Translate this page into:
A case of Parry-Romberg syndrome with congenital heart disease
2 Department of Surgery, Dr. D. Y. Patil Medical College and Hospital, Pimpri, Pune, Maharashtra, India
Correspondence Address:
Supriya P Deshmukh
401- Gaurangi CHS, Opposite Damani Estate Post Office, L.B.S. Marg, Thane - 400 601, Maharashtra
India
| How to cite this article: Deshmukh SP, Sharma YK, Dogra BB, Chaudhari NC. A case of Parry-Romberg syndrome with congenital heart disease. Indian J Dermatol Venereol Leprol 2012;78:105-106 |
Sir,
A 19-year-old female presented to our outpatient department with an asymptomatic, right-sided facial atrophy and alopecia involving frontal region of scalp and right eyebrow since four years [Figure - 1]. Skin over the involved areas was smooth in texture, non-dyspigmented, and could be easily pinched up on palpation. In addition to this, right eye showed retraction of upper-lid margin with loss of cilia and same-sided ear pinna showed atrophy of the skin and cartilage [Figure - 2]. She had a history of being operated for a congenital heart disease, i.e., Shone′s complex (subaortic stenosis and coarctation of aorta and additional finding of patent ductus arteriosus, as evidenced by the transthoracic echocardiographic report of 2006) diagnosed almost 6 years back [Figure - 3]a and b. Chest examination revealed sternotomy scar and cardiovascular system examination was normal. Dental examination was normal.
 |
| Figure 1: Right-sided facial atrophy and alopecia involving frontal area of scalp and eyebrow. This image also shows atrophied ear pinna |
 |
| Figure 2: Right eye upper lid margin is retracted with partial loss of cilia |
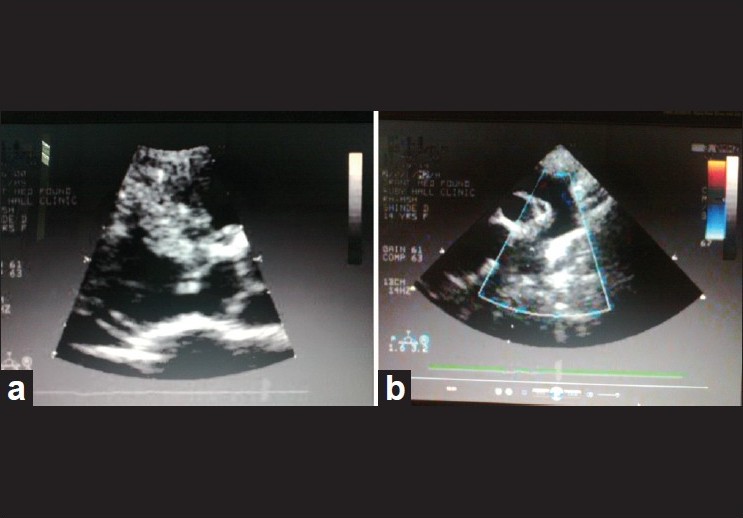 |
| Figure 3: Transthoracic echocardiography image showing Shone's complex, (a) Subaortic membrane (b) Coarctation of aorta |
Complete hemogram, urine analysis, antinuclear antibody were within normal limits. X-ray chest showed bilateral cervical ribs, right rib being more prominent than left and old sternal sutures. Orthopantogram X-ray, X-ray of skull, CT scan of brain, Electroencephalogram, Electrocardiogram, and Transthoracic echocardiography were normal. A punch biopsy from scalp was taken and a light microscopic evaluation of the hematoxylin and eosin (H and E)-stained histopathological slide showed atrophied epidermis, thick collagen bundles surrounding eccrine glands, and mild mononuclear cell infiltrate in reticular dermis. There was considerable loss of hair follicles and atrophy of appendages. Our clinical and histopathological findings made us keep both Parry-Romberg syndrome and linear localized scleroderma (LSc) "en coup de sabre" as the dermatological differential diagnoses, since both these conditions tend to overlap.
