Translate this page into:
Ulcerated necrobiosis lipoidica: A cutaneous granulomatous reaction associated with systemic B-cell lymphoma
2 Department of Pathology, Razi Hospital, Tehran University of Medical Sciences, Tehran, Iran
Correspondence Address:
Ifa Etesami
Razi Hospital, Vahdat-e-Eslami Square, Tehran
Iran
| How to cite this article: Mahmoudi H, Daneshpazhooh M, Kamyab K, Bafruee NB, Kiani A, Etesami I. Ulcerated necrobiosis lipoidica: A cutaneous granulomatous reaction associated with systemic B-cell lymphoma. Indian J Dermatol Venereol Leprol 2018;84:481-484 |
Sir,
A 40-year-old man presented to our department with bilateral chronic leg ulcers of 3 years duration. Skin biopsy at the onset of the disease showed granulomatous inflammation in a layered pattern in the dermis and upper subcutaneous layer, suggestive of necrobiosis lipoidica. He was then lost to follow up until he presented with an exacerbation of disease which was present since 3 months. The ulcers did not heal with topical antiseptics and corticosteroids. During the last 3 years, the only positive history was a suspicious history of chronic epididymitis, which had been treated as tuberculosis. Of note, he had lost 12 kg in the last 3 months. Physical examination revealed extensive ulcers on his legs [Figure - 1]. Biopsy of the leg ulcers showed layers of granulomatous lymphohistiocytic infiltration and alternating necrobiosis and fibrosis, compatible with necrobiosis lipoidica [Figure - 2]. Smears for Ziehl–Neelsen stain, cultures and polymerase chain reaction for mycobacteria and fungi were all negative.
 |
| Figure 1: Multiple ulcers on the leg |
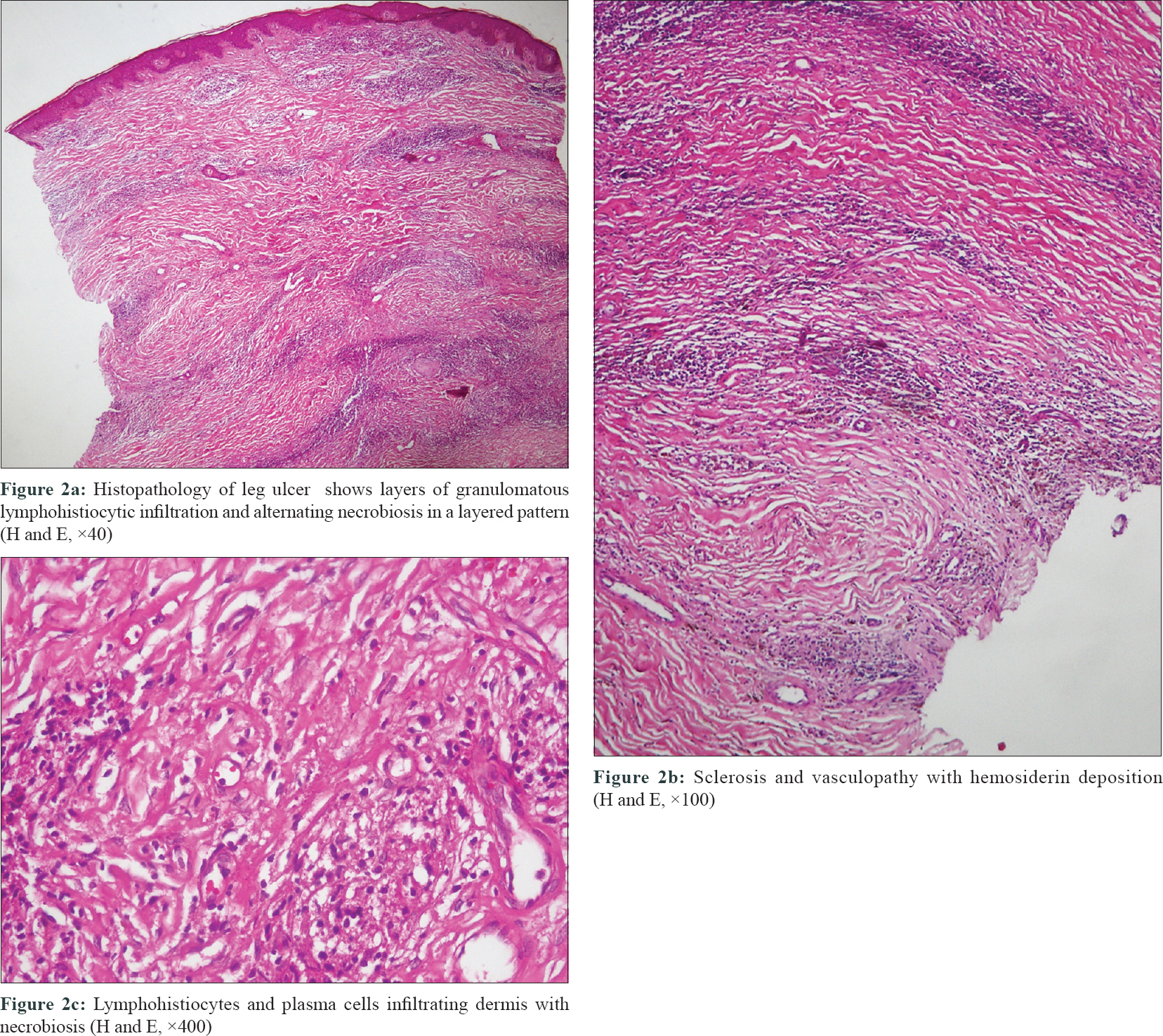 |
| Figure 2 |
Laboratory studies showed anemia, leukopenia and high erythrocyte sedimentation rate (103 mm/h; Ref- up to 20 mm/h). Renal and hepatic profiles and blood glucose levels were normal. Viral markers for HIV, hepatitis B, C, human T-lymphotropic virus 1 and 2 were all negative. Serum protein electrophoresis was normal.
