Translate this page into:
Venous malformation mimicking epidermoid cyst at the peri-ocular location in adults
Corresponding author: Dr. Kanika SahniAdditional ProfessorDepartment of Dermatology and VenereologyRoom 4070, Teaching Block, AIIMS, Delhi: 110029, India kanu.sah@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Mehta N, Dudani P, Agarwal S, Gupta S, Sahni K. Venous malformation mimicking epidermoid cyst at the peri-ocular location in adults. Indian J Dermatol Venereol Leprol 2022;88:399-401.
Sir,
We hereby report an observation seen in six patients over the last five years. They had skin-coloured peri-ocular swellings clinically suspected to be epidermoid cysts, which turned out to be cavernous haemangiomas on histopathological examination. Cavernous haemangiomas are venous malformations formed by a dermal or subcutaneous collection of dilated vascular channels, lined by flattened endothelial cells and thick fibrous septae.
All patients had a similar presentation— a single asymptomatic skin-coloured oval swelling at peri-ocular location [Figure 1a].The swellings were firm and slightly mobile but not adherent to the overlying skin. There was no history of any discharge or presence of a true punctum. A bluish-green hue with surface lobulation, but without any opening, was misinterpreted as a punctum in two cases. We termed this feature of cavernous haemangioma as a ‘pseudo-punctum’ [Figure 1b]. The swelling was located over the eyelid in three cases, temporal region in two and forehead in one case. All patients reported onset in adulthood, with gradual progression over years to the present size. Epidermoid cyst was the chief clinical diagnosis, although a differential of vascular malformation was considered in one case. During surgical excision, intra-operative bleeding exceeded the expected amount in two cases. Three excised lesions were brown-black, ill-defined and unencapsulated on gross examination [Figure 1c and d]. No post-operative hematoma was reported in any case.

- Venous malformations at peri-ocular area in adults mimicking epidermoid cysts. (a) Swelling in the upper eyelid just beneath the eyebrow in Patient 1, with a bluish-hue. (b) A nearly identical presentation in Patient 2, along with a ‘pseudo-punctum’. Grossly dark haemorrhagic lesion seen intra-operatively (c) and after excision (d) in Patient 3.
Histopathological examination revealed multiple large endothelial-cell-lined spaces congested with erythrocytes [Figure 2a]. Two cases showed muscle in the wall, implying a venous component, highlighted by Masson’s trichrome [Figure 2b].
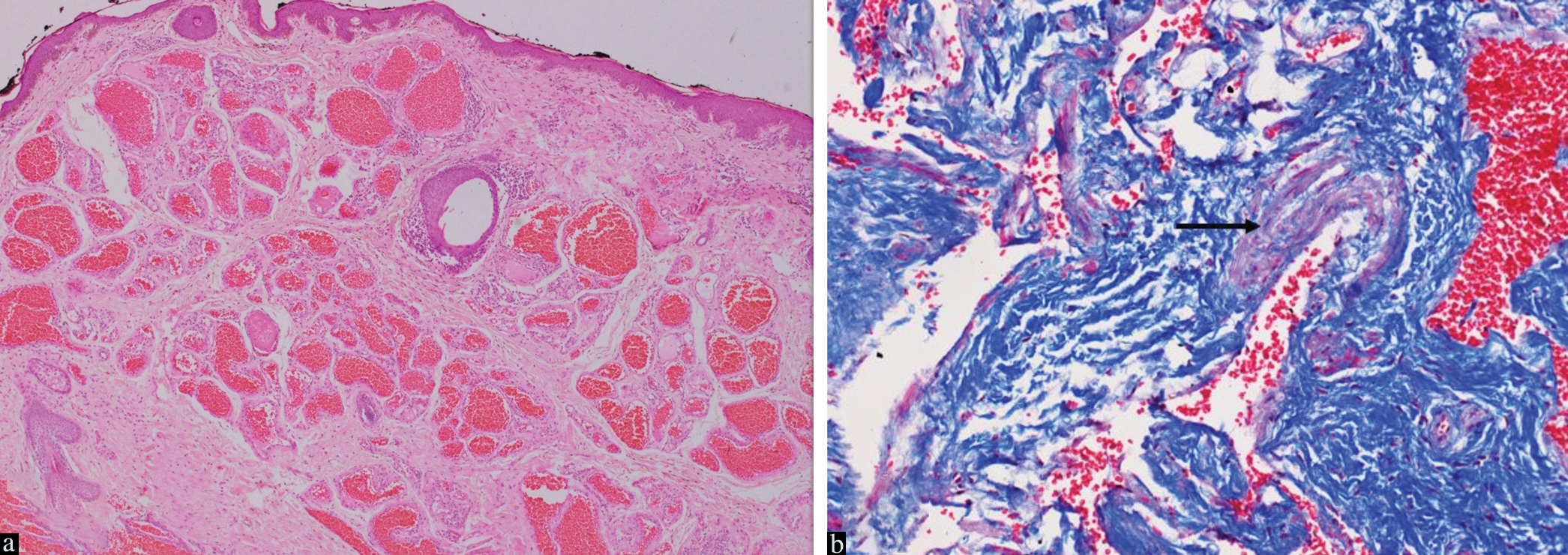
- Histopathology of cavernous haemangioma type of venous malformation. (a) Multiple large endothelial-cell lined spaces are congested with erythrocytes throughout the dermis. Haematoxylin and eosin, magnification × 400. (b) Myocytes in the wall, implying a venous component, in one of the specimens. Masson’s trichrome, magnification × 1000.
