Translate this page into:
Vitiligo developing in congenital segmental speckled lentiginous nevus: Another example of immunocompromised cutaneous district due to immunological assault on aberrant melanocytes?
2 Department of Dermatology, Katihar Medical College and Hospital, Katihar, Bihar, India
Correspondence Address:
Anup Kumar Tiwary
House No. 12, Diamond Building, Government Medical College, Haldwani, Uttarakhand
India
| How to cite this article: Tiwary AK, Kumar P. Vitiligo developing in congenital segmental speckled lentiginous nevus: Another example of immunocompromised cutaneous district due to immunological assault on aberrant melanocytes?. Indian J Dermatol Venereol Leprol 2017;83:612-614 |
Sir,
Speckled lentiginous nevus (SLN) is a relatively uncommon melanocytic nevus clinically characterized by the presence of dark colored macules and/or papules scattered over the pale brown base.[1] Vitiligo has also been reported with this nevus but in “halo” configuration in the surrounding normal skin.[2] Here, we report a unique case of co-localization of trichrome vitiligo “within” the congenital segmental speckled lentiginous nevus on face in a 9-year-old girl.
A 9-year-old girl came to the outpatient department of dermatology in a government medical college and hospital, Haldwani. She presented with a well demarcated, evenly pigmented brownish patch (base) superimposed with multiple scattered, dark brown colored macules on left cheek and periocular area since her infancy. She had also two depigmented patches within the brownish base since 2 years. Parents revealed that pale brown larger patch was present at birth but smaller dark colored scattered macules started developing since the age of 2 years and ceased to grow in number by the age of 7 years. There was no history of any pre-existing dermatosis. Personal and family history of any autoimmune disorders was non-contributory.
Cutaneous examination showed a well defined, pale brown or tan patch of size 8 cm × 12 cm, speckled with numerous small darkly pigmented macules of size 1 mm–3 mm. One vitiligo patch affected the skin of inner canthus, medial side of upper eyelid and infra-orbital region, showing ill-defined borders and some hypopigmented area in contact with normal skin suggestive of the three colors of trichrome vitiligo [Figure - 1]. The other depigmented patch was present over left cheek. Rest of the mucocutaneous and systemic examination was unremarkable and routine investigations were within normal limits.
 |
| Figure 1: Large, pale brown patch speckled with numerous, small darkly pigmented macules on left side of face |
Histopathological examination (HPE) of punch biopsy specimen taken from small dark speckled macular component of nevus and depigmented patch was done. Dark coloured speckled small macule revealed melanocytic hyperplasia in basal layer, dermal aggregation of naevomelanocytic cells along with junctional activity, while depigmented patch demonstrated complete absence of melanocytes in the basal layer of the epidermis and no nevomelanocytic cells in dermis [Figure - 2] and [Figure - 3]. Common to these two lesions were the presence of mononuclear inflammatory infiltrates in the papillary dermis suggesting some immunological basis of these lesions. Due to the poor infrastructure and financial constraints of the patient, staining for melanocytes and immunohistochemistry for infiltrating dermal mononuclear cells could not be done.
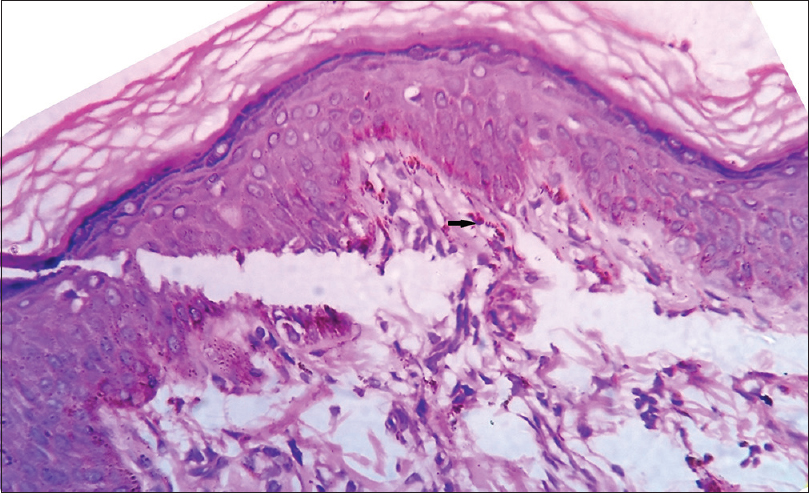 |
| Figure 2: Small, dark coloured scattered macule revealing melanocytic hyperplasia in basal layer and dermal aggregation of naevomelanocytic cells along with junctional activity (black arrow) (H and E, ×400) |
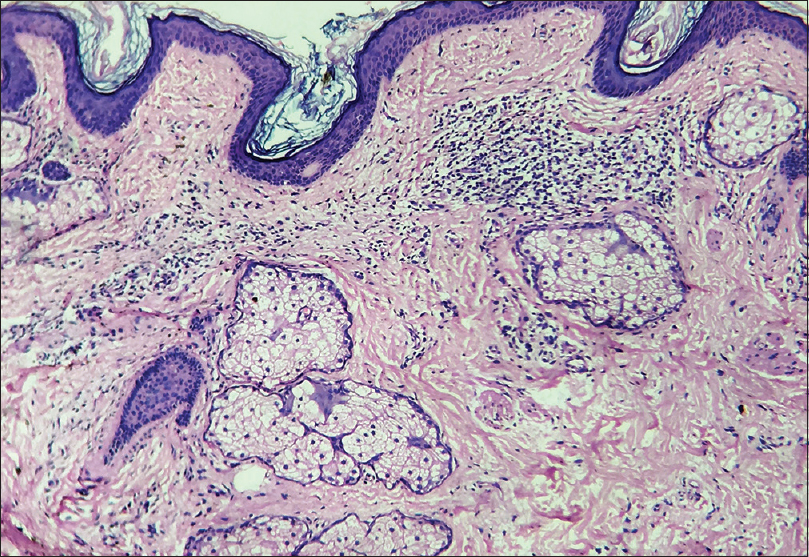 |
| Figure 3: Depigmented patch of vitiligo with complete absence of melanocytes in the basal layer of the epidermis and lymphocytic collections in papillary dermis (H and E, ×100) |
Based on typical history of evolution, characteristic clinical appearance and the histopathological findings, it was concluded as a case of “Congenital segmental speckled lentiginous nevus,” which was co-localized with trichrome vitiligo.
