psychiatric disorder characterised by recurrent, chronic, compulsive and deliberate hair plucking from different areas of the body, including the scalp, eyelashes, eyebrows, arms, legs and pubic area.11 Both conditions are more common in female patients and have a similarly distributed pattern of hair loss. Most often, in trichotillomania, the vertex and parietal regions of the scalp are affected in the form of irregular patches of hair loss showing various stages of hair regrowth, though it may present at any site on the scalp or body also.12 In traction alopecia, the scalp is usually the only affected area; other body areas are not involved.13 Unlike traction alopecia, trichotillomania is often accompanied by other psychiatric disorders in children.11 Further, in traction alopecia, the applied trauma is unintentional and usually caused by a specific hairstyle or hair styling method.
Treatment of traction alopecia varies according to the underlying causes and the age of presentation. Early intervention administered timely in the reversible stage is essential in the successful management. These approaches involve counselling, education and hair styling practices that minimise the tension on the hair.14 Patient education must aim to raise awareness about hairstyles, heat or chemicals that may be associated with traction alopecia risk. In particular, children with traction alopecia should be counselled about clinical signs and symptoms of this condition, such as itching, pain, discomfort, erythema and hair casts. Pharmacotherapy options include addressing inflammation and stimulating hair regrowth.13 However, using agents for hair regrowth promotion in the pediatric population requires further study.14
Apart from professional (e.g., ballerina), cultural (e.g., Africa, Japan), religious (e.g., Sikhism) and recreational factors, traction alopecia may be associated with psychological (obsessive-compulsive disorder) conditions. In order to minimise the impact, a multi-disciplinary approach is vital to managing a child with traction alopecia and obsessive-compulsive disorder. Early referral, intervention and psychoeducation can provide a significant advantage in paediatric population.
Declaration of patient consent
The patient gave her written informed consent to publish the case with the pictures.
Financial support and sponsorship
Nil.
Conflict of interest
There are no conflicts of interest.
References
- Traction alopecia in Sikh male patients. J Am Board Fam Med. 2007;20:497-8.
- [CrossRef] [PubMed] [Google Scholar]
- The Yale-Brown Obsessive Compulsive Scale. I. Development, use, and reliability. Arch Gen Psychiatry. 1989;46:1006-11.
- [CrossRef] [PubMed] [Google Scholar]
- Early clinical drug evaluation (ECDEU) assessment manual. Rockv Natl Inst Ment Heal 1976
- [Google Scholar]
- Traumatic marginal alopecia: Aspecial type: Alopecia groenlandica. Br J Dermatol. 1957;69:319-22.
- [CrossRef] [PubMed] [Google Scholar]
- Rapunzel alopecia: A peculiar form of non-marginal traction alopecia secondary to excessively long hair. Skin Appendage Disord. 2020;6:323-5.
- [CrossRef] [PubMed] [Google Scholar]
- Hairdressing is associated with scalp disease in African schoolchildren. Br J Dermatol. 2007;157:106-10.
- [CrossRef] [PubMed] [Google Scholar]
- The “Fringe Sign” - A useful clinical finding in traction alopecia of the marginal hair line. Dermatol Online J. 2011;17:1.
- [PubMed] [Google Scholar]
- Children with obsessive-compulsive disorder: Are they just “little adults”? J Clin Invest. 2009;119:737-46.
- [CrossRef] [PubMed] [Google Scholar]
- Obsessive-compulsive disorder in dermatology. J Dtsch Dermatol Ges. 2015;13:991-9.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnostic and statistical manual of mental disorders (DSM-5) In: American Psychiatric Association (5th ed.). Arlington, VA: American Psychiatric Publishing; 2013.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnosis and management of alopecia in children. Pediatr Clin North Am. 2014;61:427-42.
- [CrossRef] [PubMed] [Google Scholar]
- A practical approach to the diagnosis and management of hair loss in children and adolescents. Front Med (Lausanne). 2017;4:112.
- [CrossRef] [PubMed] [Google Scholar]
- Traction alopecia: How to translate study data for public education-closing the KAP gap? Dermatol Clin. 2014;32:153-61.
- [CrossRef] [PubMed] [Google Scholar]
- Review of traction alopecia in the pediatric patient: Diagnosis, prevention, and management. Pediatr Dermatol. 2021;38(Suppl 2):42-8.
- [CrossRef] [PubMed] [Google Scholar]





