Translate this page into:
Unilateral naevoid telangiectasia: A retrospective study of 11 paediatric cases
Corresponding author: Dr. Bin Zhang, Department of Dermatology, Beijing Children’s Hospital, Capital Medical University, Xicheng, Beijing, China. dr.binzhang@163.com
-
Received: ,
Accepted: ,
How to cite this article: He R, Zhang N, Guo W, Ma L, Xu Z, Zhang B. Unilateral naevoid telangiectasia: A retrospective study of 11 paediatric cases. Indian J Dermatol Venereol Leprol. 2025;91:217-21. doi: 10.25259/IJDVL_13_2024
Abstract
Background
Unilateral naevoid telangiectasia (UNT) is a rare disease with only sporadic cases reported. The pathogenesis remains elusive and especially in paediatric patients, effective and safe treatment is still uncertain.
Objectives
The purpose of this study was to summarise the clinical characteristics of UNT, explore the possible pathogenesis and evaluate the efficacy and safety of pulsed dye laser (PDL) therapy.
Methods
The epidemiological data, clinical manifestations, laboratory tests and pathological features of paediatric patients with UNT were retrospectively reviewed. PDL treatment was done on some of the patients. Clinical documents and patient images before and after treatment were assessed to evaluate efficacy and adverse events.
Results
Most of the cases (9/11) presented with unilateral lesions. The laboratory results of all the 11 cases were normal. Histological examination in six cases revealed multiple, dilated veins in the reticular dermis. Vascular endothelial growth factor (VEGF) staining was positive, whereas oestrogen receptor staining was negative. Nine cases were treated with PDL which was shown to be effective and safe.
Conclusion
UNT has typical clinical manifestations. The pathogenesis of this disease could be linked to VEGF; however, more research and confirmation are needed. PDL is an effective and safe treatment for UNT.
Keywords
Children
Pulsed dye laser treatment
Pathogenesis
Unilateral naevus telangiectasia
VEGF
Introduction
Unilateral naevoid telangiectasia (UNT) is a rare disease characterised by punctate or stellate telangiectasia scattered in a linear pattern presenting as reddish to purplish macules. Blaschko first characterised it in 1899,1 but only individual cases have been reported since then. Although hypotheses propose developmental abnormality in vascular architecture or hormonal factors, the pathogenesis of UNT is still not fully understood. Each hypothesis has pros and cons of its own. The primary objective of UNT management is to improve cosmesis and this might involve a variety of techniques like electrocautery, cryotherapy and laser therapy. Given the rarity of UNT and the absence of standardised treatment protocols, UNT represents significant diagnostic and therapeutic challenges. Our study has reported 11 cases of UNT in children with detailed clinical data and histopathologic and immunohistochemical analysis of skin lesions. Some children were treated with a PDL to verify its efficacy and safety. Based on the above, clinical evidence for the diagnosis and treatment of UNT will be provided in children.
Methods
Study design
This is a retrospective, observational case series to explore the possible pathogenesis of UNT and summarise its clinical features and treatment with PDL. The study was approved by the institutional review and ethics board of Beijing Children’s Hospital, Capital Medical University ([2022]-E-028-Y).
Clinical data
Children diagnosed with UNT who presented at our clinic from September 2020 to September 2023 were reviewed with detailed records of demographic information, medical history, cutaneous manifestations and dermoscopic photos. All children needed to complete laboratory tests of sex hormones, liver function, viral hepatitis antibodies and thyroid function. Children who were willing to complete the invasive examination and whose guardians signed the informed consent completed the histopathological and immunohistochemical examination of skin lesions.
PDL treatment
Signed informed consent was obtained from guardians of the children who received PDL treatment. Therapeutic parameters were laser wavelength of 595 nm, pulse width of 1.5–3.0 ms, spot diameter of 7 mm and energy of 8.75–11.75J/cm2. Each spot only passed through once and avoided overlapping between the spots. Each time before treatment, the lesions were photographed and the laser device settings were recorded afterwards. The patients were followed for 1 month after the treatment and photographed. The next treatment was decided according to the effect of the previous treatment. But overall, given that it was an observational study, the number of courses mainly depended on the preference of patients and guardians. The interval between the two treatments was 4–6 weeks. Treatment efficacy was assessed by comparing photographs of the lesions by two dermatologists and resolving any discrepancies by consensus. Efficacy was graded according to the degree of lightening as: Grade IV corresponds to less than 25%; Grade III corresponds to between 25 and 49%; Grade II corresponds to between 50 and 75%; and Grade I corresponds to more than 75%.2
Results
The details of 11 patients are shown in Table 1.
