Translate this page into:
Transcutaneous auricular vagus nerve stimulation treatment for cutaneous dirt-adherent disease complicated with rosacea
Corresponding author: Dr. Jian Li and Dr. Mingwang Zhang, Department of Dermatology Southwest Hospital, Third Military Medical University (Army Medical University), Jian Li, Chongqing, China. leejian728@tmmu.edu.cn
-
Received: ,
Accepted: ,
How to cite this article: Wei J, Xie L, Wan M, Kong M, Zhang M, Li J. Transcutaneous auricular vagus nerve stimulation treatment for cutaneous dirt-adherent disease complicated with rosacea. Indian J Dermatol Venereol Leprol. doi: 10.25259/IJDVL_1282_2024
Dear Editor,
Cutaneous dirt-adherent disease (CDAD) is a rare relapsing dermatosis that manifests with persistent adherence of dirt like substances occurring mainly on cheeks, forehead, breasts, and other areas with increased sebaceous activity.1 Erythematotelangiectatic rosacea (ETR) is the most common subtype of rosacea and is characterised by persistent erythema and flushing of the face.2 Traditionally, treatment methods including keratolytics, emollients, antifungal agents, and retinoids play an important role in the treatment of CDAD or ETR. However, these treatment modalities sometimes elicit a poor response or recurrence. New treatment options are needed in clinical practice.
Recent studies have indicated that psychological factors and neuroinflammation could be involved in the pathogenesis of the two diseases.1,3 Transcutaneous auricular vagus nerve stimulation (taVNS) is an efficacious non-invasive neuromodulation strategy that modulates the activity of the auricular branch of the vagus nerve by stimulating the outer conchal cavity.4 This manipulation has been demonstrated to ameliorate symptoms in patients with epilepsy, depression, migraine, and other functional neurological/psychological disorders.5 Hence, we propose that taVNS may be beneficial for the treatment of CDAD and ETR. Here, we report a case of patients with refractory CDAD and ETR that responded well to taVNS.
A 22-year-old girl presented to our department with a 4-year recurring history of rough, hypertrophic, yellowish-brown, and hard-to-peel adherent serous crusts densely covering the cheeks, eyelids, temporal regions, and eyebrows [Figure 1a]. She also had a 6-year history of facial flushing and erythema accompanied by itching [Figure 1b] and histopathology from the cheek was consistent with rosacea [Figure 2]. The patient consistently wore masks and hats to avoid social contact. The psychological self-questionnaire and psychologist evaluation indicated the presence of anxiety and depression [Table 1]. The patient underwent a range of treatments, including oral isotretinoin, H2-antagonists, doxycycline, topical emollients, and antifungal agents. Temporary symptomatic relief was achieved, typically lasting 1–2 months before relapse. This was generally followed by the occurrence of aggravated lesions. Cessation of medical treatment and stress also contributed to increased severity of lesions. Consequently, she consented to an off-label treatment with daily taVNS therapy, characterised by stimulation pulses at a frequency of 30 Hz and pulse width of 300 μs for 30 minutes per day. Concurrently, the importance of proper facial hygiene and the establishment of a facial cleaning diary were explained. After 3 weeks of treatment, she presented a significant reduction in adherent crusts, erythema, and flushing [Figure 3a]. In addition, she also experienced a significant reduction in the symptoms of anxiety and depression. No relapse was observed during the 6-months treatment-free follow-up period [Figure 3b].

- Thick yellowish-brown crusts overlying cheeks, temporal region, and eyebrows with mild swelling of the eyelids before treatment.

- Historical photograph showing the clinical condition prior to the current presentation: Note erythema and telangiectasia on the forehead, cheeks, nose, and eyelids.
