Translate this page into:
Nails in nutritional deficiencies
Correspondence Address:
Dipankar De
Department of Dermatology, Venereology, and Leprology, Postgraduate Institute of Medical Education and Research, Chandigarh
India
| How to cite this article: Seshadri D, De D. Nails in nutritional deficiencies. Indian J Dermatol Venereol Leprol 2012;78:237-241 |
Nails are not only an important aspect of the external appearance, they are also mirrors of the internal constitution and nutritional status. Nail changes in nutritional deficiencies are mostly minor and non-specific. It is often difficult to suspect a nutritional deficiency state just by observing nail changes. In this article, we have discussed the basic contents of the nail plate and the different nail changes that can be observed in various nutritional deficiency states.
The nail apparatus consists of a horny "dead" product, the nail plate, and four specialized epithelia: the proximal nail fold, the nail matrix, the nail bed, and the hyponychium. [1] The bulk of the nail plate is constituted by hair type (hard) keratins which comprise 80% to 90% of the nail plate. Epithelial type keratins account for 10% to 20%. The overall sulphur content is approximately 10% by weight. The disulfide bonds of cystine in the matrix proteins contribute maximally to nail hardness by gluing the keratin fibers together. Calcium does not contribute to nail hardness and makes up only 0.2% of the nail plate by weight. The lipid content is relatively low compared with the lipid content of the stratum corneum. Glycolic and stearic acids are nail plate lipids and their presence contributes to the water resistance. Despite the water resistance, the hydration status of the nail plate is another factor determining its hardness. The nail plate′s water content can vary greatly, with normal content being 18%. Nails become brittle when the water content is less than 16% and become soft when greater than 25%. Minerals are another important aspect of the nail plate′s composition; mainly, magnesium, calcium, iron, zinc, sodium, and copper. [2]
Malnutrition and the Nails
Since the normal nail-plate is constituted by a variety of nutrients in certain optimum proportions, almost any nutritional deficiency can produce significant changes in the nail plate. Some nutritional anomalies can also affect the nail bed. The changes may either be visible clinically or else on biochemical investigation. For instance, it has been shown that the nails of children with kwashiorkor show an increased sodium and calcium concentration and decreased magnesium concentration. [3] The iron content of nails may be lower in patients with iron deficiency anaemia. [4] There seems to be a reasonable correlation between the body and blood levels of nutrients and their concentrations in the nail plate. It works both ways - in deficiency states nail concentrations drop while in excessive intake or toxicity, the nail concentrations rise. Nail copper concentrations are raised in Wilson′s disease. [5] Nail arsenic levels can be used to diagnose arsenic poisoning. In particular, studies have shown significant positive correlation between plasma and nail selenium levels. [6],[7]
The various clinically visible anomalies of nails that can be associated with nutritional deficiencies are discussed below.
Nail Changes in Protein and Energy Deficiency and Malnutrition in General
Kwashiorkor is a nutritional syndrome due to severe protein malnutrition with relative carbohydrate excess which results in retardation of skeletal and mental development, muscular wasting, fatty liver and oedema. Marasmus is the result of prolonged starvation, a wasting syndrome, resulting in 40-50% reduction in body weight but with no peripheral oedema. Kwashiorkor is associated with nails that are soft and thin and marasmic children have fissured nails and impaired nail growth. [8]
Another nail change reported in malnutrition is longitudinal melanonychia. Melanonychia refers to blackish discolouration of the nail plate. Longitudinal melanonychia of the nail plate occurs secondary to increased melanin production in the matrix. [2]
Muehrcke′s lines are commonly associated with hypoalbuminaemia, the correction of which by albumin infusion can reverse the sign. [9] These are paired, narrow white transverse bands reflecting abnormal nail bed vasculature. When pressure is applied to the distal plate, the narrow transverse bands disappear, i.e apparent leuconychia. [2] Leukonychia refers to whitish discolouration of the nail plate. It can be true (due to nail plate abnormality) or apparent (due to nail bed abnormality, in which case it fades on pressure). [1]
Though classically associated with liver disease, Terry′s nails can also be seen in malnutrition, especially in the elderly. [2] They consist of apparent leukonychia over the proximal nail bed with a distal pink or brown band 0.5 to 3.0 mm wide. Histology of the distal band shows mainly telangiectases and the white colour is thought to reflect hyperplasia of connective tissue between the nail and bone. [9]
Beau′s lines are among the most common yet least specific signs encountered in clinical practice. Nutritional causes include protein deficiency and the general malnourished state associated with chronic alcoholism. [2] These are transverse linear depressions in the nail plate which may be caused by any disease severe enough to disrupt normal nail growth. [10] The width of the furrow is an indicator of the given ailment′s duration. Measuring the distance from the furrow to proximal nail fold gives an approximate time when the insult may have occurred. [2]
Brittle nail syndrome (BNS) is a phenomenon which can result from a multitude of causes and they are a frequent finding in poorly nourished patients. [3],[11] BNS is characterized by soft, dry, weak, easily breakable nails that show onychorrhexis and onychoschizia. [4] Onychorrhexis refers to longitudinal splitting which begins at the free edge and extends proximally while onychoschizia is lamellar peeling of the free edge of the nail plate. [11] