Translate this page into:
Wickham's striae-like appearance in a case of nodular Kaposi's sarcoma: A dermoscopic pitfall
2 Department of Pathology, Jawaharlal Institute of Postgraduate Medical Education and Research, Puducherry, India
Correspondence Address:
Laxmisha Chandrashekar
Department of Dermatology, Venereology and Leprology, Jawaharlal Institute of Postgraduate Medical Education and Research, Puducherry - 605 006
India
| How to cite this article: Behera B, Remya R, Chandrashekar L, Thappa DM, Gochhait D, Dey B. Wickham's striae-like appearance in a case of nodular Kaposi's sarcoma: A dermoscopic pitfall. Indian J Dermatol Venereol Leprol 2017;83:604-606 |
Sir,
A 45-year-old human immunodeficiency virus-seropositive man presented with 6-month history of progressively enlarging solitary asymptomatic swelling over the left leg. Cutaneous examination revealed a solitary firm, nontender, violaceous nodule of size 5 mm × 5 mm over the medial aspect of left leg with mild surface scaling [Figure - 1]. A differential diagnosis of lichen planus, Kaposi's sarcoma, basal cell carcinoma and malignant melanoma was considered. On nonpolarized contact dermoscopy, the nodule displayed a central prominent Wickham's stria-like appearance (red arrow), bluish-red areas (blue arrows), blue-white veil-like structure (yellow arrows) and multiple brown globules [black arrows, [Figure - 2]. The central Wickham's striae-like area was “out of focus” [Figure - 3]. His CD4 count was 432/mm [3] and serological tests for hepatitis B antigen, anti-hepatitis C virus antibodies and venereal disease research laboratory tests were negative. The histopathology of the excised nodule revealed hyperkeratosis, hypergranulosis, irregular acanthosis and proliferation of spindle-shaped endothelial cells forming slit-like vascular spaces in the upper and middle dermis admixed with variable lymphoplasmacytic infiltrate, and hemorrhage [Figure - 4]a. Promontory sign characterized by protrusion of new vessels into existing large vessel was also demonstrated [Figure - 4]b. Both hemosiderin-laden macrophages and free hemosiderin deposition was evident in the dermis [Figure 4c]. On immunohistochemistry, the spindle cells were positive for CD-31 [Figure 4d] and CD34. Based on clinical, histopathology and immunohistochemistry, a final diagnosis of Kaposi's sarcoma was made.
 |
| Figure 1: Solitary 5 mm × 5 mm violaceous nodule over the left leg with surface scaling |
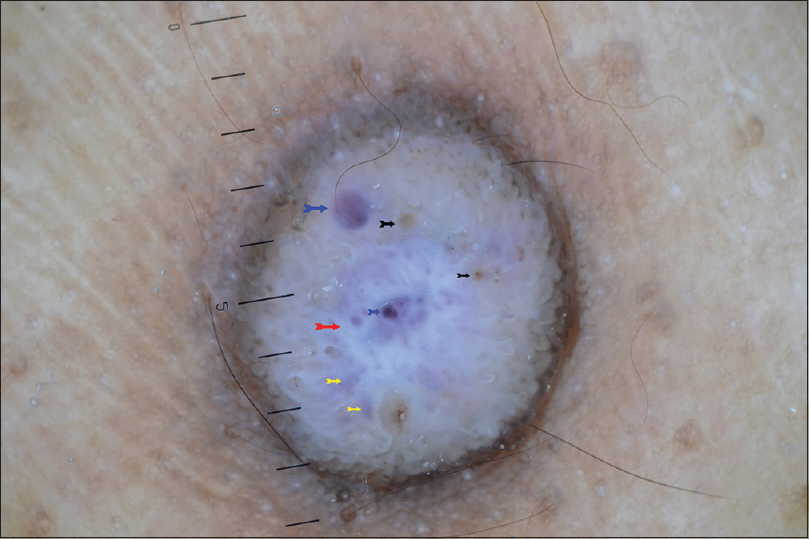 |
| Figure 2: Nonpolarized contact dermoscopy of the nodule showing “multicolored pattern” consisting of a central Wickham's stria-like appearance/pearly white area (red arrow), bluish-reddish areas (blue arrows), blue-white veil-like structure (yellow arrows) and multiple brown globules (black arrows) |
