Translate this page into:
Warfarin-induced calciphylaxis in a chronic hypercalcemic patient
2 Department of Dermatology, Taipei Medical University Hospital, Taipei, Taiwan
3 Department of Internal Medicine, Division of Nephrology, Wan Fang Hospital, Taipei Medical University, Taipei, Taiwan
Correspondence Address:
Chun-Hong Hu
Department of Dermatology, Wan Fang Hospital, No. 111, Sec. 3, Xinglong Rd., Wenshan Dist., Taipei City 116
Taiwan
| How to cite this article: Huang YC, Chou CY, Sue YM, Hu CH. Warfarin-induced calciphylaxis in a chronic hypercalcemic patient. Indian J Dermatol Venereol Leprol 2013;79:135 |
Sir,
Calciphylaxis most commonly occurs in patients with end-stage renal disease under dialysis. Warfarin is a risk factor for calciphylaxis in uremic patients, but is rarely known to induce calciphylaxis in non-uremic patients. We report herein a warfarin-induced calciphylaxis in a patient with chronic hypercalcemia.
A 19-year-old male patient with history of persistent hypercalcemia of unknown cause and chronic renal insufficiency for 1 year presented himself with extensive painful necrotic ulcer over bilateral legs for 4 months [Figure - 1]. Review of history showed that he received bilateral iliac vein stenting for the iliac vein compression syndrome. He then received warfarin after the stent implantation. One month after warfarin treatment, he developed progressive painful ulceration on bilateral legs within 1 week. The results of laboratory examination indicated elevated serum creatinine (2.1 mg/dL), calcium (12.9 mg/dL), normal phosphate (4 mg/dL) and decreased intact parathyroid hormone (6.32 ng/L). The findings of urine analysis were mild proteinuria and hematuria. Renal sonography was found to have bilateral renal stones and right hydronephrosis. The titre values of antinuclear antibody, rheumatoid factor, antineutrophil cytoplasmic antibody, antiphospholipid antibody and cryoglobulin were all negative. The result of immunoelectrophoresis showed no monoclonal gammopathy. As shown in [Figure - 2], the specimen picture of skin biopsy presented subcutaneous calcium deposits with diffuse panniculitis and fat necrosis. [Figure - 3] shows calcification within the media of small- and medium-sized arterioles, with extensive intimal hyperplasia and fibrosis. We suspected a warfarin-induced calciphylaxis and shifted it to aspirin. The ulcerations were managed by local wound care, and gradually healed with residual scars within 5 months. At that time, all our survey for hypercalcemia only revealed a high 1,25 (OH) vitamin D3 (67 pg/mL), and no etiology of hypervitaminosis D could be identified. Patient′s hypercalcemia was persistent and we educated him not to take warfarin anymore.
 |
| Figure 1: Widespread necrotic ulcerations over the right leg |
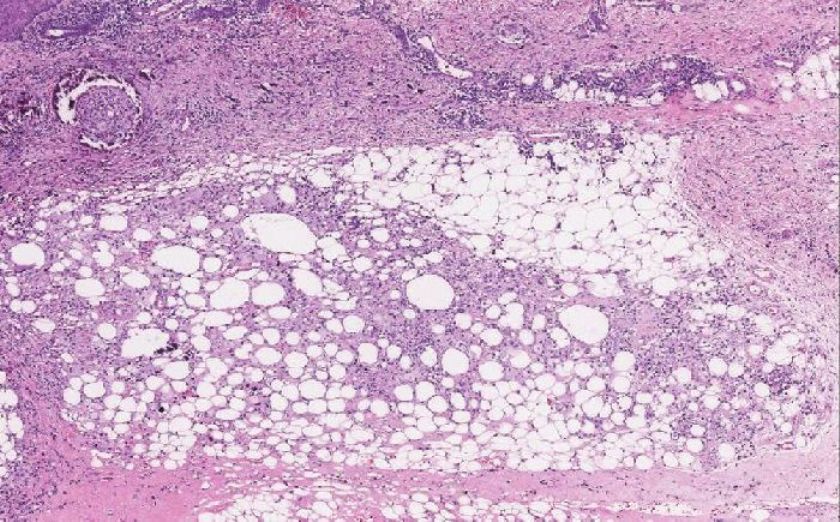 |