Epidermoid cysts are frequently seen over the head and neck. They present as single-to-few, asymptomatic slow-growing skin-coloured ovoid firm swellings within the skin. A punctum, when present, is pathognomonic, but is absent in many cases. Many different lesions may mimic an epidermoid cyst, including developmental cysts, benign cell proliferation such as nodular hidradenoma, as well as primary and secondary malignant lesions such as cutaneous B-cell lymphoma, epithelioid sarcoma, cutaneous meningioma, Merkel cell carcinoma, metastatic lung adenocarcinoma, to name a few.1 Vascular lesions have not yet been reported to mimic epidermoid cysts; however, the reverse has been seen; true epidermoid cysts may mimic lymphatic malformations.2
Cavernous haemangioma of cutaneous venous malformation, presents as a single, small skin-coloured to slightly bluish deep-seated swelling which may be elevated. About 50% of the cases are localised to the head and neck, although virtually any site may be affected. Contrary to conventional venous malformations which present as congenital large bluish-green soft compressible plaques, cavernous haemangiomas are late-presenting small skin-coloured to blue firm swellings.3 In skin of colour, a blue hue is often not appreciated.
The older term, cavernous haemangioma still dominates pathological and non-dermatological literature. ‘Haemangioma’ is not appropriate for these lesions, as they are not tumours but malformations. They are probably present at birth, but manifest late and do not regress spontaneously. They have been included under the umbrella term ‘slow-flow vascular malformation’ in the latest classification by the International Society for the Study of Vascular Anomalies.4
Radiological investigations are not helpful in their differentiation from epidermoid cysts. Both entities are predominantly hypoechoic on ultrasound, hyperintense on T1-weighted magnetic resonance imaging and poorly visualised by computed tomography. Doppler imaging is also not helpful as the flow is extremely slow.5 The calibre of these malformations is usually too small to allow phlebolith formation. The thick fibrous septae and endothelial growth within lesions may introduce hyperechoic areas, but such changes can also be seen in epidermoid cysts. Lastly, the small lesion size at presentation does not allow detailed ultrasonographic evaluation.
In conclusion, clinical clues to a cavernous malformation include peri-ocular location, lack of true punctum and the presence of a pseudo-punctum. This differential diagnosis of an epidermoid cyst enables the surgeon to suspect a vascular malformation during on-table gross evaluation and change their approach to pre-empt haemorrhagic losses and post-operative hematoma formation.
Declaration of Patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Epidermoid cyst mimicry: report of seven cases and review of the literature. J Clin Aesthet Dermatol. 2009;2:28-33.
- [PubMed] [Google Scholar]
- Low-flow vascular malformation pitfalls: From clinical examination to practical imaging evaluation–Part 1, lymphatic malformation mimickers. Am J Roentgenol. 2016;206:940-51.
- [CrossRef] [PubMed] [Google Scholar]
- Vascular malformations. In: Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, Wolff K, eds. Fitzpatrick’s Dermatology in General Medicine (8th ed). New York, NY: McGraw-Hill; 2012. p. :2076-93. In: eds
- [Google Scholar]
- ISSVA Classification of Vascular Anomalies ©2018 International Society for the Study of Vascular Anomalies Available at “issva.org/classification” Accessed March 2021.
- Low-flow vascular malformation pitfalls: From clinical examination to practical imaging evaluation-Part 2, lymphatic malformation mimickers. Am J Roentgenol. 2016;206:952-62.
- [CrossRef] [PubMed] [Google Scholar]