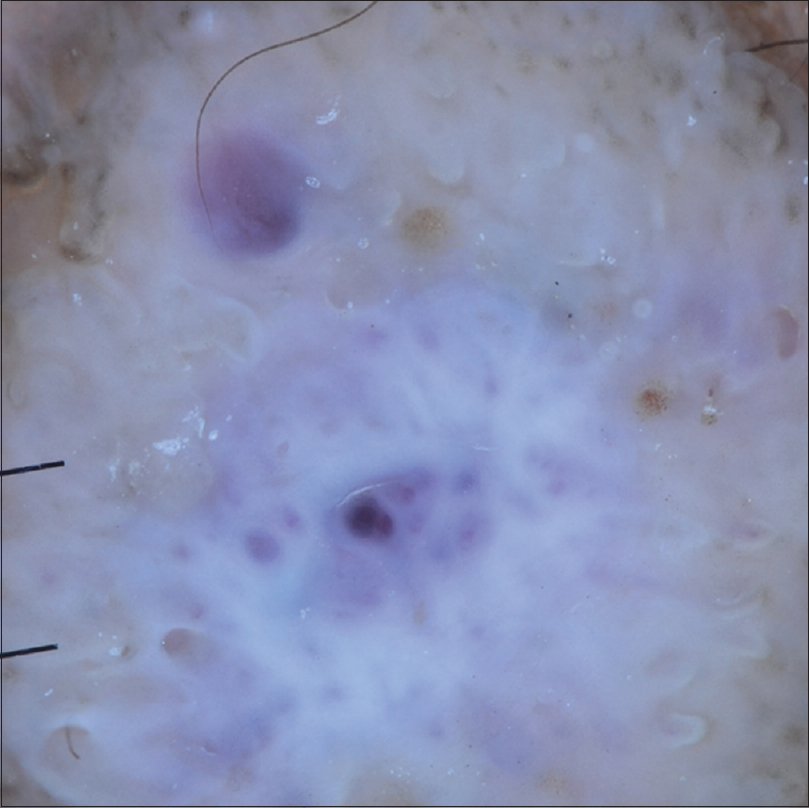 |
| Figure 3: Nonpolarized contact dermoscopy of the nodule under magnification demonstrating “out-of-focus Wickham's striae-like appearance” and in-focus bluish-red area and brown globules. |
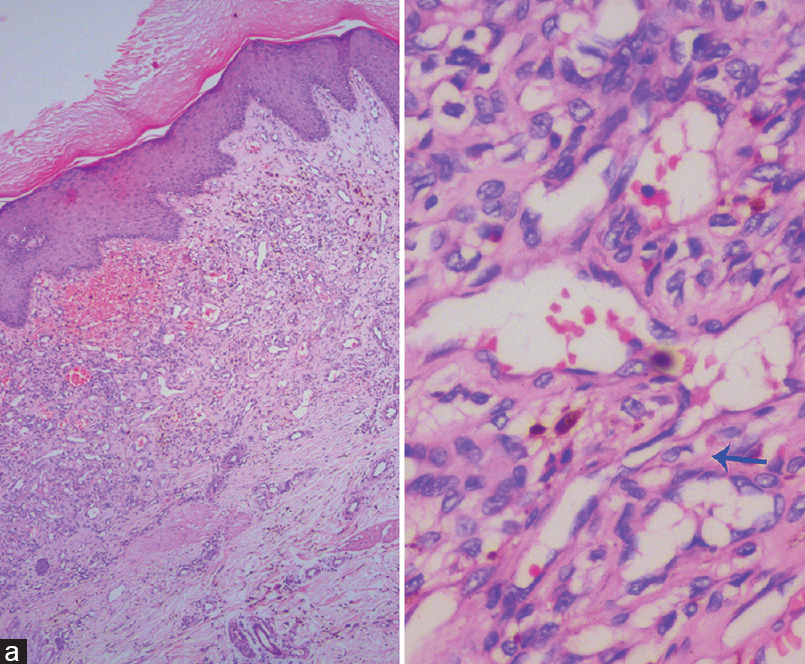 |
| Figure 4a and b: (a) Histology showing hyperkeratosis, hypergranulosis, irregular acanthosis and proliferation of spindle-shaped endothelial cells forming slit-like vascular spaces in upper and middle dermis admixed with variable lympho-plasmacytic infiltrate, and hemorrhage (H and E, ×100). (b) Promontory sign; protrusion of new vessels into existing large vessel (H and E, ×400). |
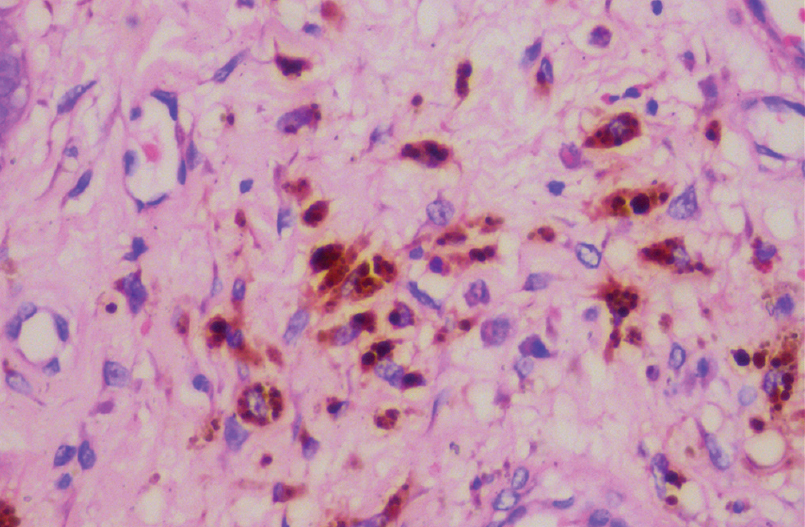 |
| Figure 4c: Free hemosiderin and hemosiderin-laden macrophages that correspond to the brown dots and globules under dermoscope (H and E, ×400) |
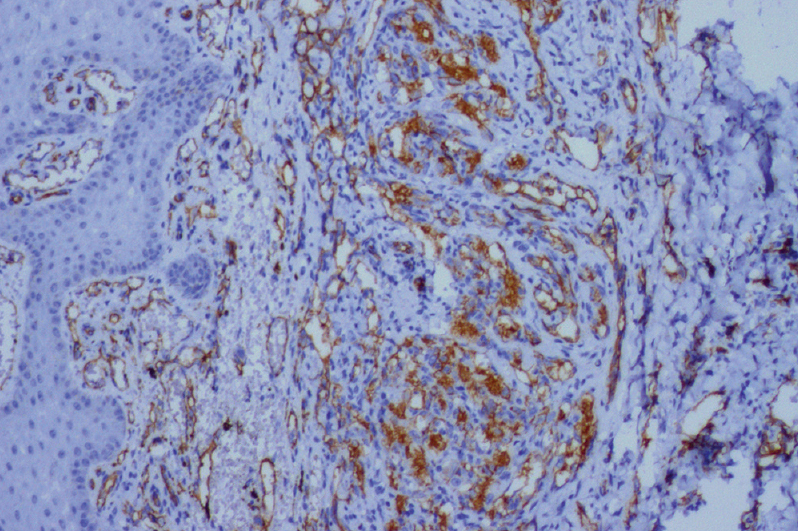 |
| Figure 4d: Immunohistochemistry showing CD31-positive spindle-shaped endothelial cells (IHC, ×400) |
Kaposi's sarcoma in human immunodeficiency virus-seropositive individuals can be misdiagnosed as lichen planus, malignant melanoma, pseudo-Kaposi sarcoma and bacillary angiomatosis. The problem is further amplified by the low incidence of Kaposi's sarcoma in Indian population. The various dermoscopic features of Kaposi's sarcoma described by Cheng et al. under polarized dermoscopy are bluish-red coloration (83%), a scaly surface (29%), small brown globules (14%) and most importantly, the multicolored rainbow pattern (36%).[1] They claimed that, although less sensitive (36.2%), the presence of the multicolored rainbow pattern is the specific (100%) dermoscopic feature of Kaposi's sarcoma as they did not find the same in 54 non-Kaposi sarcoma cutaneous tumors. They did not observe the rainbow pattern in Kaposi's sarcoma lesions when examined under nonpolarized immersion dermoscopy which they explained due to the better interaction of the polarized light beam with the dermal located vascular tumor.[1] They proposed that the rainbow pattern is due to the diffraction of light from the closely set, “back-to-back” dermal vessels present within the tumor with minimal intervening stromal and cellular tissue.[1] The absence of rainbow pattern in the rest of Kaposi's sarcoma lesions and other vascular and nonvascular cutaneous tumors was due to the lumen poor pattern of growth with abundant amounts of intervening stromal and cellular tissues.[1] The other dermatological conditions reported to produce multicolored rainbow pattern under polarized dermoscope are lichen planus, malignant melanoma, stasis dermatitis, hemosiderotic dermatofibroma and atypical fibroxanthoma.