Translate this page into:
Ulcerative penile Leishmaniasis in a child
2 Department of Pathology, Harran University School of Medicine, Sanliurfa, Turkey
Correspondence Address:
Yavuz Yesilova
Department of Dermatology, Harran University, Faculty of Medicine, Sanliurfa - 63300
Turkey
| How to cite this article: Yesilova Y, Turan E, S�r�c� HA, Kocarslan S, Tanrikulu O, Eroglu N. Ulcerative penile Leishmaniasis in a child. Indian J Dermatol Venereol Leprol 2014;80:247-249 |
Abstract
Penile ulcers may be caused by several different agents. Rarely, cutaneous leishmaniasis may also be accompanied by penile ulcers. We report a five-year-old boy with who had an ulcer on the glans penis. Smears from the ulcer demonstrated amastigotes, biopsy showed histopathological features of leishmaniasis and Leishmania was grown in culture. Treatment with meglumine antimoniate injections led to improvement.INTRODUCTION
Cutaneous leishmaniasis is a skin disease caused by flagellated protozoa from the Leishmania genus, which are transmitted by sand fly (Dipteran) bites. [1],[ 2] Cutaneous leishmaniasis is more frequently seen on exposed body areas such as the face, eyelids, forehead, hands, wrists and, occasionally, the legs. [2] The involvement of the penis is rare, although there are a few previous reports. [3],[4],[5] We report a five-year-old with cutaneous leishmaniasis of the penis.
CASE REPORT
A five-year-old boy presented with an asymptomatic and persistent ulcer on his penis of six months duration. He was treated with topical steroids, anti-bacterial, anti-scabetic and anti-viral preparations at different times; however, none of these proved effective. There was no family history of similar symptoms.
On examination, a 2 × 3 cm ulcer with a hemorrhagic crust was seen on the glans penis [Figure - 1]. There was mild, painless enlargement of the bilateral inguinal nodes. The C-reactive protein, erythrocyte sedimentation rate, complete blood counts and biochemistry results were normal. Potassium hydroxide (KOH) mount and Tzanck smear prepared from the ulcer discharge were negative.
 |
| Figure 1: A 2 × 3 cm ulcer with hemorrhagic crust on the glans penis |
The Venereal Disease Research Laboratory (VDRL) test, Fluorescent Treponemal Antibody Absorption (FTA-ABS) test and serological tests for herpes simplex virus, cytomegalovirus, Epstein-Barr virus (EBV), Chlamydia trachomatis and human immunodeficiency virus were negative. Giemsa stained smear showed amastigote forms suggestive of Leishmaniasis [Figure - 2]. Promastigotes forms of the parasite were observed in the Novy-MacNeal-Nicole (NNN) culture medium, and skin biopsy from the lesion showed features compatible with cutaneous leishmaniasis [Figure - 3]. The patient received two doses of intramuscular meglumine antimoniate 20 mg/kg, 20 days apart. No complications were noted during treatment. At the 20-day follow-up appointment, the lesion appeared to be healing with a mild scar [Figure - 4].
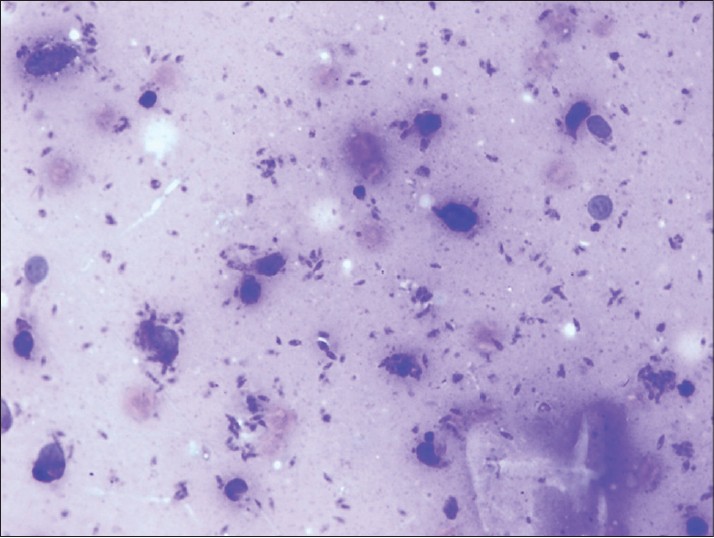 |
| Figure 2: Amastigotes seen in a smear from the ulcer (Giemsa, x100) |
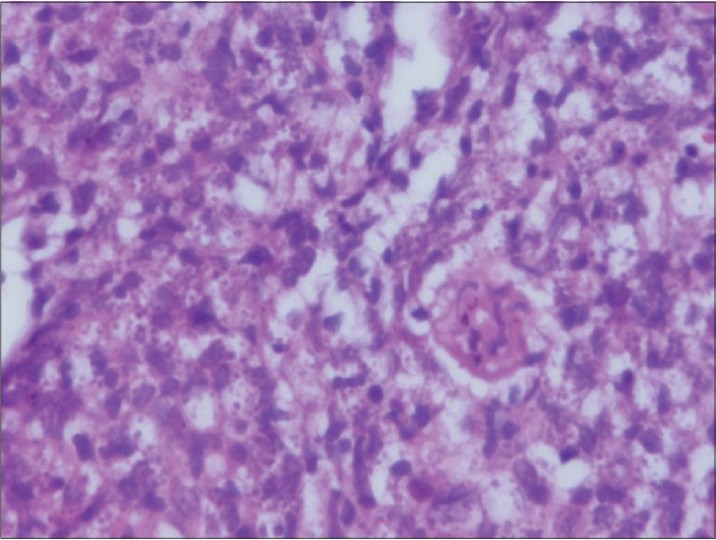 |
| Figure 3: Histopathology of the skin punch biopsy showing numerous macrophages distended with amastigotes (H and E, x1000) |
 |
| Figure 4: Decrease in size of the ulcer after treatment |
DISCUSSION
The etiopathogenesis of penile ulcers includes trauma, viral, bacterial, fungal and parasite infections, neoplasms, auto-immune bullous diseases, immune and systemic diseases, drug reactions and inflammatory and papulosquamous diseases. However, the majority of penile ulcers are caused by sexually transmitted diseases, including syphilis, genital herpes virus infection, lymphogranuloma venereum and donovanosis. Furthermore, non-venereal infections such as candida, Epstein Barr virus, bacteria, parasitic and mycobacterial infections may also cause penile ulcers. Syphilitic chancres are painless and persistent; whereas, ulcers and vesicles caused by genital herpes are painful with a high degree of inflammation. [6] Haemophilus ducreyi causes soft chancre, characterised by painful ulcers with tender lymphadenopathy. As in this case, the great majority of penile lesions are ulcers that are painless and slowly progressive. [5],[7]
