Translate this page into:
Undiagnosed purpura: A case of autoerythrocyte sensitization syndrome associated with dermatitis artefacta and pseudo-ainhum
2 Dermatologist, Skin Centre, 5 Air Force Hospital, C/O 99 APO, India
3 Psychiatrist, Base Hospital, Delhi, India
Correspondence Address:
Sandeep Arora
Skin Centre, 5 Air Force Hospital, C/O 99 APO
India
| How to cite this article: Sawhney M, Arora G, Arora S, Prakash J. Undiagnosed purpura: A case of autoerythrocyte sensitization syndrome associated with dermatitis artefacta and pseudo-ainhum. Indian J Dermatol Venereol Leprol 2006;72:379-381 |
Abstract
A 23-year-old young woman presented with recurrent episodes of painful bruising along with linear erosions on the accessible areas of the body of nine years duration with a pseudo-ainhum of her left nipple for the past three months. Her case history included repeated visits to various physicians at different centers and an extensive investigative profile. A diagnosis of autoerythrocyte sensitization was made on the basis of the clinical history, dermatological examination complemented by a positive autoerythrocyte sensitization test, psychiatric evaluation and absence of any organic cause for her ailment. She was placed on psychiatric management and has remained symptom-free after six months follow-up. The case is reported for its rarity, as well as for the association of autoerythrocyte sensitization syndrome with frank dermatitis artefacta and pseudo-ainhum, which to the best of our knowledge has not yet been reported in the literature. |
| Autoerythrocyte sensitization test: interscapular region |
 |
| Autoerythrocyte sensitization test: interscapular region |
 |
| Multiple, monomorphic parallel linear abrasions and ecchymosis right thigh with pseudo-ainhum left nipple (inset) |
 |
| Multiple, monomorphic parallel linear abrasions and ecchymosis right thigh with pseudo-ainhum left nipple (inset) |
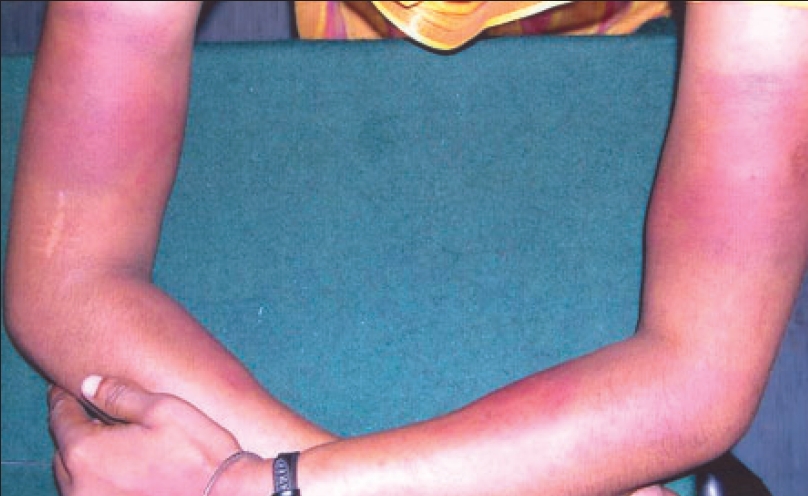 |
| Ecchymosis both arms and forearms |
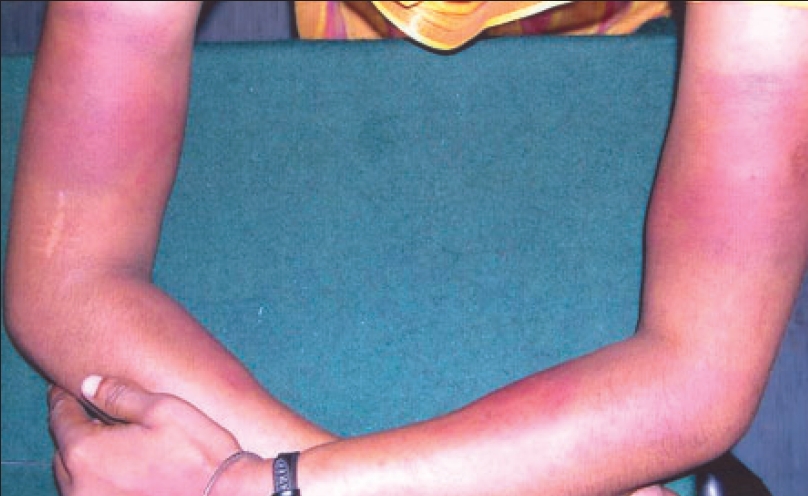 |
| Ecchymosis both arms and forearms |
Introduction
Autoerythrocyte sensitization syndrome (AES), also known as Gardner Diamond syndrome, is a psychologically induced painful bruising condition. The exact etiology of the syndrome is an enigma even today, since its first description in 1955.[1] We describe this rare condition in a young woman with an onset in her early teens, who was subjected to extensive investigations over a period of nine years before her final diagnosis.
