Translate this page into:
Unilateral cutaneous vasculitis: An uncommon presentation and a possible explanation
2 Department of Nephrology, School of Medicine, Marmara University, Istanbul, Turkey
3 Department of Rheumatology, School of Medicine, Marmara University, Istanbul, Turkey
4 Department of Pathology, School of Medicine, Marmara University, Istanbul, Turkey
Correspondence Address:
Burak Tekin
Department of Dermatology, Marmara University Pendik Training and Research Hospital, Mimar Sinan Street, No: 41, Istanbul
Turkey
| How to cite this article: Tekin B, Salman A, Tuglular S, Guler D, Ozen G, Direskeneli H, Ayranci FG, Cinel L, Ergun T. Unilateral cutaneous vasculitis: An uncommon presentation and a possible explanation. Indian J Dermatol Venereol Leprol 2015;81:518-519 |
Sir,
A 41-year-old man with ankylosing spondylitis, familial Mediterranean fever (homozygous M694V mutation) and hypertension was admitted for evaluation of purpuric skin lesions which had appeared on his left ankle 5 days before admission, and rapidly progressed proximally. There was no history of infection or exposure to a new medication as a trigger. His medical history was significant for chronic deep vein thrombosis of the left lower limb diagnosed 3 years ago and treated with oral warfarin. Physical examination showed purpuric papules and plaques covering a large area on the left lower limb, with tense bullae on the lateral aspect of the left leg and severe pitting edema. The right lower limb was normal except for a few dusky macules [Figure - 1]a. On admission, his vital signs were normal except for mild hypertension.
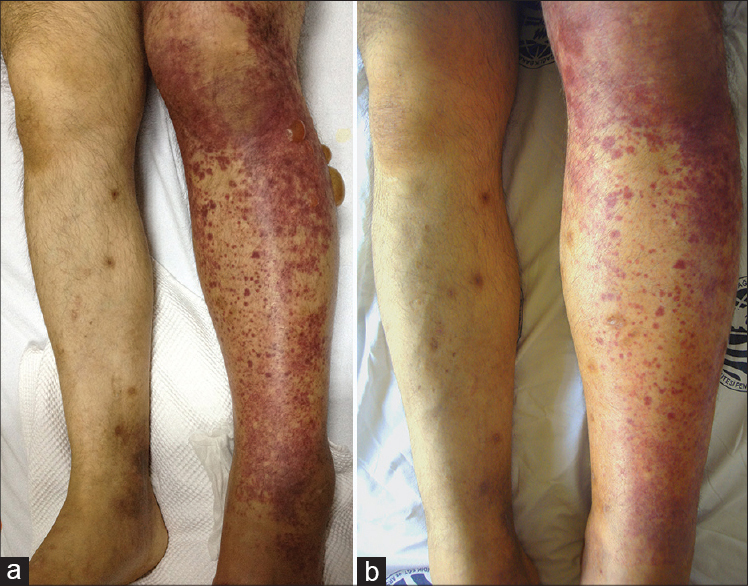 |
| Figure 1: (a) Purpuric papules and plaques with tense bullae on the left lower limb with marked edema (b) Lesions are less pronounced on the 6 th day of treatment |
Laboratory work-up showed elevated serum C-reactive protein (32 mg/l; normal: 0-5), creatinine (2 mg/dl; normal: 0-1.2) and proteinuria (705 mg/day; normal: 50-80). Evaluation for hypercoagulability revealed reduced protein S activity (49%, normal: 89-129) and a heterozygote mutation (C677T) of the MTHFR gene. Signs of intraluminal echogenicity and recanalization were noted in the left deep femoral vein on Doppler ultrasound. Findings on a skin biopsy from a purpuric papule were consistent with leukocytoclastic vasculitis [Figure - 2]. Histopathological examination of a kidney biopsy was consistent with renal amyloidosis and did not show vasculitis. The patient was diagnosed as having cutaneous vasculitis, most probably due to familial Mediterranean fever, and treatment with oral methylprednisolone (0.5 mg/kg/day) was commenced. This dose was maintained for 1 week and then tapered over the next 3 weeks. A progressive resolution of the rash was observed [Figure - 1]b.
