Translate this page into:
Trichosporon inkin causing subcutaneous sinus tract: Successfully treated by oral and ultrasound-guided intralesional itraconazole therapy
2 Department of Clinical Laboratory, West China Hospital, Sichuan University, Chengdu 610041, Sichuan, P.R. China
3 Department of Dermatovenereology, West China Hospital, Sichuan University, Chengdu 610041, Sichuan, P.R. China
Correspondence Address:
Ran Yuping
Department of Dermatovenereology, West China Hospital, Sichuan University, Chengdu 610041, Sichuan
P.R. China
| How to cite this article: Xiaoxi X, Yaling D, Kaiwen Z, Xin R, Pradhan S, Yuping R. Trichosporon inkin causing subcutaneous sinus tract: Successfully treated by oral and ultrasound-guided intralesional itraconazole therapy. Indian J Dermatol Venereol Leprol 2017;83:506-509 |
Sir,
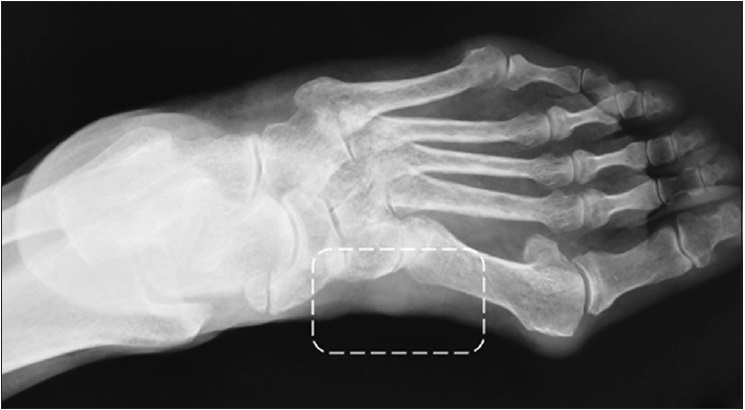
A 62-year-old Chinese woman presented with complaints of continuous discharge from the lateral aspect of the left foot since 3 months. The patient had initially noticed pruritus along with erythema and scaling on the left dorsum of the foot, preceding the onset of discharge. She did not seek medical attention at the time. The lesion developed into an ulcer on the dorsum of foot in 1 month with erosions on the lateral aspect of the foot. She underwent skin grafting and the graft was harvested from the left thigh to cover the ulcer. The graft took up well; however the lesions on the lateral aspect of the foot did not heal and continued to ooze. Cutaneous examination at the time of presentation revealed light yellow exudate from the lesion and tenderness on palpation [Figure 1a]. A radiograph of the affected part showed subcutaneous sinus formation [Figure 1b]. The patient was in good clinical condition without any underlying disease such as hypertension, diabetes or any other injury. A 20% potassium hydroxide smear revealed some short rod-like hyphae and oval spores [Figure 1c]. The cultures from the tissue grew white, cerebriform colonies with a rough surface after 5 days of incubation at both 25°C and 37°C [Figure 1d]. Deoxyribonucleic acid sequencing of the isolate was identical to Trichosporon inkin (ID: KU745296).