| Patient | Sex | Age (years) | Age of onset (years) | Site | Histopathological examination | PDL | PDL courses | PDL efficacy | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Neck | Trunk | Upper limb | Lower limb | ||||||||||||
| 1 | Man | 10.8 | 8 | - | - | - | - | L | - | - | - | + | + | 2 | Grade I |
| 2 | Woman | 10.8 | 8 | - | - | - | - | - | - | - | R | + | + | 4 | Grade I |
| 3 | Woman | 2.1 | 0 | - | - | - | - | - | R | - | - | - | + | 2 | Grade II |
| 4 | Man | 5.2 | 0 | - | - | L | R | - | R | - | - | + | + | 2 | Grade II |
| 5 | Woman | 6.3 | 0 | - | - | - | - | L | - | - | - | - | + | 5 | Grade I |
| 6 | Woman | 4 | 0 | - | - | - | R | - | R | - | - | - | + | 2 | Grade III |
| 7 | Man | 10.3 | 0 | - | - | - | - | - | R | - | R | + | - | - | - |
| 8 | Man | 10.1 | 10 | L | - | L | - | L | - | L | R | + | - | - | - |
| 9 | Woman | 13 | 10 | - | - | - | - | - | R | - | - | + | + | 2 | Grade II |
| 10 | Woman | 7.8 | 0 | - | - | - | - | - | R | - | - | - | + | 2 | Grade III |
| 11 | Woman | 9 | 4 | - | - | - | - | - | - | L | - | - | + | 2 | Grade II |
General information
In this study, 11 paediatric patients with UNT were enrolled—four men and 7 women. Six patients were grouped as congenital UNT and five patients were grouped as acquired UNT with an average onset of 8 years of age. The family history was unremarkable. All the children exhibited normal growth and development.
Cutaneous manifestations
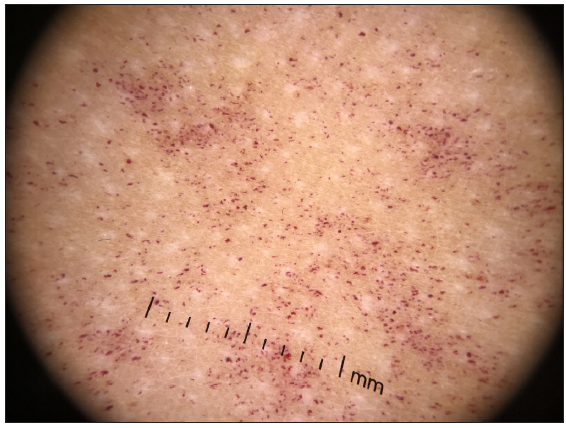
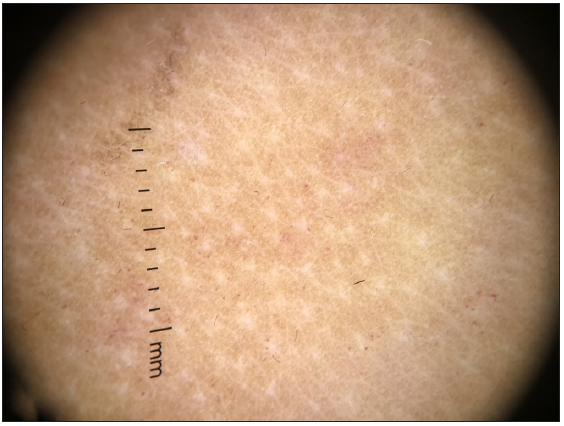
Nine patients had unilateral lesions, whereas the other two were bilateral. Limb involvement could be observed in all the patients with ipsilateral neck, thorax or back affected in three patients. Parents of these children noted that the lesions were modest in the early stages of the disease, but subsequently became larger and longer, eventually revealing a band. The characteristic of lesions were light pink patches of 1–2 cm in diameter, distributed in a linear pattern. Discrete punctate or stellate telangiectasia could be spotted [Figure 1a]. The dermatoscopy revealed dotted or round vessels on a light red background which faded under local pressure [Figure 1b]. The lesions’ skin temperature was normal with no aberrant pulsation or tremor.
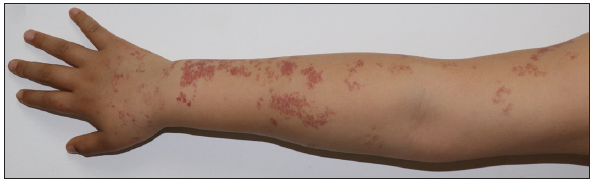
- Banded telangiectasia patches on the right upper limb of patient 10.