Spiral computed tomography scan of the chest revealed reticulonodular opacities in the basal portion of both lungs, suggestive of tuberculosis. Three sputum smears were negative for acid-fast bacillus. The computed tomography scan of the abdomen was normal.
In view of bicytopenia, a bone marrow biopsy was performed, which showed nonnecrotizing granulomatous inflammation, which was negative for acid fast bacilli by Ziehl–Neelsen staining. As multiple areas of granulomatous inflammation was found in different organs such as skin, bone marrow and probably epididymis, we did a thorough investigation in our patient, including serum angiotensin-converting enzyme level, C-antineutrophil cytoplasmic antibody and P-antineutrophil cytoplasmic antibody, tuberculin skin test, polymerase chain reaction for acid fast bacilli and fungi. However, all the tests were negative. As the workup did not reveal any signs of malignancy or inflammatory conditions, considering the chest computed tomography scan findings, the high prevalence of tuberculosis in our country and his previous history of epididymitis, the patient received a four-drug regimen for tuberculosis for nearly 2 months with no improvement. During the second month of receiving the antituberculosis therapy, lymph node enlargement was noted in his right lateral neck. A biopsy from his lymph node revealed diffuse sheets of large immunoblastoid cells admixed with few scattered giant cells, frequent mitotic figures and many apoptotic bodies in-between, suggestive of B-cell lymphoma [Figure - 3]. Immunohistochemical stainings showed positive staining for CD10, CD20 and Bcl6 and confirmed the diagnosis of diffuse large B-cell lymphoma [Figure - 3]. The patient was referred to the hematologist and received cyclophosphamide, hydroxydaunorubicin, vincristine, prednisolone, rituximab chemotherapy regimen. However, his condition deteriorated rapidly and he died in less than 2 months after chemotherapy was started.