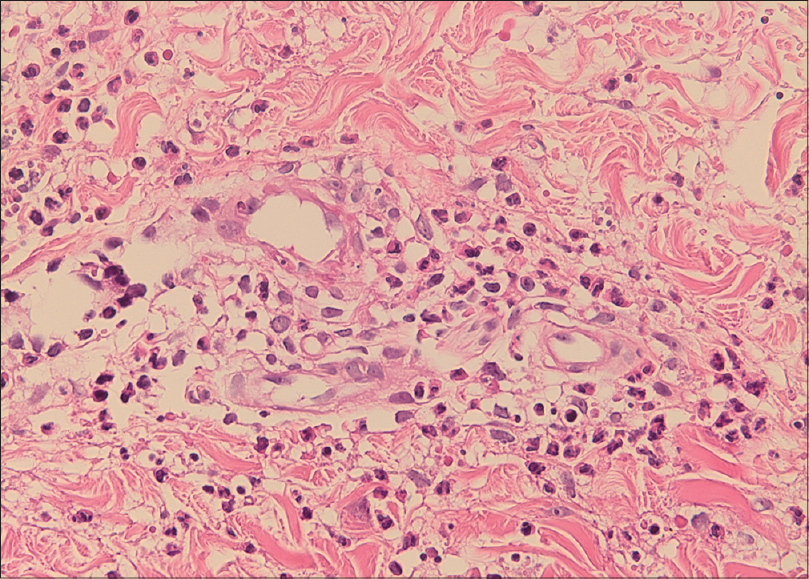 |
| Figure 2: Vessel wall infiltrated with neutrophils, and leukocytoclasia. Endothelial cells are swollen and neutrophils extend into the perivascular area (H and E, ×400) |
Cutaneous small vessel vasculitis classically manifests as palpable purpura due to intense neutrophilic inflammation of the post-capillary venules. Dependent areas of the body such as the lower extremities and sites covered by tight clothing are preferentially involved, indicating the role of hydrostatic pressure and stasis in the pathogenesis. [1] Although symmetrical distribution of lesions is the rule, at least two cases of cutaneous small vessel vasculitis with predominantly unilateral involvement have been reported. In both of these, the relatively spared limb had been kept horizontal due to infection or immobilization, while the more prominently affected limb was in a relatively dependent position. The resulting higher hydrostatic pressure in the latter could explain the asymmetrical involvement. [2],[3]
Familial Mediterranean fever, a hereditary periodic fever syndrome, can influence blood vessels via multiple mechanisms. The association between this disease and the vasculitides can be explained by endothelial cell dysfunction and damage mediated by pro-inflammatory cytokines. Further, an increased incidence of hypercoagulopathy and thrombosis has been observed in familial Mediterranean fever, presumably linked to persistent subclinical inflammation. [4]
Familial Mediterranean fever may have contributed to both the thrombosis and vasculitis in our patient. We hypothesize that the chronic deep vein thrombosis increased the hydrostatic pressure in the left lower limb, leading to unilateral cutaneous vasculitis. This is a presentation clinicians should be aware of, though it remains to be seen if unilateral cutaneous vasculitis can also occur in other conditions affecting local hemodynamics, such as chronic lymphedema or vascular malformations.
| 1. |
Shinkai K, Fox LP. Cutaneous vasculitis. In: Bolognia JL, Jorizzo JL, Schaffer JV, editors. Dermatology. 3 rd ed. China: Elsevier; 2012. p. 385-410.
[Google Scholar]
|
| 2. |
Schattner A, Cohen J. Curious cutaneous vasculitis. Rheumatol Int 2008;28:1281-2.
[Google Scholar]
|
| 3. |
Gershinsky Y, Levi R, Heyman SN. Unilateral purpuric rash in a patient with acute renal failure. Isr Med Assoc J 2011;13:515.
[Google Scholar]
|
| 4. |
Aksu K, Keser G. Coexistence of vasculitides with familial Mediterranean fever. Rheumatol Int 2011;31:1263-74.
[Google Scholar]
|
Fulltext Views
9,061
PDF downloads
2,178