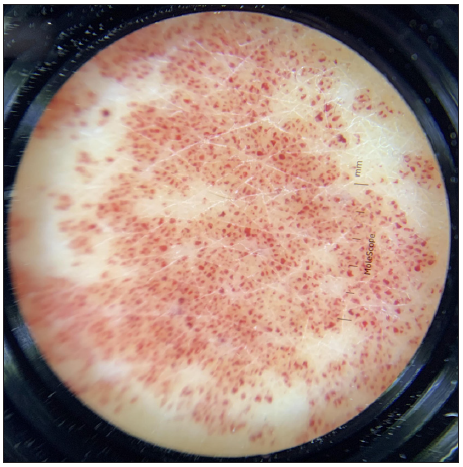
- Dotted vessels on a light red background under dermoscopy (MoleScope, polarised light, 4x).
Laboratory examinations
The results of laboratory tests of all our patients were normal. The histopathological examination of skin lesions in six children revealed tortuose, enlarged capillaries in the dermis without capillary wall thickening or vascular endothelial cell proliferation [Figure 1c]. Negative oestrogen receptor staining [Figure 1d] and positive Vascular endothelial growth factor (VEGF) staining [Figure 1e] were found in immunohistochemistry.
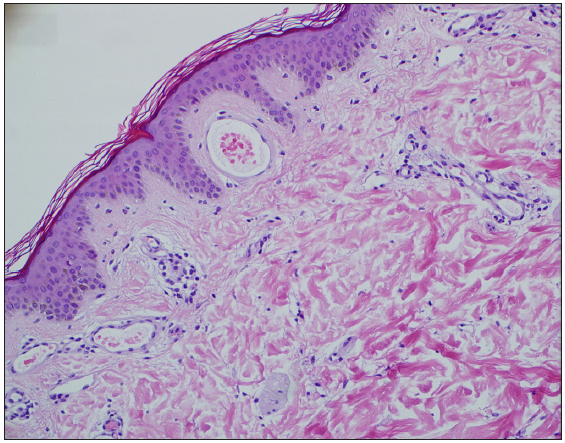
- Enlargement of thin-walled capillaries in the dermis, but no capillary wall thickening or vascular endothelial cell proliferation (Haematoxylin-eosin staining, 200x).
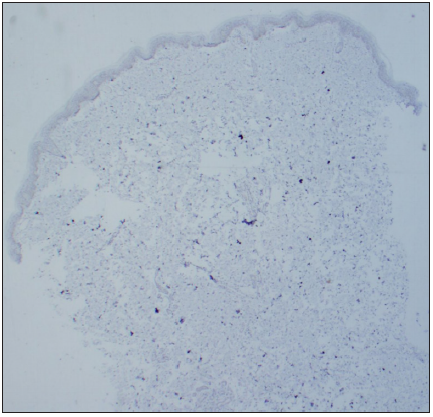
- Negative oestrogen receptor staining (50x).
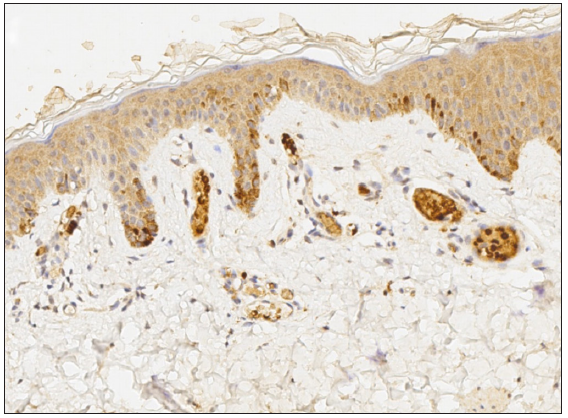
- Positive vascular endothelial growth factor staining (200x).
Laser treatment
PDL was used to treat nine patients. Three patients (33.3%) achieved Grade I efficacy [Figure 2 and 3], four patients (44.4%) achieved Grade II efficacy and two patients (22.3%) achieved Grade III efficacy. After PDL treatment, one patient had pigmentation which resolved after 3 months of sun protection.

- Skin lesions of patient 1 before treatment.

- Skin lesions of patient 1 after treatment.