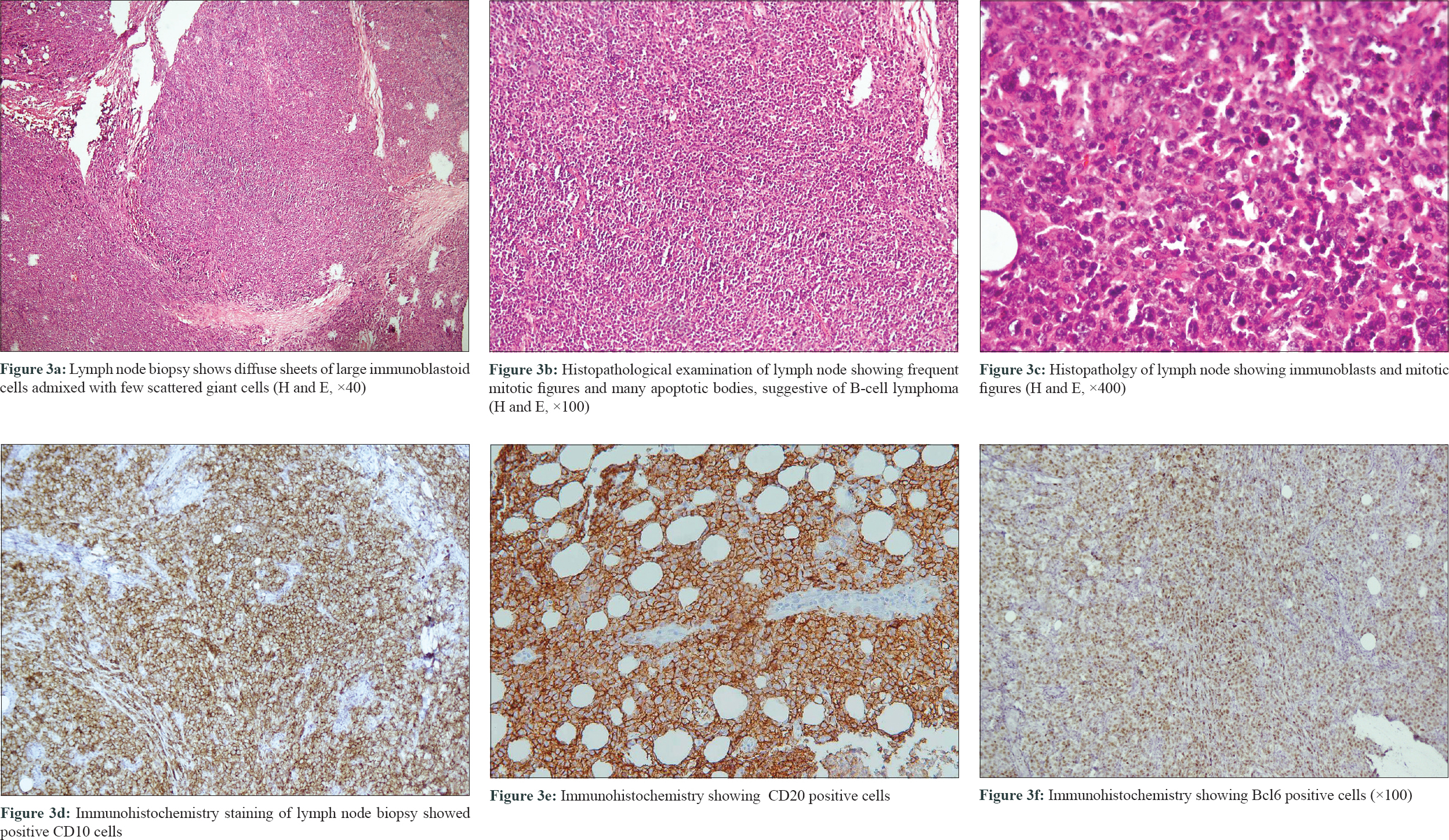 |
| Figure 3 |
Cutaneous noninfectious granulomas developing in association with lymphomas is a well-known phenomenon, that can be categorized into two types.[1] The first type is characterized by finding granulomatous infiltrates in skin lesions composed of neoplastic cells of the lymphoma. In these cases, the granulomatous reactions within tumoral lesions may lead to unusual clinical and histopathological patterns. Examples of this type are granulomatous slack skin or granulomatous infiltrates within cutaneous marginal zone B-cell lymphoma lesions.[2] The second type is development of noninfectious granulomas in organs not involved by lymphoma. In this type, the organs most frequently involved by granulomatous inflammations are lymph nodes, spleen and liver. Skin involvement has very rarely been reported. The correct diagnosis of the underlying lymphoma in this type may be more difficult and challenging because tumoral cells are absent in the granulomatous reaction. As, most commonly, sarcoid-type granulomas have been documented in association with lymphoproliferative diseases, the term “sarcoidosis-lymphoma” was proposed. However, the reported cutaneous granulomas of tuberculoid, palisaded and granuloma annulare-type in association with lymphomas showed that the term “sarcoidosis-lymphoma” is not a proper term.[3] In 2004, three cases of granulomatous skin reactions (tuberculoid type, granuloma annulare-type and sarcoidal type) and lymphomas were reported.[2] Since then, many such cases have been reported in association with lymphomas, and interestingly, these reactions developed both before and after the diagnosis of lymphoma.
Necrobiosis lipoidica is a noninfectious granuloma usually presenting as shiny brown-yellow plaques on the shins that is characterized by collagen degeneration and thickening of blood vessels histologically.[4] Necrobiosis lipoidica is associated with various conditions such as diabetes mellitus, sarcoidosis and rheumatoid arthritis.[5] Ulceration occurs in nearly 30% of cases. To our knowledge, necrobiosis lipoidica has not been reported in association with B-cell lymphoma previously.
