Translate this page into:
Transient autoimmune thyroiditis associated with Sweet's syndrome
Correspondence Address:
Vinay Shanker
Department of Dermatology, Venereology and Leprosy, Indira Gandhi Medical College, Shimla - 171 001, Himachal Pradesh
India
| How to cite this article: Rattan R, Sharma A, Shanker V, Tegta GR, Verma GK. Transient autoimmune thyroiditis associated with Sweet's syndrome. Indian J Dermatol Venereol Leprol 2016;82:112 |
Sir,
Sweet's syndrome, also known as acute febrile neutrophilic dermatosis, is an inflammatory skin disorder characterized by an acute onset of painful erythematous papules, plaques or nodules. Fever and peripheral neutrophilic leucocytosis are also present. A dense neutrophilic infiltrate without evidence of primary vasculitis is seen on histopathology. It is usually associated with infections, inflammatory bowel disease, pregnancy, malignancies, autoimmune connective tissue diseases and drugs. We describe a patient with Sweet's syndrome who subsequently developed transient autoimmune thyroiditis.
A 52-year-old diabetic and hypertensive woman presented with a 5 day history of high grade fever and tender red lesions. Cutaneous examination revealed erythematous papules and nodules which were distributed over the trunk, limbs and face. These coalesced to form irregular, edematous plaques with well defined margins and pseudo-vesiculation [Figure - 1]a and [Figure - 1]b. There was no mucosal involvement. Her systemic examination was within normal limits and there was no enlargement or tenderness of the thyroid gland. There was no history suggestive of preceding infections, thyroid dysfunction, autoimmune connective tissue disease or malignancy. She was receiving olmesartan and hydrochlorothiazide for hypertension along with metformin and glimepiride for diabetes. She gave no history of any other drug intake prior to the onset of lesions.
 |
| Figure 1: (a and b) Erythematous papules and nodules at the time of presentation |
Laboratory and imaging evaluation was done to establish the diagnosis of Sweet's syndrome and investigate possible associated infectious, inflammatory or neoplastic conditions. The haemogram revealed raised a total leukocyte count (14,000/mm 3), neutrophilia (75%) and a raised ESR (120 mm in first hour). The C reactive protein test was positive. Liver and renal function tests, urine and stool microscopy, chest X-ray and ultrasound of the abdomen/pelvis did not reveal any abnormality. Blood and urine cultures were sterile.
Incidentally, the patient had her thyroid function tests done on the second day of illness, which showed normal T3, T4 and TSH levels. However, a repeat thyroid function test revealed normal T3 (1.0 ng/ml), raised T4 (15.60 µg/dl), decreased TSH (0.07 mIU/ml) and markedly raised anti-TPO antibodies (>1300 U/ml). Ultrasonography of the thyroid region was normal. A thyroid scan showed minimal tracer uptake in the thyroid bed region [Figure - 2]. All these findings were suggestive of autoimmune thyroiditis.
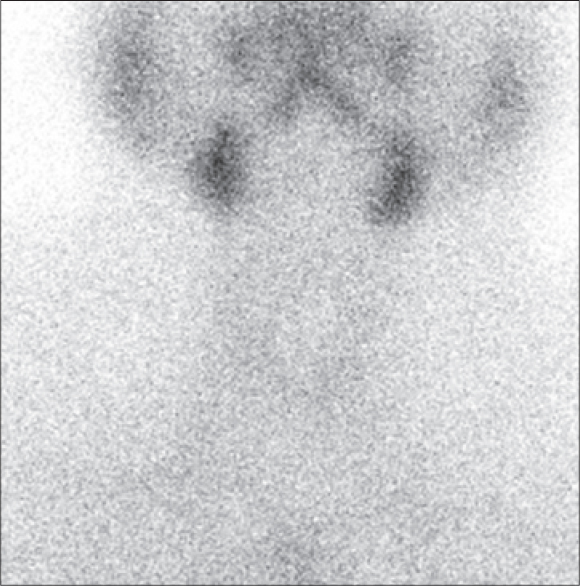 |
| Figure 2: Thyroid scan showing minimal uptake in the thyroid bed region |
Histopathological examination of the skin biopsy showed a diffuse dense infiltrate of neutrophils involving the upper and mid dermis with edema of the papillary dermis [Figure - 3]. On the basis of clinical and histopathological findings, a diagnosis of Sweet's syndrome was made. She was treated with oral corticosteroids following which the fever subsided in two days and skin lesions in five days [Figure - 4]. The dose of corticosteroids was tapered down over the course of four weeks. Thyroid function tests were repeated after a month. The T3, T4 and TSH levels returned to normal, anti-TPO antibodies levels decreased (828 mIU/ml) and the thyroid scan showed normal uptake [Figure - 5].
