Translate this page into:
An unusual case of multiple erythematous nodules with ulcerative lesion
Correspondence Address:
Abhijeet Kumar Jha
C/O-B.K. Jha (Anish), Advocate, Krishna Nagar, Mahavir Chowk, Saharsa, Bihar - 852 201
India
| How to cite this article: Jha AK, Mallik SK, Ganguly S, Jaykar KC. An unusual case of multiple erythematous nodules with ulcerative lesion. Indian J Dermatol Venereol Leprol 2012;78:229 |
Sir,
A 32-year-old female from eastern Bihar presented with multiple firm erythematous nodules distributed mainly over the extensor surfaces of the extremities [Figure - 1]a and buttocks [Figure - 2]a. These lesions started appearing 2 years ago and were steadily increasing both in size and in number. In addition, fungating, ulcerative and verrucous growths were observed on both the heels [Figure - 3], which started 5 months ago. On examination, the peripheral nerves were normal, without hypopigmented patches or loss of sensation. There was no history of loss of weight. On asking specifically about the history of kala-azar, she revealed that she had suffered from the disease 4 years back and was improperly treated. Hematological and biochemical investigations were within normal limits. Slit-skin smear (SSS) for acid-fast bacilli was negative, but was positive for Leishman-Donovan (LD) bodies. The rK-39 test was positive and the histopathology was consistent with the diagnosis of Post Kala-Azar Dermal Leishmaniasis (PKDL). She was treated with IM sodium stibogluconate (20 mg/ kg/ day) for 4 weeks. The patient recovered completely and her skin lesions disappeared within a month [Figure - 1]b and [Figure - 2]b. A repeat SSS was negative for LD bodies. On histopathology, there was effacement of rete ridges, grenz zone and dense lymphohistiocytic infiltration [Figure - 4]a along with multiple LD bodies [Figure - 4]a and b.
 |
| Figure 1: (a) Erythematous nodules around the knees. (b) Complete resolution of knee lesions after 4 weeks |
 |
| Figure 2: (a) Lesions on the buttocks. (b) Complete resolution of lesions on the buttocks |
 |
| Figure 3: Verrucous growth on the heel |
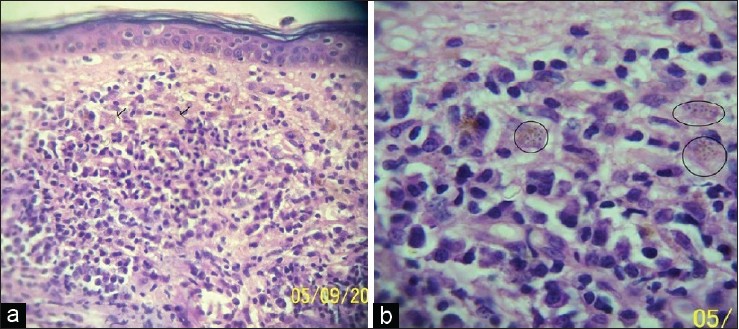 |
| Figure 4: (a) Photomicrograph showing effacement of rete ridges, grenz zone and dense lymphohistiocytic infiltration. Multiple Leishman Donovan bodies are appreciable, marked with arrow (H and E, ×100). (b) Multiple Leishman Donovan bodies are appreciable, marked with circle (H and E, ×400) |
Post kala-azar dermal leishmaniasis is a late cutaneous manifestation of leishmaniasis, first described by Brahmachari in 1922. [1] In India, the rash appears 1-2 years after recovery. [2] The early lesions are hypopigmented macules followed by diffuse nodulation. The rash is progressive over many years, and seldom heals spontaneously. The differential diagnoses of nodular lesions are leprosy, syphilis, onchocerciasis, mycosis fungoides, leukemia cutis and sarcoidosis. In PKDL, SSSs are usually positive. Histology shows a poorly differentiated infiltrate of chronic inflammatory cells, with a variable number of amastigotes in dermal macrophages.
Demonstration of LD bodies in the SSS or by culture of the skin tissue was considered to be the gold standard for the diagnosis of PKDL. [3] Recombinant DNA technology has produced serodiagnostic antigens, which include rK39, A2, ORF F, rH2A, rH2B, rGBP, rLACK and purified lipophospho-glycane (LPG). [4] We considered a differential diagnosis of histoid leprosy and mycosis fungoides for our case and ruled them out. Leishmaniasis recidivans was differentiated due to the absence of worsening of lesions during summers, and our patient was suffering from visceral leishmaniasis 2 years back without any cutaneous lesion during that period. We report this case because of the unusual features like complete absence of lesions on the face, as seen in PKDL, and ulcerative lesions on the heels. Therefore, a high index of suspicion has to be maintained in an endemic area, and PKDL should always be kept in the list of differential diagnoses.
| 1. |
Brahmachari UN. A new form of cutaneous leishmaniasis - Dermal leishmanoid. Indian Med Gazette 1927;57:125-7.
[Google Scholar]
|
| 2. |
Klotz O, Lindenberg H. The pathology of leishmaniasis of the nose. Am J Trop Med 1922;3:117-41.
[Google Scholar]
|
| 3. |
Sharma MC, Gupta AK, Verma N, Das VN, Saran R, Kar SK. Demonstration of Leishmania parasites in skin lesions of Indian post kala-azar dermal leishmaniasis (PKDL) cases. J Commun Dis 2000;32:67-8.
[Google Scholar]
|
| 4. |
Salotra P, Singh R. Challenges in the diagnosis of post kala-azar dermal leishmaniasis. Indian J Med Res 2006;123:295-310.
[Google Scholar]
|
Fulltext Views
2,107
PDF downloads
3,479





