Translate this page into:
Ulceronodular syphilis as the first manifestation of HIV infection
Correspondence Address:
Juan Manriquez
Department of Dermatology, Pontificia Universidad Catolica de Chile, 4686 Vicu�a Mackenna St. Santiago
Chile
| How to cite this article: Navarrete RA, Kellet CV, Manriquez J. Ulceronodular syphilis as the first manifestation of HIV infection. Indian J Dermatol Venereol Leprol 2015;81:224 |
Sir,
Malignant syphilis is a severe and rare manifestation of secondary syphilis and in recent times has been reported mostly in patients with HIV infection. Clinically, the condition is characterized by ulcerated skin lesions covered by thick crusts associated with severe constitutional symptoms. The diagnosis is often difficult and is based on clinical, histological and laboratory parameters.
We report a case of a 25-year-old male who presented with a 3-month history of malaise, fever and asymptomatic nodules all over the body. On examination, the patient had multiple erythematous ulcerated nodules and plaques covered with thick adherent crusts distributed symmetrically on the face [Figure - 1]a, trunk and extremities. The patient also had an indurated ulcer on the penis [Figure - 1]b, and generalized lymphadenopathy. However, there were no other mucosal lesions.
 |
| Figure 1: (a) Symmetrically distributed ulcerated nodules and plaques, covered with thick adherent crusts. (b) Indurated ulcer on penis |
Apart from increased systemic inflammatory response parameters, other routine laboratory tests including complete blood count, liver function tests and urinalysis were normal. The rapid plasma reagin test (RPR) was positive in 512 dilution, and the microhemagglutination antibody assay for Treponema pallidum (MHA-TP) was positive. The HIV ELISA was positive, and the CD4 count was 236/mm 3 . Biopsy from a papulo-nodular lesion showed a dense infiltrate of plasma cells, lymphocytes, and histiocytes. Immunohistochemical staining with monoclonal antibodies revealed T. pallidum in the dermis [Figure - 2]. The cerebrospinal fluid biochemistry, cytology and syphilis serology were negative. He was treated with three doses of benzathine penicillin 2.4 MU, with marked improvement [Figure - 3]. However, the patient did not develop a Jarisch Herxheimer reaction (JHR).
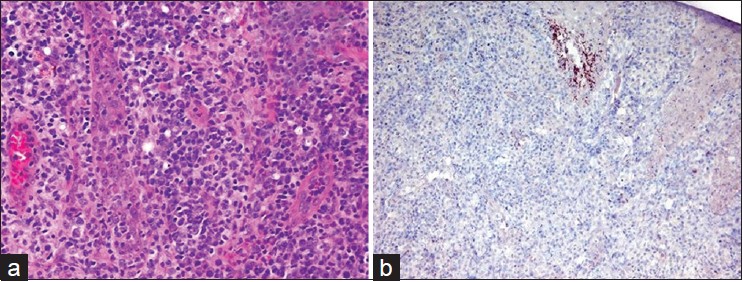 |
| Figure 2: (a) A dense infiltrate of plasma cells admixed with lymphocytes and histiocytes is seen in the dermis (H and E, ×200) (b) Spirochetes highlighted by brown chromogen in the dermis (immunohistochemical stain, ×200) |
 |
| Figure 3: Clinical improvement one week after the treatment with benzathine penicillin |
Syphilis is a chronic, systemic infection that progresses through clinically manifest and latent stages. [1] Although, most patients co-infected with HIV and syphilis develop typical manifestations of syphilis, there are reports of that in some, HIV infection can alter the course of syphilis. [2] One such manifestation is malignant syphilis, a term first used in 1859 by Bazin to to describe a rare form of destructive syphilis, with deeply ulcerating lesions and severe toxemia. [3]
Clinical diagnosis of malignant syphilis is often difficult with several conditions including varicella, herpes simplex, herpes zoster, pityriasis lichenoides et varioliformis acuta, cryptococcocis, coccidioidomycosis, lymphomas, candidiasis and atypical mycobacteriosis entering the differential diagnosis. [2] Diagnostic criteria for malignant syphilis include the presence of a strongly positive RPR titer, characteristic gross and microscopic morphology, a severe Jarisch-Herxheimer reaction on treatment, and rapid resolution of the lesions with antibiotics. In our patient, the diagnosis of malignant syphilis was based on the presence of a positive RPR/MHA-TP titers, clinically characteristic nodulo-ulcerated lesions which revealed a plasma cell-rich inflammatory infiltrate on histopathology, and rapid resolution of the lesions with antibiotics. However, the patient did not develop a Jarisch-Herxheimer reaction.
Our case highlights the important association between malignant syphilis and HIV infection as concurrent HIV infection increases the risk of developing malignant syphilis by 60 times. [4],[5] With a rising global incidence of syphilis in HIV patients, [2] it is essential to be aware of this rare presentation of the disease.
| 1. |
Romero-Jiménez MJ, Suárez Lozano I, Fajardo Picó JM, Barón Franco B. Malignant syphilis in patient with human immunodeficiency virus (HIV): Case report and literature review. An Med Interna 2003;20:373-6.
[Google Scholar]
|
| 2. |
Pérez-Pérez L, Cabanillas M, Ginarte M, Sánchez-Aguilar D, Toribio J. Malignant syphilis in an HIV-infected patient. Actas Dermosifiliogr 2007;98:351-4.
[Google Scholar]
|
| 3. |
Tucker JD, Shah S, Jarell AD, Tsai KY, Zembowicz A, Kroshinsky D. Lues maligna in early HIV infection case report and review of the literature. Sex Transm Dis 2009;36:512-4.
[Google Scholar]
|
| 4. |
Fisher DA, Chang LW, Tuffanelli DL. Lues maligna. Presentation of a case and a review of the literature. Arch Dermatol 1969;99:70-3.
[Google Scholar]
|
| 5. |
Schofer H, Imhof M, Thoma-Greber E, Brockmeyer NH, Hartmann M, Gerken G, et al. Active syphilis in HIV infection: A multicentre retrospective survey. The German AIDS Study Group (GASG). Genitourin Med 1996;72:176-81.
[Google Scholar]
|
Fulltext Views
3,957
PDF downloads
2,997