| Figure 2: Calcification within the arterioles and subcutaneous calcium deposits with panniculitis and fat necrosis (H and E, x100) |
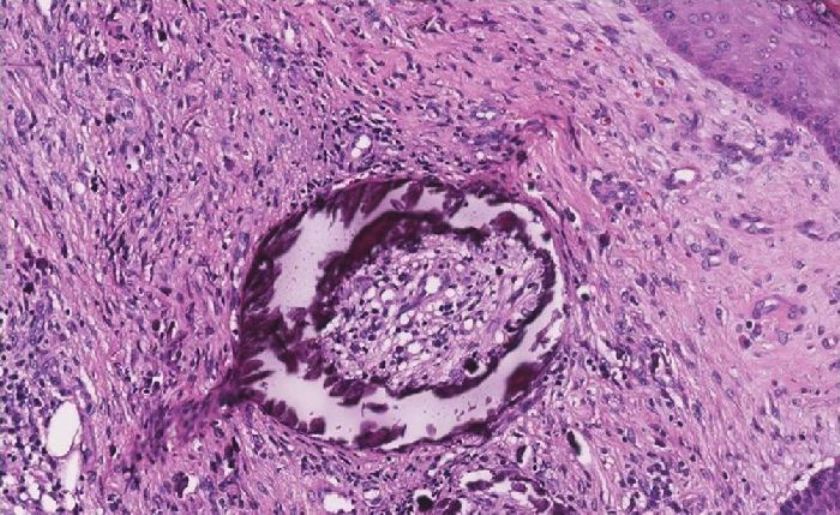 |
| Figure 3: Circumferential medial calcific deposit in an arteriole with extensive intimal hyperplasia and fibrosis (H and E, x400) |
Except calciphylaxis, we need to consider the conditions of antiphospholipid syndrome or vasculitis in a patient with extensive necrotic ulcerations. We could exclude those diseases by adequate laboratory workup and the typical histological findings of calciphylaxis.
In non-uremic patients, primary hyperparathyroidism, malignancy and connective tissue diseases are the most commonly found underlying diseases. [1] Other possible causes in calciphylaxis include high calcium phosphate product and hypercoaguability. But, only few reports exist in the literature to describe warfarin-induced calciphylaxis in non-uremic patients. [2],[3] Warfarin can inhibit the activation of matrix G1A protein, which inhibits vascular calcification and reduces functional protein C levels to cause hypercoaguability. [4] Our patient had persistent hypercalcemia and was triggered by warfarin therapy. Combination of hypercalcemia and warfarin therapy can lead to calciphylaxis. To the best of our knowledge, this is the first report of warfarin-induced calciphylaxis in a non-uremic hypercalcemic patient.
Calciphylaxis is a condition with high morbidity and mortality usually due to infection. Intravenous sodium thiosulfate is a novel treatment for calciphylaxis through the probable mechanism of dissolving insoluble calcium salts in tissue into soluble calcium thiosulfate. [5] The current therapeutic trend for calciphylaxis consists of reducing calcium phosphate product, improving hypercoaguability, improving wound care, prevention of infection and using a trial of intravenous sodium thiosulfate. Avoiding warfarin in a high-risk patient and halting it in a patient with existing calciphylaxis are important.
| 1. |
Nigwekar SU, Wolf M, Sterns RH, Hix JK. Calciphylaxis from nonuremic causes: A systematic review. Clin J Am Soc Nephrol 2008;3:1139-43.
[Google Scholar]
|
| 2. |
Asobie N, Wong E, Cook MG. Calciphylaxis in a diabetic patient provoked by warfarin therapy. Clin Exp Dermatol 2008;33:342-4.
[Google Scholar]
|
| 3. |
Banerjee C, Woller SC, Holm JR, Stevens SM, Lahey MJ. Atypical calciphylaxis in a patient receiving warfarin then resolving with cessation of warfarin and application of hyperbaric oxygen therapy. Clin Appl Thromb Hemost 2010;16:345-50.
[Google Scholar]
|
| 4. |
Howe AM, Webster WS. Warfarin exposure and calcification of the arterial system in the rat. Int J Exp Pathol 2000;81:51-6.
[Google Scholar]
|
| 5. |
Schlieper G, Brandenburg V, Ketteler M, Floege J. Sodium thiosulfate in the treatment of calcific uremic arteriolopathy. Nat Rev Nephrol 2009;5:539-43.
[Google Scholar]
|
Fulltext Views
3,411
PDF downloads
1,969