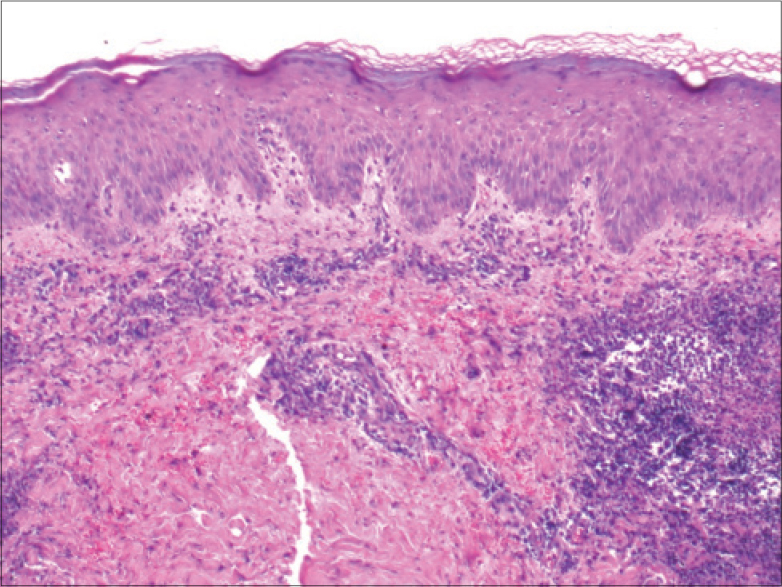 |
| Figure 3: Edema and dense neutrophilic infiltrate in the upper dermis (H and E, ×40) |
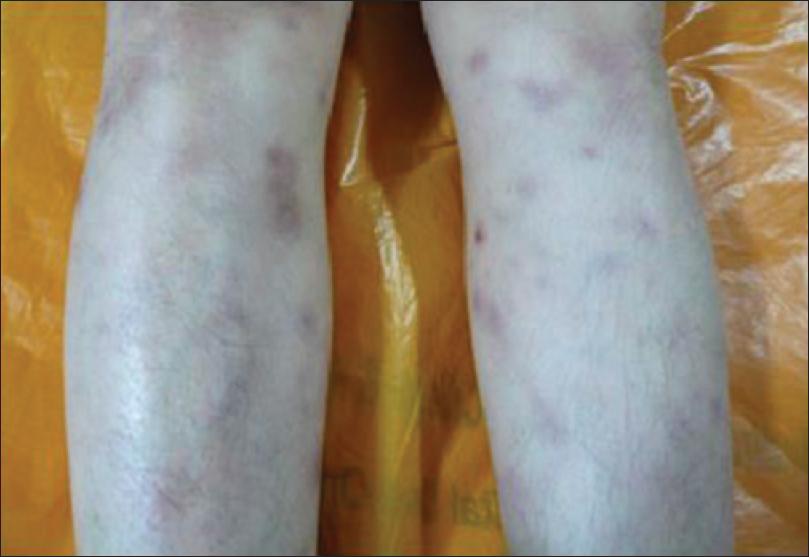 |
| Figure 4: Improvement in clinical appearance after starting corticosteroids |
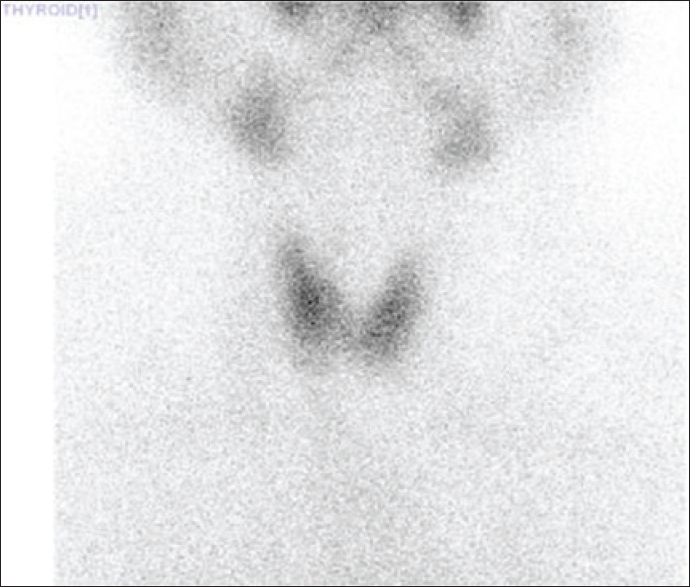 |
| Figure 5: Thyroid scan after 4 weeks of treatment, showing normal uptake in the thyroid bed region |
Sweet's syndrome may be idiopathic or associated with a variety of systemic disorders in about 50% of cases. These may occur either before, simultaneously or after the disease.[1],[2] Classical or idiopathic Sweet's syndrome typically affects women in the third to fifth decade of life. The disease process is postulated to result from a hypersensitivity reaction to bacterial, viral or tumor antigens. Cytokines may also have a direct or indirect role. Further evidence comes from the association of Sweet's syndrome in patients with thyroid disease.[3] The appearance of Sweet's syndrome and thyroiditis in the same patient is probably associated with the immune mediated effects of helper T-cell type 1 cytokines (IL1, IFN-γ, TNF-α).[1],[4] It could also be due to a common causative agent. Based on a literature search, we could find four cases of Sweet's syndrome associated with Hashimoto's thyroiditis.[3],[4],[5],[6],[7] Two cases of association with subacute thyroiditis have also been reported.[8],[9]
Our patient fulfilled the diagnostic criteria for Sweet's syndrome. There were no clinical or laboratory findings suggestive of pre-existing thyroiditis. Her thyroid function tests and thyroid uptake improved with treatment, and was normal at the third and sixth month of follow up. We believe that our patient developed transient thyroiditis due to Sweet's syndrome, as she had no pre-existing thyroiditis and the thyroid functions tests returned to normal after treatment. Occurrence of both these conditions could be coincidental as well. We suggest that a possibility of autoimmune thyroiditis should be kept in mind while evaluating a patient of Sweet's syndrome due to the increasing evidence of association with thyroid disease.
