Translate this page into:
Unusual targetoid nodule on the back
2 Department of Pathology, Facultad de Medicina, Pontificia Universidaad Católica de Chile, Santiago, Chile
Corresponding Author:
Camila Downey
Department of Dermatology, Facultad de Medicina, Pontificia Universidad Católica de Chile, Santiago
Chile
camiladowney@gmail.com
| How to cite this article: Garc�a-Huidobro I, Ábarzúa-Araya A, Downey C, González S. Unusual targetoid nodule on the back. Indian J Dermatol Venereol Leprol 2017;83:408-410 |
A 28-year-old woman presented with an asymptomatic recurrent nodule on her back for 6 months. The lesion was increasing in size and the patient noted variations in the nodule's color from pink to light brown. On examination, a non-tender, red to violaceous nodule with a thin pale brown margin and a peripheral ecchymotic ring measuring 1.6 cm × 1 cm was seen on the right posterior shoulder [Figure - 1]. The remainder of the dermatological examination was unremarkable.
 |
| Figure 1: An erythemato-violaceous, non-tender, central nodule surrounded by a thin pale brown area and a peripheral ecchymotic ring measuring 1.6 cm × 1 cm on the right posterior shoulder |
An excisional biopsy showed dilated vascular channels in the papillary dermis with a lining of prominent endothelial normotypic cells. Extravasated erythrocytes and perivascular superficial mononuclear inflammatory infiltrate were also seen [Figure - 2]. Immunohistochemistry revealed intense positive reaction for the lymphatic endothelial cell marker podoplanin (D2–40) [Figure - 3]. Perl's stain was also positive [Figure - 4]. The study was negative for Wilms' tumor 1 gene.
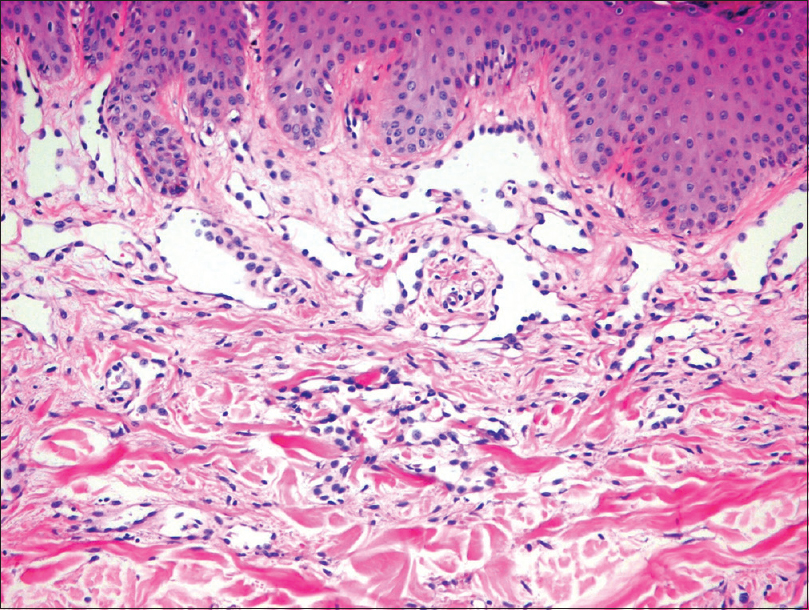 |
| Figure 2: Dilated vascular channels in papillary dermis with a lining of prominent endothelial normotypic cells. Extravasated erythrocytes and perivascular superficial mononuclear inflammatory infiltrate and hemosiderophages were also found (H and E, ×100) |
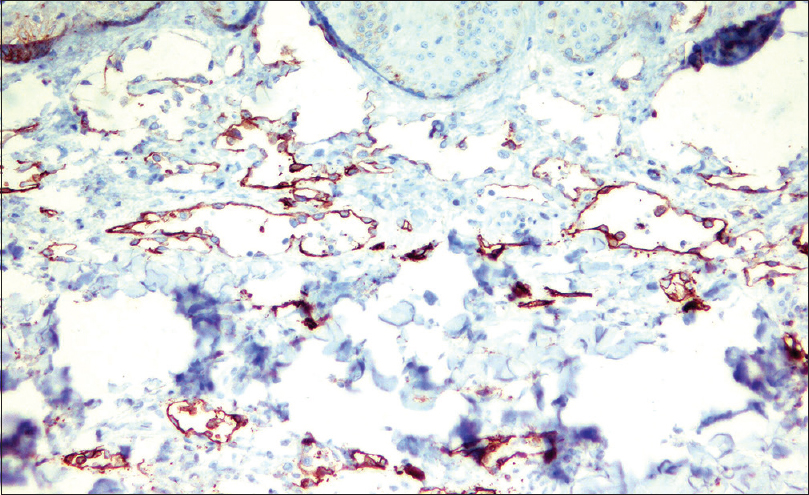 |
| Figure 3: Immunohistochemical study showed intense positive reaction for the lymphatic endothelial cell marker podoplanin (D2– 40, ×100) |
 |
| Figure 4: Isolated hemosiderophages around blood vessels at the periphery of the lesion (Perl's stain, ×400) |
What Is Your Diagnosis?
| 1. | Trindade F, Kutzner H, Tellechea Ó, Requena L, Colmenero I. Hobnail hemangioma reclassified as superficial lymphatic malformation: A study of 52 cases. J Am Acad Dermatol 2012;66:112-5. [Google Scholar] |
| 2. | Carlson JA, Daulat S, Goodheart HP. Targetoid hemosiderotic hemangioma – A dynamic vascular tumor: Report of 3 cases with episodic and cyclic changes and comparison with solitary angiokeratomas. J Am Acad Dermatol 1999;41(2 Pt 1):215-24. [Google Scholar] |
| 3. | Joyce JC, Keith PJ, Szabo S, Holland KE. Superficial hemosiderotic lymphovascular malformation (hobnail hemangioma): A report of six cases. Pediatr Dermatol 2014;31:281-5. [Google Scholar] |
| 4. | Gendernalik SB, Gendernalik JD. Recurrent targetoid hemosiderotic hemangioma in a 26-year-old man. J Am Osteopath Assoc 2011;111:117-8. [Google Scholar] |
| 5. | Hejnold M, Dyduch G, Mojsa I, Okon K. Hobnail hemangioma: a immunohistochemical study and literature review. Pol J Pathol 2012;63:189-92. [Google Scholar] |
Fulltext Views
3,570
PDF downloads
2,465