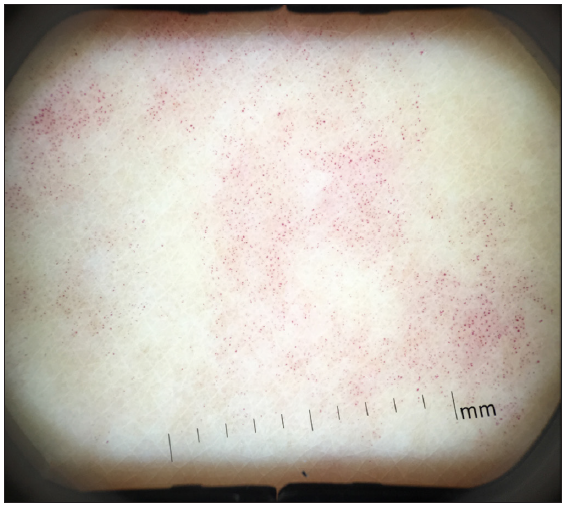
- Dermatoscopic findings before treatment (DermaScope, polarised light, 8x).
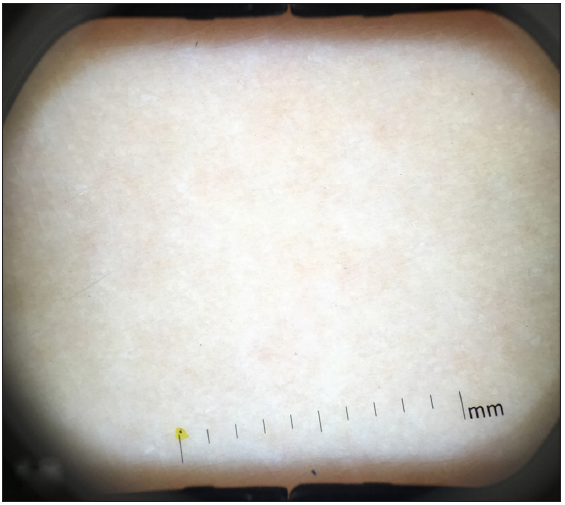
- Dermatoscopic findings after treatment (DermaScope, polarised light, 8x).
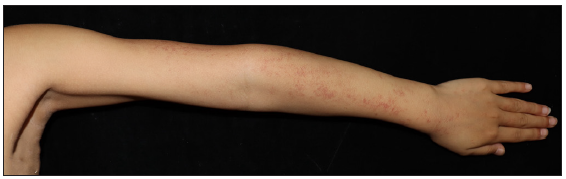
- Skin lesions of patient 5 before treatment.

- Skin lesions of patient 5 after treatment.
- Dermatoscopic findings before treatment (DermLite, polarised light, 10x).
- Dermatoscopic findings after treatment (DermLite, polarised light, 10x).
Discussion
UNT can be subtyped into congenital and acquired types, according to the age of onset. Wenson’s review of nearly 100 UNT literature has indicated that congenital type accounts for roughly 16% with a man-to-woman incidence ratio of almost 1:2,3 which is comparable to that of our study. Six of our 11 patients were congenital, whereas the other 5 were acquired. Given that all our patients were children, the proportion of congenital UNT in the population of children should be higher.
UNT is typically characterised by stripes of dilated capillary macules and patches with distinct edges which disappear under local pressure. Many of the cases present with unilateral lesions along the Blaschko line, while bilateral cases have also been reported. The pathological features include tortuous dilated capillaries in the upper dermis without aberrant vascular endothelial cell proliferation. In dermoscopic examination, UNT typically manifests as dotted or globular vessels on a reddish background. The diagnosis of UNT is made based on the clinical characteristics.
UNT’s pathogenesis is yet unknown. Approximately half of the cases are linked to puberty or pregnancy,3 and some UNT acquired during pregnancy can spontaneously resolve after delivery.4 The positive staining for oestrogen receptors in lesional immunohistochemistry further supported the fact that the pathogenesis of UNT is linked to oestrogen.5 However, the previous positive results were acquired via a unique radiolabeling technique which cannot be recapitulated by other labs.6,7 The results of oestrogen receptor staining in our study were all negative which raised the question of the role of oestrogen in the pathogenesis of UNT.
It has also been postulated that the oestrogen receptors in the lesions of UNT patients are abnormally hypersensitive and that congenital UNT is generated by the stimulation of high levels of maternal oestrogen or progesterone. Acquired UNT develops during puberty or pregnancy due to hormonal changes.8 In addition, for some patients with liver illness or thyroid malfunction, the increased oestrogen in the serum may contribute to the UNT phenotype.9 However, this theory has been challenged. Cunliffe et al. gave oestrogen cream topically to a woman with acquired UNT during pregnancy, after the delivery skin lesions had disappeared and there was no recurrence in an artificially high oestrogen environment.10 Many cases of UNT have also been reported in healthy individuals.11 Of the five acquired UNT patients in this study, there was one pubertal girl and four prepubertal boys. None had aberrant serum oestrogen levels, or deranged liver or thyroid function tests. More studies are needed to determine whether oestrogen is the primary cause of UNT.
