Translate this page into:
Unexpected high fluorine-18 fluorodeoxyglucose uptake on positron emission tomography/computed tomography of a benign cellular blue nevus
Corresponding author: Dr. Jun Young Kim, Department of Dermatology, Kyungpook National University Hospital, 130, Dongdeok-ro, Jung-gu, Daegu 41944, South Korea. 198kjy@hanmail.net
-
Received: ,
Accepted: ,
How to cite this article: Lee HJ, Kim JY. Unexpected high fluorine-18 fluorodeoxyglucose uptake on positron emission tomography/computed tomography of a benign cellular blue nevus. Indian J Dermatol Venereol Leprol 2021;87:265-7.
Sir,
Positron emission tomography/computed tomography (PET/ CT) is useful for investigating suspected malignancies. Fluorine-18 fluorodeoxyglucose (18F-FDG) is a tracer used with such studies to detect hypermetabolic lesions and high uptake of 18F-FDG usually indicates the presence of malignancy.1
A 31-year-old female visited the dermatology department, after consulting a breast surgeon, because of an incidental finding of high uptake (standardized uptake value max 6.1) of 18F-FDG by the skin of her left buttock on PET/ CT [Figure 1a] conducted for the staging of her breast cancer. Cutaneous physical examination showed a blue-to-gray, non-fixed, hard mass, measuring 5.5 cm × 4.1 cm on the left buttock [Figure 1b]. She stated that the mass had been present since birth and had persisted without any noticeable change. An incisional biopsy was performed, revealing the mass as a benign blue nevus. Following consultation with a nuclear medicine physician it was understood that the hypermetabolic uptake on PET/CT imaging was localized to a soft tissue lesion of her left buttock rather than a peripheral lesion; therefore, this was considered a true positive finding. However, he could not explain the exact cause of the high uptake. Considering the possibility of malignant change of cellular blue nevus or metastasis of breast cancer, subsequent total excision was performed. We carefully and closely repeated the pathological examination and it showed dense pigmented melanocytic infiltration throughout whole dermis to subcutaneous tissue [Figure 2a]. Even after bleaching of the dense pigmentation there were nearly absent necrosis, mitotic rate more than 1-2/mm2, cytologic atypia, asymmetry and large expansile tumor nests, all featuring benign blue nevus again [Figure 2b]. Various immunohistochemical (IHC) stains including the markers of proliferation and mitosis (focal positive of HMB45, S-100, Melan-A and negative of Ki-67, PHH-3) were used [Figure 2c and d], but we could not find any evidence to suspect melanoma or other malignancies. As cellular blue nevus, atypical cellular blue nevus and blue nevus like melanomas have recently been reported as within the same spectrum, differential diagnosis of them is still subjective.2 By the histologic criteria shown by Hung et al., this case demonstrates two of the findings of atypical cellular blue nevus; size >1cm and cellular crowding, but without cellular atypia.2 It was difficult to define this case obviously as atypical cellular blue nevus. Therefore, we finally diagnosed the lesion as a benign cellular blue nevus showing high uptake of 18F-FDG. We did not perform sentinel lymph node biopsy because of the benign features of the primary lesion. The patient was followed up for 11 months postoperatively without recurrence or metastasis in primary lesion and chest/ abdominal CT imaging studies.