Case report
A 23-year-old female patient was referred as a case of myositis with recurrent painful ′spontaneous′ bruising for a period of nine years over her extremities and trunk. Attendant complaints included excoriation of her left nipple and menorrhagia. Historically, the onset of complaints started with acute pain and sudden onset of weakness of all four extremities, followed by spontaneous bruising over both forearms. For the next nine years she was investigated for neurological or hematological abnormality for the unexplained abnormal posturing and recurrent ecchymoses, albeit with no positive results. All neurological investigations were normal. There was a normal hemogram, coagulation profile which included a platelet count, bleeding time, prothrombin time, activated partial thromboplastin time, Von Willebrand factor levels, a negative antinuclear factor, anti ds-DNA, anticardiolipin antibody, lupus anticoagulant, cryoglobulins; and a normal electromyography and muscle biopsy. A hormonal profile and ultrasound of the pelvis for the menorrhagia was also normal.
General and systemic examination was normal. Dermatological examination revealed multiple tender ecchymoses [Figure - 1] and parallel linear abrasions [Figure - 2] present over all the four extremities and anterior abdominal wall. Well-defined circular ulcer at the base of her left nipple had resulted in a partial avulsion of the same resulting in a pseudo-ainhum [Figure - 2]. She denied any history of any self-inflicted injury. There was a history of menorrhagia of seven years duration. However there was no history of epistaxis, hemoptysis, hematuria or blood in stool.
In view of the above, a suspicion of AES with dermatitis artefacta was entertained. To confirm the diagnosis an intradermal test for autoerythrocyte sensitization was done with washed RBCs of the patient in the intrascapular region with a saline control on the opposite side. Within two hours the patient developed a painful ecchymotic reaction, at the site of the injection, similar to the lesions on her extremities. There was no reaction at the control site [Figure - 3]. A skin biopsy revealed a dermal and subcutaneous hemorrhage with an intense acute inflammatory cell infiltrate.
Psychiatric evaluation revealed multiple stressors in her day-to-day life. Psychometric evaluation revealed anxiety features in Rorschach and a need for nurturance and affiliation in Thematic Appreciation Test. An active psychiatric intervention in the form of anxiolytics with buspirone 5mg thrice a day, relaxation measures, family therapy and environmental manipulation was attempted. The patient gradually became more confident and improved on her sick role behavior. The episodes of ecchymoses reduced in frequency and finally stopped after three months. Features of dermatitis artefacta subsided faster with no fresh excoriations observed after one month. The nipple ulcer relapsed once.
Discussion
The historical aspects of AES date back to 1955 when Frank Gardner and Louis Diamond first described four adult women with painful ecchymoses, reproducible after an intradermal injection of the patient′s own RBC and suggested a theory of hypersensitivity to erythrocyte stroma as cause of its occurrence. This condition was named AES.[1] Later, in 1961, Oscar Ratnoff and Agle observed that most such patients had an underlying psychiatric interface and hence named the condition "psychogenic purpura".[2]
AES usually affects adult females.[1],[2],[3] Occasional reports in men and children are present in the literature.[4] Among the various postulated etiological factors, it is now well established that AES occurs in patients with various psychiatric disorders like depression, anxiety, difficulties in handling aggression or obsessive compulsive disorder, among others.[5] Our patient too showed features of anxiety.