Some researchers have argued that UNT is a type of mosaicism created by somatic mutation during embryonic development12 based on the fact that the skin lesions are distributed along the Blaschko line. VEGF stimulates vascular development as a critical regulator of physiological and pathological angiogenesis and it is thought to be involved in the mechanism of UNT. Turan et al. propose that the telangiectasias may result from elevated serum levels of angiogenic factors like VEGF.13 Smith et al. described a UNT patient with chronic hepatitis C virus infection who showed increased positive VEGF staining in the skin lesions.14 The positive stain for VEGF in our study further supports the role of VEGF in the pathogenesis of UNT. Further verifying the uniqueness of VEGF in UNT, we biopsied other capillary malformations such as port-wine stain lesions and processed them with VEGF immunohistochemical staining. The results were negative. Considering this, we assume that VEGF immunohistochemical staining can be a critical tool in identifying UNT and other capillary malformations.
Medical intervention is usually not necessary for UNT patients, except for cosmetic concerns. In such cases, PDL therapy can be considered. The location of the dilated capillaries is more superficial in UNT and better treatment response can be expected compared with those of other capillary malformations such as port-wine stains. In this study, nine cases underwent PDL with a total significant efficiency of 77.7% (Grade I and Grade II) which is similar to previous research.15 The only side effect is a transient pigmentary change. It is considered to be related to larger vessel diameter and more vascular branches. For patients with poor response to PDL treatment, haemoprotein photodynamic therapy can be used to selectively destroy malformed blood vessels.16
Conclusion
UNT has typical clinical manifestations. The pathogenesis of this disease could be linked to VEGF; however, more research and confirmation are needed. The treatment of UNT with PDL is both successful and safe.
Ethical approval
The study was approved by the Institutional Review and Ethics Board of Beijing Children’s Hospital, Capital Medical University ([2022]-E-028-Y).
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Teleangiektasien versammlungen berliner dermatologische gesellschaft. Monatsschr Prakt Dermat. 1899;28:451.
- [Google Scholar]
- Can the response of port-wine stains to laser treatment be reliably assessed using subjective methods? Br J Dermatol. 2000;143:360-4.
- [CrossRef] [PubMed] [Google Scholar]
- Unilateral nevoid telangiectasia syndrome: A case report and review of the literature. Dermatol Online J. 2011;17:2.
- [Google Scholar]
- Unilateral nevoid telangiectasia: A condition unmasked by hyperoestrogenism? Eur J Dermatol. 2017;27:439-41.
- [CrossRef] [PubMed] [Google Scholar]
- Unilateral nevoid telangiectatic syndrome. The role of estrogen and progesterone receptors. Arch Dermatol. 1983;119:226-8.
- [CrossRef] [PubMed] [Google Scholar]
- Unilateral nevoid telangiectasia on the lower extremity of a pediatric patient. J Am Acad Dermatol. 2010;62:528-30.
- [CrossRef] [PubMed] [Google Scholar]
- Unilateral nevoid telangiectesia: Report of two pediatric cases. Turk J Pediatr. 2015;57:635-8.
- [PubMed] [Google Scholar]
- Image Gallery: Unmasking of unilateral naevoid telangiectasia during puberty. Br J Dermatol. 2018;178:e331.
- [CrossRef] [PubMed] [Google Scholar]
- Acquired unilateral nevoid telangiectasia accompanied by liver metastasis of colon cancer. Ann Dermatol. 2016;28:404-5.
- [CrossRef] [PubMed] [Google Scholar]
- Unilateral nevoid telangiectasia in a healthy man. Case Rep Dermatol. 2021;13:330-5.
- [CrossRef] [PubMed] [Google Scholar]
- Acquired unilateral nevoid telangiectasia syndrome accompanied by chronic hepatitis B virus infection. Acta Dermatovenerol Croat. 2013;21:133-4.
- [PubMed] [Google Scholar]
- Unilateral nevoid telangiectasia syndrome (UNTS) associated with chronic hepatitis C virus and positive immunoreactivity for VEGF. Dermatol Online J. 2014;20:13030/qt8g9268sf.
- [PubMed] [Google Scholar]
- Unilateral nevoid telangiectasia--response to PDL. Int J Dermatol. 2006;45:960-4.
- [CrossRef] [PubMed] [Google Scholar]
- Hemoporfin photodynamic therapy for a case of unilateral nevoid telangiectasia. Chin Med J (Engl). 2020;134:1245-7.
- [CrossRef] [PubMed] [Google Scholar]