Here we reported a case of recalcitrant, ulcerated necrobiosis lipoidica since 3 years, with a recent exacerbation occurring concurrently with the diagnosis of a diffuse large B-cell lymphoma. As various noninfectious granulomas have been reported in association with lymphomas both before and after the diagnosis and our patient had multiple-site granulomatous inflammation in the skin, epididymis and bone marrow, an association of necrobiosis lipoidica-type granulomatous reaction and B-cell lymphoma is another possibility. In other words, our patient may have had an indolent lymphoproliferative disorder that transformed into an aggressive lymphoma concomitant with the exacerbation of necrobiosis lipoidica lesions. Therefore, we recommend considering systemic lymphoma in patients presenting with recalcitrant noninfectious granuloma – in our case necrobiosis lipoidica – especially if systemic symptoms such as cytopenia, or weight loss are present.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Cerroni L. Cutaneous granulomas and malignant lymphomas. Dermatology 2003;206:78-80.
[Google Scholar]
|
| 2. |
Scarabello A, Leinweber B, Ardigó M, Rütten A, Feller AC, Kerl H, et al. Cutaneous lymphomas with prominent granulomatous reaction: A potential pitfall in the histopathologic diagnosis of cutaneous T- and B-cell lymphomas. Am J Surg Pathol 2002;26:1259-68.
[Google Scholar]
|
| 3. |
Rongioletti F, Cerroni L, Massone C, Basso M, Ciambellotti A, Rebora A, et al. Different histologic patterns of cutaneous granulomas in systemic lymphoma. J Am Acad Dermatol 2004;51:600-5.
[Google Scholar]
|
| 4. |
Reid SD, Ladizinski B, Lee K, Baibergenova A, Alavi A. Update on necrobiosis lipoidica: A review of etiology, diagnosis, and treatment options. J Am Acad Dermatol 2013;69:783-91.
[Google Scholar]
|
| 5. |
Sibbald C, Reid S, Alavi A. Necrobiosis lipoidica. Dermatol Clin 2015;33:343-60.
[Google Scholar]
|
Fulltext Views
3,306
PDF downloads
2,272