 |
| Figure 1a: Erosions with discharge on the medial aspect of the left foot (black circle) and black arrow pointing toward the position where she received the skin graft |
 |
| Figure 1b: X-ray showing the sinus in the lesion (in the white box) |
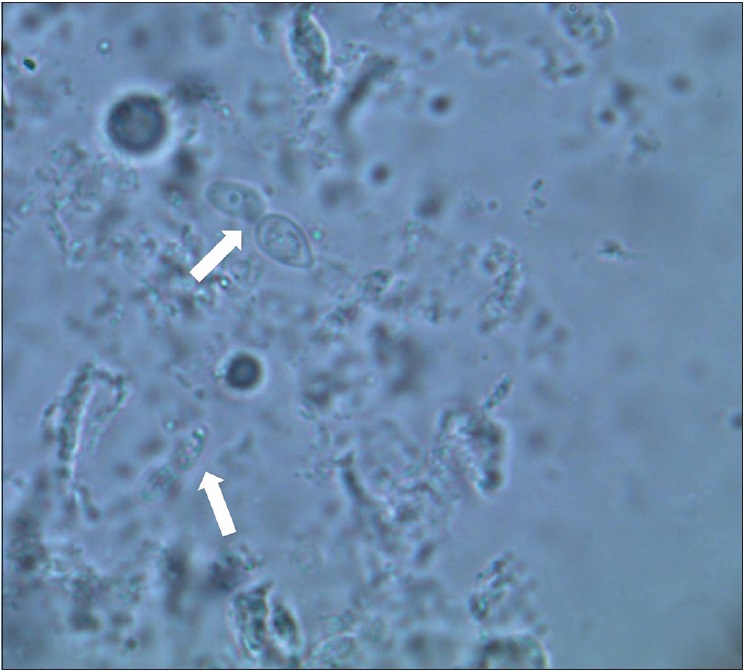 |
| Figure 1c: Fungal spores observed in a 20% KOH smear (×1000) |
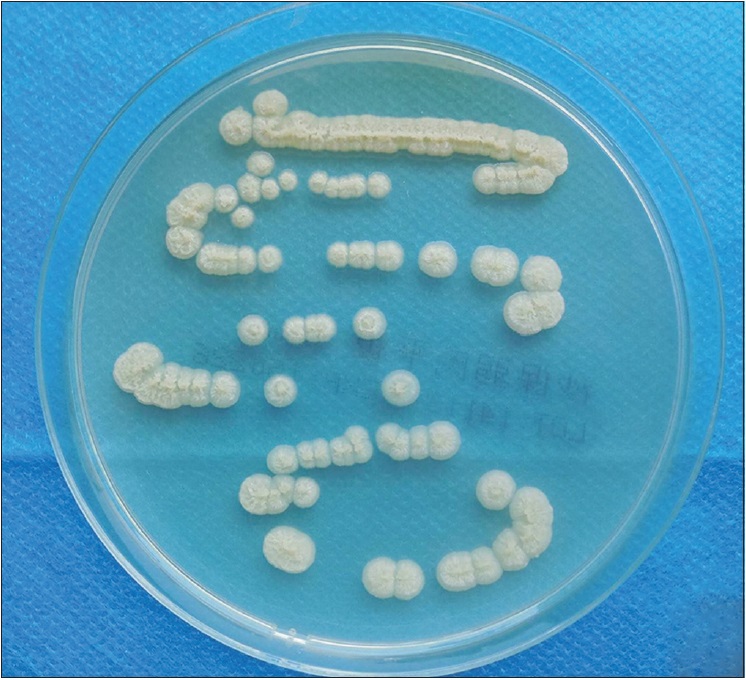 |
| Figure 1d: The culture of tissue exhibiting cerebriform colonies of fungi at both 25°C and 37°C |
She was started on treatment with oral itraconazole 200 mg twice a day and 1% naftifine and 0.3% ketoconazole cream topically. After 16 days, the lesion showed slight improvement, but cultures from the sections still demonstrated the same fungus as before treatment. In this case, susceptibility tests on the isolate showed itraconazole to be a good inhibitor of T. inkin (minimal inhibitory concentration ≤0.125 mg/L). However, scar formation due to the chronic inflammation and poor circulation was thought to reduce the local drug concentration and affect the efficacy of treatment. Hence, we injected itraconazole at five sites near the lesion (6.5 ml, containing 21.45 mg itraconazole in total), under ultrasonic guidance, making sure that the drug concentration surpassed the minimal inhibitory concentration of itraconazole [Figure 2a] and [Figure 2b]. Itraconazole solution was aseptically prepared before the procedure by diluting one 250 mg (25 ml) vial of injectable itraconazole (Sporanox, Janssen Pharmaceutica N.V.) in 50 ml normal saline to obtain 75 ml solution containing 3.3 mg/ml of drug. The injection sites became red, swollen and painful with elevated skin temperature on the first day of injection. However, no fever or other systemic effects were observed. The lesion scabbed without any discharge 20 days later. Oral itraconazole was continued for a month till the lesion totally resolved [Figure 3a] with a following X-ray showing no sinus tract [Figure 3b].