| 1. |
Cohen Philip R, Kurzrock Razelle. Sweet's syndrome revisited: A review of disease concepts. Int J Dermatol. 2003;42:761-78.
[Google Scholar]
|
| 2. |
Cox NH, Jorizzo JL, Bourke JF and Savage. Vasculitis, Neutrophilic Dermatoses and Related Disorders. In: Burns T, Breathnach S Cox N, Griffiths C, editors. Rook's Textbook of Dermatology. 8th ed. Singapore: Wiley Blackwell, 2010. p. 50.74.
[Google Scholar]
|
| 3. |
Francisco CR, Patal PC, Cubillan EA, Isip-Tan IT. Sweet's syndrome associated with Hashimoto's thyroiditis. BMJ Case Rep. 2011 Aug 24;2011.
[Google Scholar]
|
| 4. |
Freedberg I M, Eisen A Z, Wolff K, Austen K F, Goldsmith L A, Katz S I. Acute febrile neutrophilic dermatosis. Fitzpatrick's Dermatology in General Medicine. 2003;1:949-59.
[Google Scholar]
|
| 5. |
Nakayama H, Shimao S, Hamamoto T, Munemura C, Nakai A. Neutrophilic dermatosis of the face associated with aortitis syndrome and Hashimoto's Thyroiditis. Acta Derm Venereol. 1993;73:380-1.
[Google Scholar]
|
| 6. |
Medeiros S, Santos R, Carneiro V, et al. Sweet syndrome associated with Hashimoto thyroiditis. Dermatol Online J. 2008;14:10.
[Google Scholar]
|
| 7. |
Saeed M, Brown GE, Agarwal A, Pellowski D, Jacks J, Liverett HK, Vyas KS. Autoimmune clustering: Sweet syndrome, Hashimoto thyroiditis, and psoriasis. J Clin Rheumatol. 2011 Mar; 17(2):76-8.
[Google Scholar]
|
| 8. |
Alcalay J, Filhaber A, David M, et al. Sweet's syndrome and subacute thyroiditis. Dermatologica. 1987;174:28-9.
[Google Scholar]
|
| 9. |
Kalmus Y, Kovatz S, Shilo L, et al. Sweet's syndrome and subacutethyroiditis. Postgrad Med J. 2000;76:229-30.
[Google Scholar]
|
Fulltext Views
2,167
PDF downloads
2,470