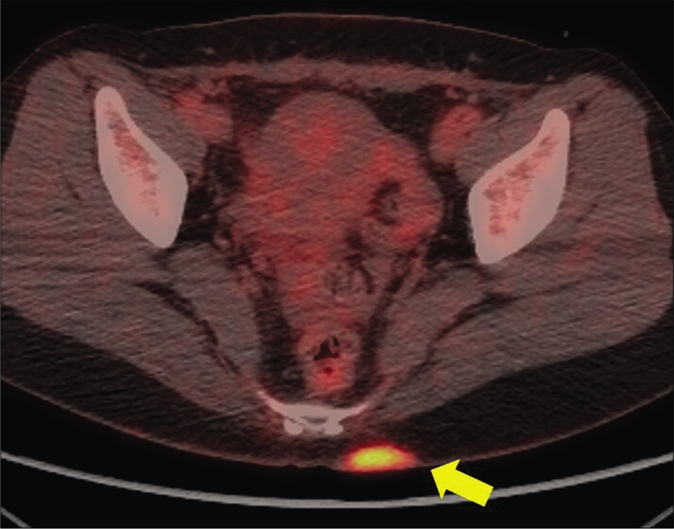
- Positron emission tomography/computed tomography showed high fluorine-18 fluorodeoxyglucose uptake in left buttock (yellow arrow) of breast cancer patient

- A blue-to-gray, non-fixed, hard mass, measuring 5.5 cm × 4.1 cm on left buttock
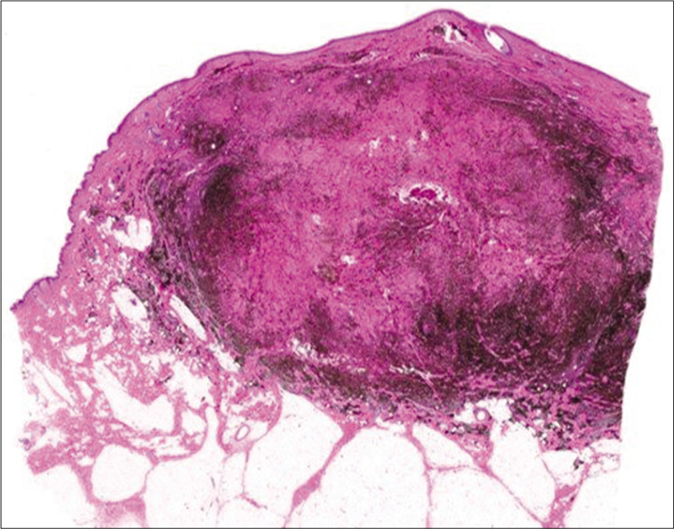
- Dense pigmented melanocytic infiltration throughout whole dermis to subcutaneous tissue (hematoxylin and eosin, ×40)
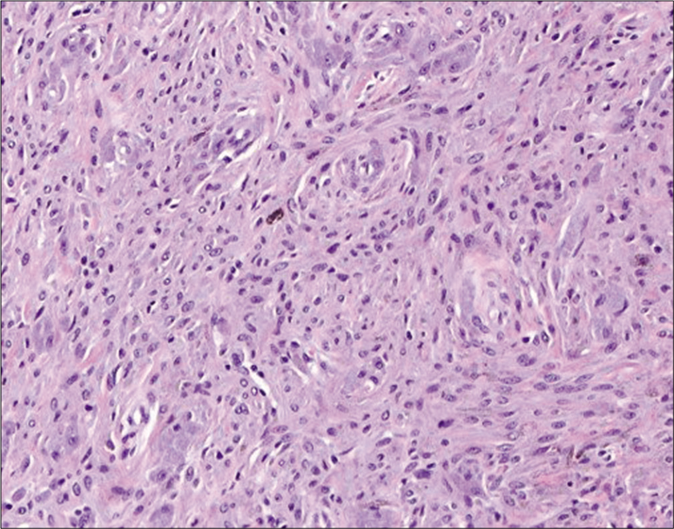
- Even after bleaching the pigment, it showed rare cellular atypia and mitosis (hematoxylin and eosin, ×200)
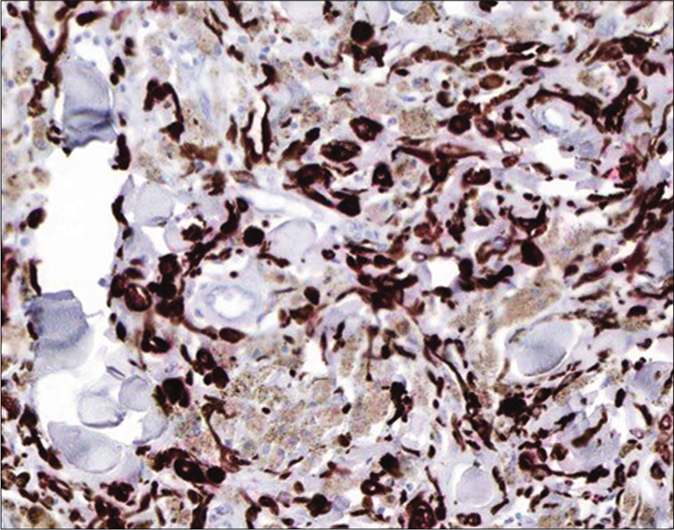
- Melan A focal positivity (Immunohistochemistry with 3-Amino-9-ethylcarbozole chromogen, ×200)
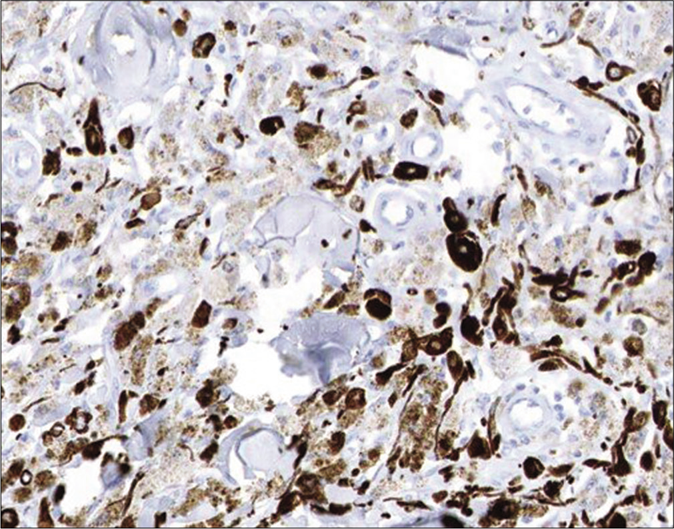
- Absence of Ki-67 (Immunohistochemistry with 3-Amino-9-ethylcarbozole chromogen, ×200)
In PET/CT imaging, FDG, an analog of glucose, is taken up, prevented from being further catabolized and becomes trapped in metabolically active cells.3 As a result, a variety of benign lesions with increased metabolic activity and glucose metabolism, such as inflammatory or infectious cutaneous conditions, are observed as false positives.3 Benign tumors that result in false-positive results include fibrous mesothelioma, schwannoma, aggressive neurofibromas and enchondromas.3 Recently Robinson et al. reported a rare case of benign intradermal nevus yielding a false-positive finding on PET/ CT.4 However, we were unable to find any previous reports of false-positive high uptake of 18F-FDG in a benign blue nevus.
The mechanism by which this case of benign blue nevus resulted in a false-positive 18F-FDG uptake result is unclear. Infiltration of inflammatory cells (neutrophils and activated macrophages) or proliferation of pigmented spindle cells and hypercellularity rather than malignant change or metastasis might have caused alterations in