Because of the very young age of patient, no aggressive treatment was offered except topical application of tacrolimus and basic fibroblast growth factor solution (bFGF) for vitiligo but patient did not turn up further.
It is usually noticed during infancy or childhood with the development of tan or brown patch as base on which multiple dark flat or elevated lesions arise over the time due to nevomelanocytic aggregations at dermoepidermal junction or dermis and tends to persist for life although its spontaneous regression is possible.[3],[4],[5]
There is an interesting and complex association between melanocytic nevus (congenital or acquired) and vitiligo as evidenced by occasional development of vitiligo lesions around melanocytic nevus. The relative configuration and chronological sequence of development of the melanocytic nevus and vitiligo may vary. The depigmented patch usually follows the pre-existing nevus and encircle it like “halo,” classically seen in halo nevi. Speckled lentiginous nevus is no exception as it was seen to be encircled by vitiligo lesions in one such case reported previously in literature.[2] Of note, we were unable to find any previous reports describing the development of vitiligo “within” the speckled lentiginous nevus as in our case.
The co-occurrence of melanocytic nevus and vitiligo is fascinating to dermatologists. It has been proposed that both melanocytic nevi and vitiligo occur due to mosaicism of abnormal melanocytes leading to the stimulation of cellular immunity. In vitiligo, melanocytorrhagic apoptosis of abnormal melanocytes ultimately leads to depigmentation while in cases of melanocytic nevi, immune reactions against nevomelanocytes may face both outcome; regression of nevi or development of depigmented patche/s, “within” or “around” the nevus due to immunological clearance of normal or abnormal melanocytes, respectively.[6]
In recent few years, a new concept has been put forward to explain many isotopic development of dermatoses as “locus minoris resistentiae” which was collectively termed as “Immunocompromised cutaneous district (ICD).” According to the current concept of ICD, a complex and altered interplay between immune cells, nerve fibres and neuromediators occurs within the primary lesion, resulting in localized immune dysregulation which may lead to the development of secondary lesion manifesting as opportunistic infections, tumors, or immune reactions/disorders.[7]
Development of secondary lesion in the form of depigmented patch of vitiligo (immune reaction) over the speckled lentiginous nevus (primary lesion) justifies it as a new example of ICD.
Histopathology of such melanocytic nevus, in addition to basal melanocytic hyperplasia and nevomelanocytic aggregations in papillary dermis, shows the presence of superficial dermal lymphocytic infiltrates in both the biopsy specimen, depigmented patch of vitiligo and melanocytic nevus further supporting the role of immunological reactivity against shared melanocytic antigens.
With all such clinicopathological descriptions of this fascinating association and based on newer concept of ICD, our case also justifies to be considered as another ICD caused by immunological assault on aberrant melanocytes of mosaic origin.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the legal guardian has given his consent for images and other clinical information to be reported in the journal. The guardian understands that name and initial will not be published and due efforts will be made to conceal patient identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Thappa DM, Garg BR, Bansal D, Ratnakar C. Speckled lentiginous naevus. Indian J Dermatol Venereol Leprol 1995;61:224-5.
[Google Scholar]
|
| 2. |
Kim YY, Kim MY, Kim TY. Development of halo nevus around nevus spilus as a central nevus, and the concurrent vitiligo. Ann Dermatol 2008;20:237-9.
[Google Scholar]
|
| 3. |
Corradin MT, Cacitti V, Giulioni E, Patriarca MM, Vettorello A. Nevus spilus: A review of the literature. SM J Dermatol 2015;1:1003.
[Google Scholar]
|
| 4. |
Kalla G, Purohit S, Purohit A, Vyas M. Speckled lentiginous naevus. Indian J Dermatol Venereol Leprol 1996;62:329-30.
[Google Scholar]
|
| 5. |
Cecchi R, Fancelli L, Troiano M. Melanoma arising in giant zosteriform nevus spilus. Indian J Dermatol Venereol Leprol 2012;78:643-5.
[Google Scholar]
|
| 6. |
Attili VR, Attili SK. Anatomical segmentations in all forms of vitiligo: A new dimension to the etiopathogenesis. Indian J Dermatol Venereol Leprol 2016;82:379-88.
[Google Scholar]
|
| 7. |
Caccavale S, Kannangara AP, Ruocco E. The immunocompromised cutaneous district and the necessity of a new classification of its disparate causes. Indian J Dermatol Venereol Leprol 2016;82:227-9.
[Google Scholar]
|
Fulltext Views
3,962
PDF downloads
1,166