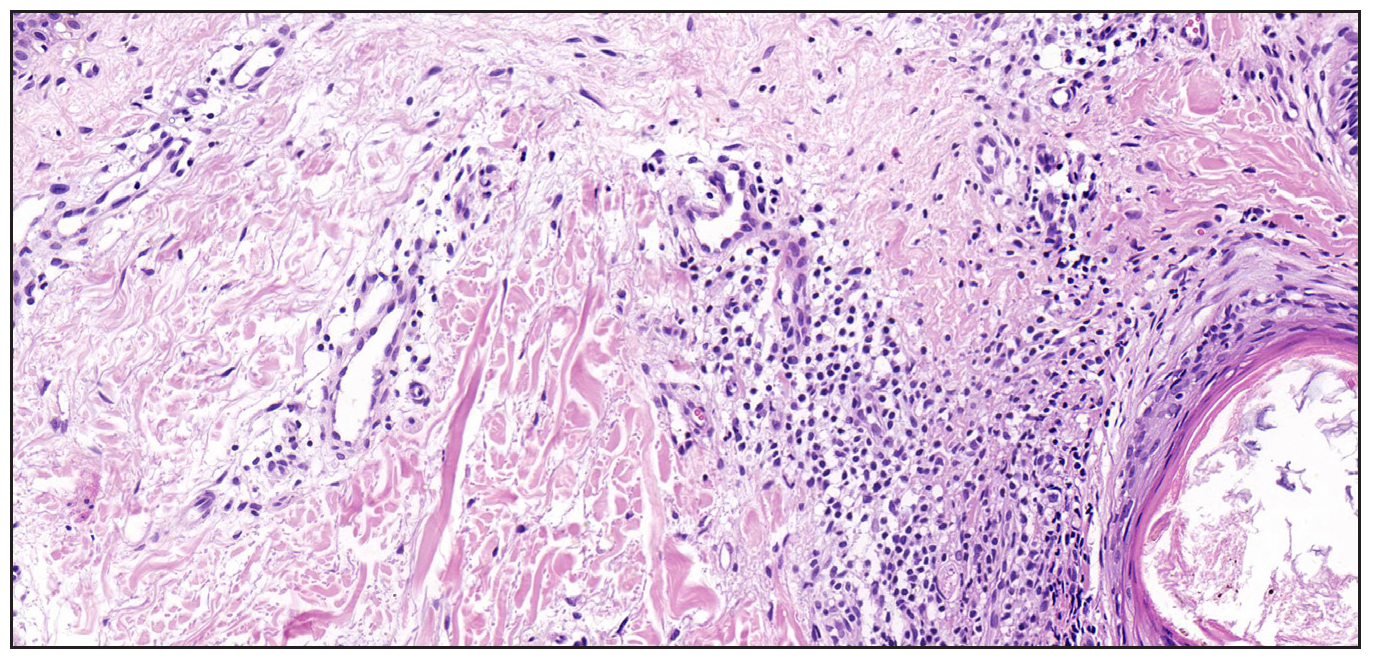
- Histopathological features. Histopathological examination of the skin from the patient’s cheek revealed scattered or focal lymphocytes and histiocytes surrounding the vessels in the superficial to mid-dermis. (Haematoxylin and eosin, 100x).
| Before treatment (week 0) | After treatment (3 weeks) | follow-up (6 months after treatment) | |
|---|---|---|---|
| Assessment of CADA/ETR | |||
| Crust | Cheeks, eyelids, temporal, and eyebrows | None | None |
| Swellinga | 2 | 0 | 0 |
| Itchingb | 2 | 0 | 0 |
| Sting/burnc | 1 | 0 | 0 |
| Clinician’s Erythema Assessment (CEA) scored | 3 | 2 | 1 |
| Patient Self-Assessment (PSA) scoree | 3 | 1 | 1 |
| Global Flushing Severity Scale (GFSS) scoref | 7 | 2 | 0 |
| Psychological examination | |||
| Patient Health Questionnaire-9 (PHQ-9) scoreg | 7 | 3 | 3 |
| Generalized Anxiety Disorder-7 (GAD-7) scoreh | 14 | 5 | 2 |
a, b and c: Assessing facial swelling, itching, or sting/burn condition, ranking severity on a scale of 0–4: 0, None; 1, Slight; 2, Mild; 3, Moderate; or 4, Severe;
d: Clinician’s erythema assessment (CEA) score (assessing the patient’s facial erythema condition, ranking severity on a scale of 0–4: 0, clear; 1, almost clear; 2, mild; 3, moderate; or 4, severe);
e: Patient self-assessment (PSA) score (self-assessing the facial erythema condition, ranking severity on a scale of 0–4: 0, clear; 1, almost clear; 2, mild; 3, moderate; or 4, severe);
f: Global flushing severity scale (GFSS) score (assessing the patient’s facial flushing condition: 0, did not have, 1–3, mild; 4–6, moderate; 7–9, severe; or 10, extreme);
g: Patient health questionnaire-9 (PHQ-9) score (assessing the patient’s depression condition: 5–9, mild; 10–14, moderate; or >14, moderately severe/severe);
h: Generalised anxiety disorder-7 (GAD-7) score (assessing the patient’s anxiety condition: 5–9, mild; 10–14, moderate; or >14, moderately severe/severe).

