Translate this page into:
Unilateral nevoid telangiectasia with no estrogen and progesterone receptors in a pediatric patient
2 Department of Pathology, Dr. Behcet Uz Children's Hospital, Izmir, Turkey
Correspondence Address:
F Sule Afsar
2040 Sok. Kugu 122 D:50, 35540 Mavisehir Karsiyaka Izmir
Turkey
| How to cite this article: Afsar F S, Ortac R, Diniz G. Unilateral nevoid telangiectasia with no estrogen and progesterone receptors in a pediatric patient. Indian J Dermatol Venereol Leprol 2008;74:163-164 |
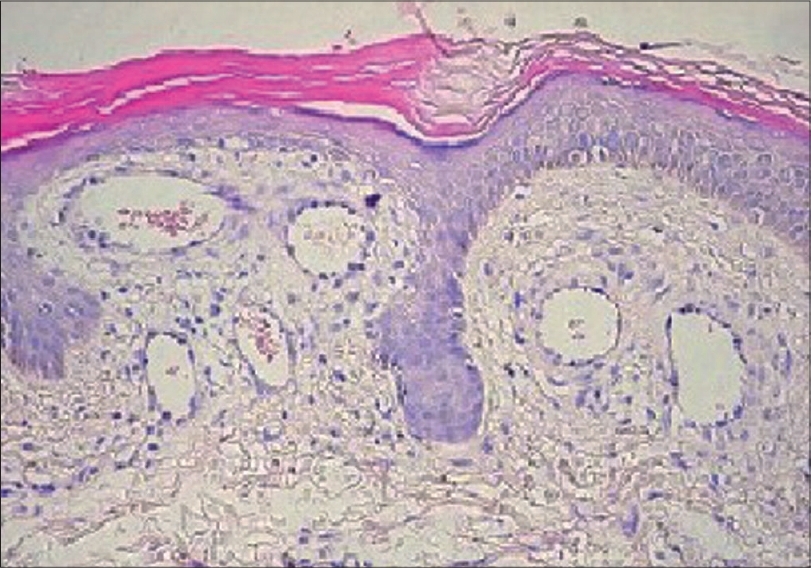 |
| Figure 3: Dilated vessels without endothelial proliferation and vasculitis in the papillary dermis (H and E stain, �400) |
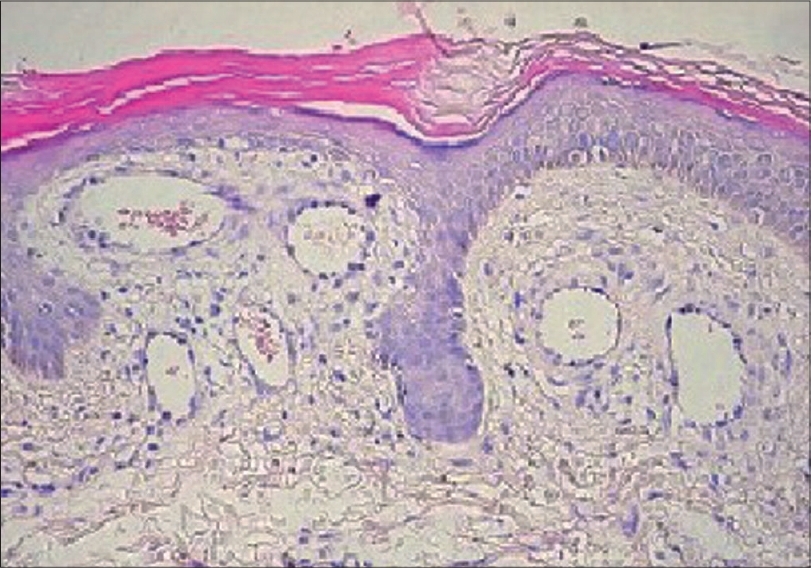 |
| Figure 3: Dilated vessels without endothelial proliferation and vasculitis in the papillary dermis (H and E stain, �400) |
 |
| Figure 2: Dorsal appearance of multiple telangiectasia involving the skin overlying T1-T3 dermatomal areas |
 |
| Figure 2: Dorsal appearance of multiple telangiectasia involving the skin overlying T1-T3 dermatomal areas |
 |
| Figure 1: Ventral appearance of multiple telangiectasia involving the skin overlying T1-T3 dermatomal areas |
 |
| Figure 1: Ventral appearance of multiple telangiectasia involving the skin overlying T1-T3 dermatomal areas |
Sir,
Unilateral nevoid telangiectasia (UNT) is characterized by the dermatomal distribution of telangiectasia, which are distributed unilaterally and frequently found in C3-C4 or the trigeminal dermatomal areas. [1] UNT may be congenital or acquired. Acquired UNT may occur coincident with physiologic states of estrogen increase, including puberty and pregnancy in women and adrenarche in men. Acquired UNT may also occur in estrogenized pathologic states, such as chronic hepatic disease in alcoholism. [2] We describe a case of UNT that had no evidence of estrogen or progesterone receptor expression in a 9-year-old girl.
A 9-year-old girl presented with multiple asymptomatic red spots that had firstly appeared on the skin of the inner aspect of the right lower arm at the age of 1½ and continued to spread on the ventral aspect of the right upper arm, periaxillary area and the upper back involving the dermatomes of T1-T3 [Figure - 1],[Figure - 2].
