Translate this page into:
Tufted hair folliculitis associated with Melkersson-Rosenthal syndrome and hidradenitis suppurativa
Correspondence Address:
Sule Gungor
Department of Dermatology, Okmeydan? Training and Research Hospital, Dar�llacize Street, Istanbul
Turkey
| How to cite this article: Gungor S, Yuksel T, Topal I. Tufted hair folliculitis associated with Melkersson-Rosenthal syndrome and hidradenitis suppurativa. Indian J Dermatol Venereol Leprol 2014;80:484 |
Sir,
Case 1 a 23-year-old male presented to our clinic with a 3-year history of chronic, relapsing, inflammatory lesions and alopecia of the scalp. His medical history and medical records showed that he was diagnosed as Melkersson-Rosenthal syndrome 15 years earlier. Dermatological examination showed scarring alopecia within tufts of hair, fissured tongue, and macroglossia [Figure - 1]. Dermoscopic evaluation showed tufts of hair with perifollicular scaling and interfollicular white and milky red areas [Figure - 2]. Histopathological examination showed clustering of several adjacent hair follicles surrounding fibrotic tissue. As no active inflammatory lesions were observed, medical treatment was not initiated.
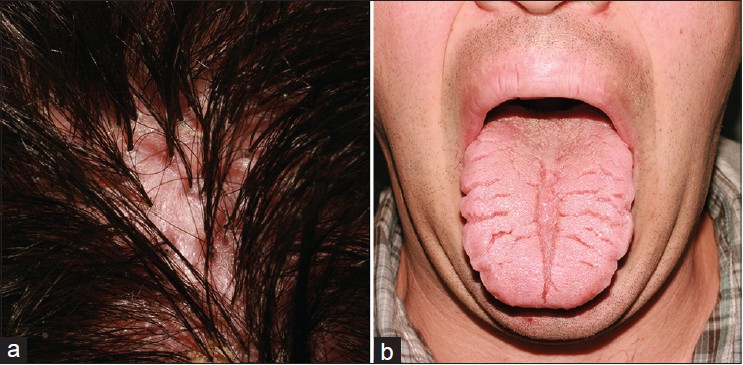 |
| Figure 1: (a) Scarring alopecia within tufts of hair (b) Fissured tongue and macroglossia |
Case 2 a 25-year-old male presented to our clinic with 1-year history of tufted hairs on the scalp, and painful nodules in the axillary and inguinal regions. Dermatological examination showed multiple hairs emerging from a single, dilated follicular ostia, adherent yellow-white perifollicular crusts on the scalp, and deep-seated nodules in the axillary-inguinal regions [Figure - 3]. Dermoscopic evaluation of the scalp showed tufts of hair with perifollicular tubular scaling, perifollicular whitish coloration in a starburst pattern, and interfollicular concentrically oriented blood vessels [Figure - 4]. A punch biopsy of the scalp was performed and histopathological examination revealed superficial and deep folliculitis involving several follicles opening into a common ostium from which multiple hairs emerged. Based on the clinical and histopathological findings, we made a diagnosis of tufted hair folliculitis associated with hidradenitis suppurativa. Doxycycline 100 mg, twice a day was given for two months; the inflammatory lesions resolved, but tufts of hair remained unchanged.
 |
| Figure 2: Dermoscopic examination shows tufts of hair with perifollicular scaling and interfollicular white and milky red areas |
 |
| Figure 3: (a) Multiple hairs emerging from a single dilated follicular ostia and adherent yellow-white perifollicular crusts on the scalp (b) Deep-seated nodules on the axillary-inguinal regions |
 |
| Figure 4: Dermoscopic examination shows tufts of hair with perifollicular scaling and interfollicular dotted vessels |
DISCUSSION
Tufted hair folliculitis is characterized by irregular areas of scarring alopecia within tufts of hair emerging from dilated follicular orifices as a result of recurrent and progressive folliculitis of the scalp. [1],[2],[3]
Melkersson-Rosenthal syndrome is a clinical entity characterized by the triad of recurrent facial paralysis, recurrent labial edema, and fissured tongue. Although the etiopathogenesis of Melkersson-Rosenthal syndrome is not fully known, histological examination shows granulomatous inflammation and eventually it is an inflammatory disease. [4] Hidradenitis suppurativa is an inflammatory disorder originating from the hair follicle. Clinically, it is characterized by inflamed nodules, abscesses followed by sinus tracts, fistulae, and scars. [5] Case 2 had tufted hair folliculitis associated with hidradenitis suppurativa, suggesting that tufted hair folliculitis on the scalp may be an end stage of hidradenitis suppurativa involving the scalp, which is agreement with Pujol′s hypothesis [3] that tufted hair folliculitis is a secondary phenomenon that occurs following primary follicular damage.
Dermoscopic evaluation in case 1 showed interfollicular milky red areas, and concentrically oriented vessels were noted in case 2; these features were consistent with the duration of the lesions. The scalp lesions in case 1 were in the inactive fibrous stage and there was no observable infiltration in the perivascular region, whereas in case 2 the scalp lesions were in the active inflammatory phase and there was perivascular and dermal neutrophil, eosinophil, and plasma cell infiltration resulting in interfollicular twisted vessels. Perifollicular whitish starburst coloration was observed in case 2, indicative of the active stage or prefibrotic stage.
Herein we reported 2 cases of tufted hair folliculitis in association with 2 distinct inflammatory disorders; the 2 cases indicate that tufted hair folliculitis is not a specific disease, but a secondary phenomenon that occurs in inflammatory diseases. Additionally, the dermoscopic features of both the active and inactive phases of tufted hair folliculitis were described.
| 1. |
Annessi G. Tufted folliculitis of the scalp: A distinctive clinicohistological variant of folliculitis decalvans. Br J Dermatol 1998;138:799-805.
[Google Scholar]
|
| 2. |
Habif TP. Clinical Dermatology: A Color Guide to Diagnosis and Therapy. 5 th ed. Vol. 24. Edinburg, UK: ElsevierInc; 2010. p. 913-46.
[Google Scholar]
|
| 3. |
Pujol RM, García-Patos V, Ravella-Mateu A, Casanova JM, de Moragas JM.Tufted hair folliculitis: A specific disease? Br J Dermatol 1994;130:259-60.
[Google Scholar]
|
| 4. |
Madke BS, Ghia D, Gadkari R, Nayak C. Cheilitis granulomatosa (Miescher granulomatous macrocheilitis) with trisomy 21. Dermatol Online J 2012;18:7.
[Google Scholar]
|
| 5. |
Syed ZU, Hamzavi IH. Atypical hidradenitis suppurativa involving the posterior neck and occiput. Arch Dermatol 2011;147:1343-4.
[Google Scholar]
|
Fulltext Views
8,033
PDF downloads
2,693