- After 3 weeks of TaVNS treatment: The adherent crusts and edema completely resolved, erythema and telangiectasia showed significant improvement.

- Follow-up after 6 months without treatment: Facial erythema and telangiectasia further alleviated and there was no recurrence of crust formation.
The diagnosis of CDAD and ETR is primarily clinical, given the scarcity of definitive biological markers. The assessment hinges on a meticulous review of the patient’s medical history with particular attention to the recurrent episodes of facial erythema and flushing that typically precede the formation of crusts. These clinical features are instrumental in establishing a diagnosis of CDAD complicated with ETR.
TaVNS has emerged as a promising therapeutic modality for functional neurological and psychological disorders.5 It has been demonstrated to ameliorate both facial dermatological symptoms and concomitant psychological manifestations. Studies have implicated taVNS in modulating the inflammatory response by regulating cholinergic signalling pathways, both peripherally and centrally. This modulation is positioned to enhance synaptic plasticity within key brain regions of the central nervous system, thereby improving cognitive function and alleviating mental symptoms. Moreover, studies have also shown that taVNS is linked to the neuro-skin axis that regulates the relationship between brain regions to alleviate neuroinflammatory effects.5,6 We propose that CDAD and ETR could be manifestations of underlying neurological or psychological conditions, sharing similarities in their clinical presentations and underlying pathophysiological mechanisms. The presence of facial destructive lesions has been correlated with the onset of psychological distress in affected individuals. Furthermore, the exacerbation of psychological stressors is believed to contribute to the progression or relapse of CDAD and ETR.7 Therefore, we postulated that taVNS may be an effective treatment for CDAD and ETR. Besides, we treated other 10 cases of refractory ETR by TaVNS and all the patients achieved satisfactory improvement in facial erythema and flushing symptoms.
The therapeutic effect of taVNS and the detailed mechanism of CDAD or ETR require further exploration. To our knowledge, this is the first reported case of CDAD complicated with ETR that was successfully treated using taVNS. TaVNS is expected to be a new therapeutic option to treat patients with ETR or CDAD.
Ethical approval
The research/study was approved by the Institutional Review Board at the Medical Ethics Committee of Southwest Hospital, number (A)K203192, dated 2023.12.15.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Fund: The Doctoral ‘Through Train’ Research Program of Chongqing, China (No. CSTB2022BSXM-JCX0021).
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Dermatosis neglecta based on exanthematous drug eruption following head trauma: A case report and literature review. Clin Cosmet Investig Dermatol. 2023;16:2083-8.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Epidemiology of acne and rosacea: A worldwide global study. J Am Acad Dermatol. 2024;90:1016-8.
- [CrossRef] [PubMed] [Google Scholar]
- Recent advances in understanding and managing rosacea. F1000Res. 2018;7:F1000 Faculty Rev-1885.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Vagus nerve stimulation attenuates the systemic inflammatory response to endotoxin. Nature. 2000;405:458-62.
- [CrossRef] [PubMed] [Google Scholar]
- A review of vagus nerve stimulation as a therapeutic intervention. J Inflamm Res. 2018;11:203-13.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Neural networks and the anti-inflammatory effect of transcutaneous auricular vagus nerve stimulation in depression. J Neuroinflammation. 2020;17:54.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Updates on the risk of neuropsychiatric and gastrointestinal comorbidities in rosacea and its possible relationship with the gut-brain-skin axis. Int J Mol Sci. 2020;21:8427.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]