Parry-Romberg Syndrome is a rare disorder characterized by progressive hemifacial atrophy of the skin, adipose tissue, and in some cases involving muscle, cartilage, and underlying bony structures. The incidence and cause of this alteration is unknown. [1] Hyperactivity of the brain stem sympathetic centers, possibly caused by an autoimmune process, may be the primary cause for cutaneous and subcutaneous atrophy in this condition. [2] Trauma, viral infections, endocrine disturbances, and heredity are also believed to be associated with the disease. [1] It begins in childhood, preferentially involves the upper face, and is usually unilateral. It may start with hyper- or hypopigmentation, followed by slowly progressing atrophy which tends to remain limited to the distribution of the trigeminal nerve or may involve the entire face unilaterally or bilaterally. [3] A number of conditions have been reported in association with Parry-Romberg syndrome, [3] e.g., (1) Ocular changes such as loss of eyebrows and eyelashes, iris atrophy, ocular muscle palsies, uveitis, and enophthalmos; (2) Central nervous system disorders like migraine, headaches, hemiparesis, trigeminal neuralgia, and unilateral epilepsy. There may be localized areas of alopecia as seen in our case. The affected side of oral cavity can present with some deficiency in dental root development detectable on X-ray Orthopantogram and also unilateral atrophy of tongue. [3]
Linear LSc "en coup de sabre" is an autoimmune connective tissue disorder which involves the face unilaterally, usually the frontoparietal area, but may extend downward. Most cases begin before 10 years of age. The involved skin is depressed, hard, hyperpigmented, shiny, and devoid of hair. Ocular, neurological, and oral cavity alterations described above may be present with linear LSc "en coup de sabre" as well. [4]
The relationship between Parry-Romberg syndrome and linear LSc "en coup de sabre" is not clearly understood. Tollefson and Witman, [5] found in their study that both entities frequently co-exist and both are likely variants of morphea. However, Orozco-Covarrubias et al. [4] pointed out that in most cases, it is possible to differentiate between scleroderma "en coup de sabre" and Parry-Romberg syndrome. They found that most important clinical feature that differentiated both conditions was "cutaneous sclerosis," absence of which favors diagnosis of Parry-Romberg syndrome. Statistically significant histopathological features were connective tissue fibrosis, adnexal atrophy, and mononuclear cell infiltrate (superficial and deep), which favors a diagnosis of LSc "en coup de sabre."
Shone′s complex is a rare congenital heart disease, described by Shone et al. in 1963. The complete form typically consists of four obstructive lesions namely parachute-like mitral valve, supravalvar mitral ring, subaortic stenosis, and coarctation of aorta. [6] However, incomplete forms with two or three lesions are also described as seen in our case.
Sharma et al. [7] reported coexistence of LSc "en coup de sabre morphea" and aortic regurgitation in a single case of systemic sclerosis. However, association of Parry-Romberg syndrome or LSc "en coup de sabre morphea" with congenital heart disease has not been reported in the literature, and whether it is merely a chance occurrence or an actual association remains to be seen.
| 1. |
Da Silva Pinheiro TP, Camarinha-da Silva C, Limeira-da Silveira CS, Ereno-Botelho PC, Rodrigues Pinheiro MG, Viana-Pinheiro JJ. Progressive hemifacial atrophy-Case report. Med Oral Patol Oral Cir Bucal 2006;11:E112-4.
[Google Scholar]
|
| 2. |
Lonchampt P, Emile J, Pélier-Cady MC, Cadou B, Barthelaix A. Central sympathetic dysregulation and immunological abnormalities in a case of progressive facial hemiatrophy (Parry-Romberg disease). Clin Auton Res 1995;5:199-204.
[Google Scholar]
|
| 3. |
Sandhu K, Handa S. Subdural hygroma in a patient with Parry-Romberg Syndrome. Pediatr Dermatol 2004;21:48-50.
[Google Scholar]
|
| 4. |
Orozco-Covarrubias L, Guzmán-Meza A, Ridaura-Sanz C, Carrasco Daza D, Sosa-de-Martinez C, Ruiz-Maldonado R. Scleroderma 'en coup de sabre' and progressive facial hemiatrophy. Is it possible to differentiate them? J Eur Acad Dermatol Venereol 2002;16:361-6.
[Google Scholar]
|
| 5. |
Tollefson MM, Witman PM. En coup de sabre morphea and Parry-Romberg syndrome: A retrospective review of 54 patients. J Am Acad Dermatol 2007;56:257-63.
[Google Scholar]
|
| 6. |
Narvencar KP, Jaquese-Costa AK, Patil VR. Shone's complex. J Assoc Physicians India 2009;57:415-6.
[Google Scholar]
|
| 7. |
Sharma YK, Sawhney MP, Srivastava S. Systemic sclerosis, localized morphea, en coup de sabre and aortic regurgitation: A rare association. Indian J Dermatol Venereol Leprol 2004;70:99-101.
[Google Scholar]
|
Fulltext Views
4,234
PDF downloads
3,546