Nonsteroidal anti-inflammatory drugs, sulphonamides, penicillin, tetracyclines, anti-epileptics and anti-malarials may also cause erosive and ulcerative drug reactions in the genital mucosa. Inflammatory and papulosquamous diseases such as psoriasis, lichen sclerosus, angiokeratomas, lichen nitidus, lichen planus, Behηet′s disease, Reiter′s syndrome, pyoderma gangrenosum, pemphigus and inflammatory bowel disease may also involve the penile area. Additionally, erythroplasia of Queyrat, squamous cell carcinoma, basal cell carcinoma, extramammary Paget′s disease, lymphoma and leukaemia are neoplastic diseases that cause penile ulcers. Rarely, penile ulcers related to mechanical, chemical, thermal and factitial reasons may also be seen. [6],[7],[8]
The diagnosis of cutaneous leishmaniasis is frequently made clinically. Yet, the demonstration of parasites using laboratory methods is important in terms of ascertaining a diagnosis. [9],[10] The demonstration of amastigotes on Giemsa stain of smears taken from the edge of lesions is the simplest and most effective diagnosis for this disease. [10] The demonstration of plasma cells and Leishmania donovani inside macrophages in the dermis by histopathological examination is another diagnostic tool often employed. [11] In our case, the amastigote form of the parasite was seen in the Giemsa smear and the promastigote form was seen in the culture medium.
In conclusion, cutaneous leishmaniasis should be considered in patients who are travelers to or residents of highly endemic regions in the presence of refractory, chronic lesions on exposed or unexposed areas of the body.
| 1. |
Reveiz L, Maia-Elkhoury AN, Nicholls RS, Romero GA, Yadon ZE. Interventions for American cutaneous and mucocutaneous leishmaniasis: A systematic review update. PLoS One 2013, 8:e61843.
[Google Scholar]
|
| 2. |
Gurel MS, Ulukanligil M, Ozbilge H: Cutaneous leishmaniasis in Sanliurfa: Epidemiologic and clinical features of the last four years (1997-2000). Int J Dermatol 2002, 41:32-37.
[Google Scholar]
|
| 3. |
Schubach A, Cuzzi-Maya T, Goncalves-Costa SC, Pirmez C, Oliveira-Neto MP: Leishmaniasis of glans penis. J Eur Acad Dermatol Venereol 1998, 10:226-228.
[Google Scholar]
|
| 4. |
Grunwald MH, Amichai B, Trau H: Cutaneous leishmaniasis on an unusual site: The glans penis. Br J Urol 1998, 82:928.
[Google Scholar]
|
| 5. |
Castro Coto A, Hidalgo Hidalgo H, Solano Aguilar E, Coto Chacon F: [Leishmaniasis of the genital organs]. Med Cutan Ibero Lat Am 1987, 15:145-150.
[Google Scholar]
|
| 6. |
Bulat V, Situm M, Ljubicic I, Madiraca D: [Wounds in the genital and oral region]. Acta Med Croatica 2012, 66 Suppl 1:109-117.
[Google Scholar]
|
| 7. |
Teichman JM, Sea J, Thompson IM, Elston DM: Noninfectious penile lesions. Am Fam Physician 2010, 81:167-174.
[Google Scholar]
|
| 8. |
Arya M, Kalsi J, Kelly J, Muneer A: Malignant and premalignant lesions of the penis. BMJ 2013, 346:f1149.
[Google Scholar]
|
| 9. |
Gurel MS, Yesilova Y, Olgen MK, Ozbel Y: [Cutaneous leishmaniasis in Turkey]. Turkiye Parazitol Derg 2012, 36:121-129.
[Google Scholar]
|
| 10. |
Kocarslan S, Turan E, Ekinci T, Yesilova Y, Apari R: Clinical and histopathological characteristics of cutaneous Leishmaniasis in Sanliurfa City of Turkey including Syrian refugees. Indian J Pathol Microbiol 2013, 56:211-215.
[Google Scholar]
|
| 11. |
Pehoushek JF, Quinn DM, Crum WP: Cutaneous leishmaniasis in soldiers returning from deployment to Iraq. J Am Acad Dermatol 2004, 51:S197-200.
[Google Scholar]
|
Fulltext Views
4,133
PDF downloads
2,289