General examination was unremarkable. Multiple blanchable telangiectatic macules were present over the medial arm, periaxillary and scapular areas. An incisional biopsy showed numerous dilated and congested thin-walled small to medium sized blood vessels in the papillary dermis. The vessels were lined by bland flat endothelial cells without any endothelial proliferation or inflammatory infiltration [Figure - 3]. Based on clinical appearance and histopathological findings, a diagnosis of UNT was made. Because the parent of the patient did not accept to have determined her serum estrogen and progesterone levels and the serologic tests for hepatitis B and C, streptavidin biotin complex method was applied for immunohistochemical analysis. Diaminobenzidine was used as chromogen. Immunohistochemical stains for estrogen (DAKO, Denmark, M7047) and progesterone receptors (DAKO, Denmark M3569) were negative in the endothelial cells of the UNT.
The parent refused pulse dye laser treatment, and the patient was lost to follow-up.
UNT is a cutaneous condition mostly involving the trigeminal nerve distrubution or the C3, C4 or adjacent dermatomes. The histopathology of UNT is characterized by dilated capillaries in the upper and mid-dermis. [2] Without endothelial proliferation UNT has been reported to be associated with hyperestrogenemic states such as puberty, pregnancy and alcoholism. [2],[3],[4],[5] This is explained by the hypothesis that a humoral agent, probably estrogen, stimulates the end target organs that are distributed congenitally in a dermatomal pattern in order to produce telangiectasia. [2]
There are a few cases of UNT with serologic evidence of hepatitis C supporting the hormonal theory, which is based on hyperestrogenemic state, but this theory does not apply in all UNT cases. [6],[7] Cases of UNT occurring in the presence of normal serum estrogens and liver function are documented in literature. [8],[9],[10] Tok et al. reported a case of UNT related to pregnancy with no estrogen and progesterone receptors, and suggested that the receptor assays were not sensitive enough to detect estrogen and progesterone levels in the skin when compared with the breast tissue. [11]
It is known that normal skin contains low levels of estrogen receptors and it is difficult to explain the lack of estrogen receptors in case of increased circulating estrogen. [12] Although we were not able to report the serum estrogen and progesterone levels of our patient, the lack of estrogen and progesterone receptors supports the theory that physiologic hormonal or hyperestrogenemic states do not always apply for the etiopathogenesis of the UNT. It was suggested that UNT might result from a somatic mutation in the presence of normal hormonal status, [2] but further data need to be supplied for its pathogenesis.
| 1. |
Blaschko A. Telangiektasien. Versammlungen. Berliner Dermatologische Gesellschaft. Monatschr Prakt Dermat 1899;28:451.
[Google Scholar]
|
| 2. |
Wilkin JK, Smith JG Jr, Cullison DA, Peters GE, Rodriquez-Rigau LJ, Feucht CL. Unilateral dermatomal superficial telangiectasia. Nine new cases and a review of unilateral dermatomal superficial telangiectasia. J Am Acad Dermatol 1983;8:468-77.
[Google Scholar]
|
| 3. |
Sanchez Conejo-Mir J, Ortega Resina M, Camacho Martinez F. Unilateral nevoid telangiectasia syndrome: Study of cutaneous estrogen receptors. Med Cutan Ibero Lat Am 1984;12:469-75.
[Google Scholar]
|
| 4. |
Uhlin SR, McCarty KS. Unilateral nevoid telangiectatic syndrome: The role of estrogen and progesterone receptors. Arch Dermatol 1983;119:226-8.
[Google Scholar]
|
| 5. |
Woollons A, Darley CR. Unilateral naevoid telangiectasia syndrome in pregnancy. Clin Exp Dermatol 1996;21:459-60.
[Google Scholar]
|
| 6. |
Hynes LR, Shenefelt PD. Unilateral nevoid telangiectasia: occurence in two patients with hepatitis C. J Am Acad Dermatol 1997;36:819-22.
[Google Scholar]
|
| 7. |
Taskapan O, Harmanyeri Y, Sener O, Aksu A. Acquired unilateral nevoid telangiectasia syndrome. Acta Derm Venereol 1997;77:62-3.
[Google Scholar]
|
| 8. |
Jucas JJ, Rietschel RL, Lewis CW. Unilateral nevoid telangiectasia. Arch Dermatol 1979;115:359-60.
[Google Scholar]
|
| 9. |
Karakas M, Durdu M, Sonmezoglu S, Akman A, Gumurdulu D. Unilateral nevoid telangiectasia. J Dermatol 2004;31:109-12.
[Google Scholar]
|
| 10. |
Duong MH, Raymond GP. Unilateral dermatomal superficial telangiectasia. Can Med Assoc J 1983;129:1117-8.
[Google Scholar]
|
| 11. |
Tok J, Berberian BJ, Sulica VI. Unilateral nevoid telangiectasia syndrome. Cutis 1994;53:53-4.
[Google Scholar]
|
| 12. |
Hasselquist MB, Goldberg N, Schroeter A, Spelsberg TC. Isolation and characterization of the estrogen receptor in human skin. J Clin Endocrinol Metab 1980;50:76-82.
[Google Scholar]
|
Fulltext Views
3,735
PDF downloads
3,329