[2],[3] In our case, the nodular Kaposi's sarcoma under nonpolarized contact dermoscopy (HEINE DELTA20® Dermatoscope, ×10 magnification) did not demonstrate rainbow pattern but showed different colors consisting of pearly white area, bluish-red areas and blue-white veil-like structure. We called it “multicolored pattern” but not rainbow pattern which is probably a feature of polarized dermoscopy. The presence of Wickham's striae or pearly white area is considered to be a valuable dermoscopic finding of lichen planus. The various morphological patterns of Wickham's striae are reticular, circular, linear, globular, radial streaming, veil-like and combined.[4] In our case, despite the presence of Wickham's striae-like appearance, the presence of multicolor pattern gave a clue to the underlying vascular nature of the nodule, thus ruling out lichen planus. A multicolored structureless pattern has been described in a case of extradigital golmus tumor under polarized, non-contact dermoscopy that showed a central purple color surrounded by a whitish area and a peripheral brown pigmentation.[5] The Wickham's striae-like appearane in the present case were “out of focus,” which can help to differentiate Kaposi's sarcoma from lichen planus. Coates and Bowling reported nonspecific reddish-brown erythema under nonpolarized contact dermoscopy in two cases of Kaposi's sarcoma.[6] The prominent white/pearly white area correspond to compact orthokeratosis above the hypergranulosis. In our case, the out-of-focus Wickham's striae may be due to the presence of prominent hyperkeratosis above the zone of hypergranulosis. The bluish-red area and blue-white veil-like structure correspond to the proliferating dermal blood vessels, the scaling to the eczematous change over the surface and brown globules to the hemosiderin-laden macrophages. The prominent white/pearly white area and less prominent red area in our case may be due to the fact that superficial structures (hyperkeratosis, hypergranulosis and acanthosis) are better visualized by nonpolarized dermoscopy than deeper structures (vessels) and the skin color of the patient (skin type V).[7] The presence of blue-white veil-like structure has been described in malignant melanoma. The presence of multicolor pattern and absence of pigment network in our case helped in differentiating Kaposi's sarcoma from malignant melanoma. Blue-white veil-like structures and brown dots have been described in basal cell carcinoma, especially pigmented basal cell carcinoma.[8],[9] The presence of multicolor pattern/pearly white area can help in differentiating Kaposi's sarcoma from basal cell carcinoma. Use of dermoscopy is evolving day by day as a diagnostic tool in various cutaneous disorders. It can be sometimes misleading unless interpreted properly. The dermoscopic features of vascular tumors can be overshadowed by the epidermal structures (Wickham's striae-like appearance as in our case). Hence, it