glucose metabolism and accumulation of FDG. Previous research has suggested that idiopathic chromosomal aberrations or genetic mutations associated with melanoma might be one of the possibilities.5 But we could not perform them in this case. The patient strongly refused molecular tests like fluorescence in-situ hybridization or chromosomal aberrations because of the cost and her good prognosis during follow-ups.
A sound understanding of the fundamentals regarding molecular and genetic evaluation for false-positive 18F-FDG uptake of benign skin tumors, including blue nevi, is necessary to avoid misdiagnoses. We may also consider benign blue nevus as possibly one of the skin diseases that can show false positive findings on PET/CT.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
This work was supported by a National Research Foundation of Korea (NRF) grant funded by the Korean government (MSIT) (No. 2018R1C1B5085905).
Conflicts of interest
There are no conflicts of interest.
References
- The role of imaging in the management of patients with nonmelanoma skin cancer: Diagnostic modalities and applications. J Am Acad Dermatol. 2017;76:579-88.
- [CrossRef] [PubMed] [Google Scholar]
- Cellular blue nevomelanocytic lesions: Analysis of clinical, histological, and outcome data in 37 cases. Am J Dermatopathol. 2016;38:499-503.
- [CrossRef] [PubMed] [Google Scholar]
- Common causes of false positive F18 FDG PET/CT scans in oncology. Braz Arch Biol Technol. 2007;50:29-35.
- [CrossRef] [Google Scholar]
- Unexpected positron emission tomography/computed tomography uptake in benign dermal naevus. Australas J Dermatol. 2019;60:e58-60.
- [CrossRef] [PubMed] [Google Scholar]
- Proliferative activity, chromosomal aberrations, and tumor specific mutations in the differential diagnosis between blue nevi and melanoma. Am J Pathol. 2013;182:640-5.
- [CrossRef] [PubMed] [Google Scholar]