The associated complaints in such patients include neurological and ocular symptoms, hemorrhagic manifestations, menorrhagia and a varied symptomatology.[6],[7] Our patient had transient headaches, muscular and joint aches and occasional chest and abdominal pain with her episodes of purpura.
Gardner and Diamond believed that the syndrome was due to autosensitization, as has been proposed for lupus erythematosus. Other causes include a number of hematological and immunological abnormalities.[8],[9] The rapidly developing science of psychoimmunology has revealed the intricacies of the neuroimmunocutaneous endocrine network, which stands as the latest rigid etiological hypothesis.[10] This is a study of the integrated system of the behavior-neuroendocrine system interactions in particular. Communication between the brain and the immune system is bidirectional and mediated by neuropeptides. Although this refutes the theory of autoimmunity as proposed by Gardner and Diamond, it is still hypothetical and needs to be conclusively proven in AES.
The autoerythrocyte sensitization test is a very useful tool to support the diagnosis of AES. It strengthened and confirmed our diagnosis of the case too. We used washed RBC in our test and obtained a positive result. An association with frank dermatitis artefacta and pseudo-ainhum has not been reported. Pseudo-ainhum in our case was a direct result of self-inflicted injury and thus artifactual in origin.
The aim of reporting this rare case was to highlight the importance of looking beyond what′s visible in the patient. The primary complaint of anxiety was never looked into and a concrete diagnosis was never arrived at. Our patient responded well to psychiatric intervention and has now remained symptom-free for six months. She continues to be on anxiolytics and regular psychiatric follow-up.
| 1. |
Gardner FM, Diamond LK. Auto-erythrocyte sensitization. A form of purpura producing painful bruising following autosensitization to red blood cells in certain women. Blood 1955;10:675-90.
[Google Scholar]
|
| 2. |
Ratnoff OD. The psychogenic purpuras: A review of autoerythrocyte sensitization, autosensitization to DNA, "Hysterical" and factitial bleeding and the religious stigmata. Semin Hematol 1980;17:192-213.
[Google Scholar]
|
| 3. |
Chatterjee M, Jaiswal AK. Painful bruising syndrome. Indian J Dermatol Venereol Leprol 2002;68:347-8.
[Google Scholar]
|
| 4. |
Kakihara T, Tanaka A, Imai C, Ikarashi Y, Uchiyama M, Emura I. Psychosomatic reaction exhibiting hemorrhagic erythema and motorsensory disturbance. Pediatr Int 2003;45:472-4.
[Google Scholar]
|
| 5. |
Hallstrom T, Hersle K, Mobacken H. Mental symptoms and personality structure in autoerythrocyte sensitization syndrome. Br J Psychiatr 1969;115:1269-76.
[Google Scholar]
|
| 6. |
Vun YY, Muir J. Periodic painful purpura: Fact or factitious? Aust J Dermatol 2004;45:58-63.
[Google Scholar]
|
| 7. |
Kalla G, Roy R, Purohit DR, Garg A. Painful bruising syndrome. Indian J Dermatol 2001;46:118-9.
[Google Scholar]
|
| 8. |
Fey MF, Beck EA. Psychogenic purpura, idiopathic thrombocytopenic purpura and platelet dysfunction in the same patient. J Clin Psychiatr 1986;47:386-7.
[Google Scholar]
|
| 9. |
Sudy E, Urbina F, Vasquez P. Autoerythrocyte sensitization syndrome with positive anticardiolipin antibodies. Br J Dermatol 1998;138:367-8.
[Google Scholar]
|
| 10. |
Brazzini B, Ghersetich I, Hercogova J, Lotti T. The neuro-immuno-cutaneous-endocrine network: Relationship between mind and skin. Dermatol Ther 2003;16:123-31.
[Google Scholar]
|
Fulltext Views
5,199
PDF downloads
1,745