 |
| Figure 2a: Ultrasound-guided intralesional itraconazole administration: itraconazole was injected in five sites nearby the lesion (white trigon) |
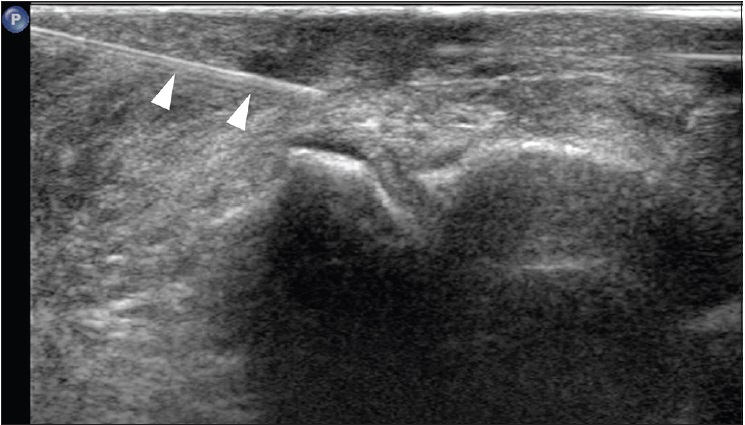 |
| Figure 2b: Ultrasonic image of the intralesional injection, the trigons pointed at injection needle |
 |
| Figure 3a: Lesions after treatment: 1 month after the injection of itraconazole, the lesion was totally cured |
 |
| Figure 3b: X-ray examination after treatment: X-ray showing no sinus tract in her left foot |
Trichosporon spp. is widely distributed in nature and is commonly isolated from the soil. Invasive infections caused by these species were usually reported in immunocompromised hosts.[1] Currently, T. inkin has not yet been found to cause subcutaneous sinus tract. However, in our patient, the fact that antifungal therapy finally cured the sinus demonstrates the significance of its pathogenicity. Cancer, invasive procedures, organ transplantation and broad-spectrum antibiotic therapy are risk factors for trichosporosis.[1] In our case, it is still unclear whether the subcutaneous trichosporosis was a primary or a secondary infection. As the woman was a farmer, long-term exposure to the soil and vegetative matter, minor trauma and the skin graft may have predisposed her to the infection.
There is no standard therapy for infections due to this fungus. On scanning the literature regarding the patients with this infection from 1996 to 2015, the cured cases were found to be treated with oral or intravenous amphotericin, azoles or caspofungin with an average treatment duration of 42.8 days. Associated diseases include white piedra, pemphigus, endocarditis, peritonitis and rheumatoid arthritis.[2] However, in the lesions associated with scar formation, necrotic tissue and ischemia, the tissue penetration of the drug is decreased greatly and in such cases, systemic treatment alone is inadequate. We need better modes of drug delivery to increase the local drug concentration in a direct and efficient manner. Intralesional pharmacotherapy has been tried in animal cutaneous sporotrichosis.[3] In these cases, amphotericin (usually 5 mg/ml) was injected every 2 weeks without any systemic adverse effects. Tani et al. first used transbronchial intracavitary itraconazole in pulmonary aspergilloma, twice a week for a total of 9 times (715 mg).[4] Temporary fever and elevation of C-reactive protein was observed during treatment. Intralesional itraconazole was also tried in an acute myelomonocytic leukemia patient who developed Candida krusei fungemia and fungal myositis. Itraconazole was injected into the muscles 5 mg daily for 10 days without any significant complication.[5]
We are reporting this case due to the rarity of subcutaneous trichosporosis in an immunocompetent individual and the good response to therapy. Ultrasound-guided intralesional injection not only ensures the precision and safety of administration, but also helps to observe the condition of the lesion at the same time. It has a very promising prospect in refractory subcutaneous fungal infections.
Acknowledgment
We would like to thank the ultrasonography department of West China Hospital, Sichuan University, for their help in ultrasound examination.
Financial support and sponsorship
This work is supported by Project 81472539 of the National Natural Science Foundation of China.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Colombo AL, Padovan AC, Chaves GM. Current knowledge of Trichosporon spp. and Trichosporonosis. Clin Microbiol Rev 2011;24:682-700.
[Google Scholar]
|
| 2. |
Shivaprakash MR, Singh G, Gupta P, Dhaliwal M, Kanwar AJ, Chakrabarti A. Extensive white piedra of the scalp caused by Trichosporon inkin: A case report and review of literature. Mycopathologia 2011;172:481-6.
[Google Scholar]
|
| 3. |
Gremião I, Schubach T, Pereira S, Rodrigues A, Honse C, Barros M. Treatment of refractory feline sporotrichosis with a combination of intralesional amphotericin B and oral itraconazole. Aust Vet J 2011;89:346-51.
[Google Scholar]
|
| 4. |
Tani S, Tomioka H, Tsuchimoto K, Kaneda T, Kubota M, Kaneko M, et al. A case of pulmonary aspergilloma successfully treated with trans bronchial intracavitary itraconazole. Nihon Kokyuki Gakkai Zasshi 2008;46:997-1002.
[Google Scholar]
|
| 5. |
Lin XJ, Yao RX, He MQ, Zhu BL, Guo WJ. Treatment of fungal myositis with intra-lesional and intravenous itraconazole: A case report. J Med Case Rep 2013;7:132.
[Google Scholar]
|
Fulltext Views
3,305
PDF downloads
1,751