is very important to look for any subtle feature (bluish-red area as in our case) that can point toward the vascular nature of the lesion. Another important clue toward the vascular nature of the lesion is the presence of brown dots/globules (free hemosiderin and hemosiderin laden macrophages). The pigment pattern due to hemosiderin deposition is reflected as brown dots and globules in a focal or irregular pattern probably due to its golden-brown colour. In contrast, the pigment pattern due to melanin deposition can reflect as brown, black, gray to blue colour in a network, pseudonetwork or irregular pattern. Hence, it is very crucial to analyze each dermoscopic finding of the cutaneous lesion and correlate it with histopathological features.
In conclusion, the presence of out of focus Wickham's striae-like appearance under nonpolarized contact dermoscopy in a case of nodular Kaposi's sarcoma can be a dermoscopic pitfall. The presence of multicolored pattern can help in differentiating it from other clinical mimics.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Cheng ST, Ke CL, Lee CH, Wu CS, Chen GS, Hu SC. Rainbow pattern in Kaposi's sarcoma under polarized dermoscopy: A dermoscopic pathological study. Br J Dermatol 2009;160:801-9.
[Google Scholar]
|
| 2. |
Vázquez-López F, García-García B, Rajadhyaksha M, Marghoob AA. Dermoscopic rainbow pattern in non-Kaposi sarcoma lesions. Br J Dermatol 2009;161:474-5.
[Google Scholar]
|
| 3. |
Pitarch G. Dermoscopic rainbow pattern in atypical fibroxanthoma. Actas Dermosifiliogr 2014;105:97-9.
[Google Scholar]
|
| 4. |
Güngör S, Topal IO, Göncü EK. Dermoscopic patterns in active and regressive lichen planus and lichen planus variants: A morphological study. Dermatol Pract Concept 2015;5:45-53.
[Google Scholar]
|
| 5. |
Oliveira A. Dermoscopy in the diagnosis of extradigital glomus tumors. Int J Dermatol 2016;55: e504–e518.
[Google Scholar]
|
| 6. |
Coates D, Bowling J. Dermoscopy is not always helpful in the diagnosis of vascular lesions. Australas J Dermatol 2010;51:292-4.
[Google Scholar]
|
| 7. |
Benvenuto-Andrade C, Dusza SW, Agero AL, Scope A, Rajadhyaksha M, Halpern AC, et al. Differences between polarized light dermoscopy and immersion contact dermoscopy for the evaluation of skin lesions. Arch Dermatol 2007;143:329-38.
[Google Scholar]
|
| 8. |
Menzies SW, Westerhoff K, Rabinovitz H, Kopf AW, McCarthy WH, Katz B. Surface microscopy of pigmented basal cell carcinoma. Arch Dermatol 2000;136:1012-6.
[Google Scholar]
|
| 9. |
Altamura D, Menzies SW, Argenziano G, Zalaudek I, Soyer HP, Sera F, et al. Dermatoscopy of basal cell carcinoma: Morphologic variability of global and local features and accuracy of diagnosis. J Am Acad Dermatol 2010;62:67-75.
[Google Scholar]
|
Fulltext Views
5,900
PDF downloads
1,289





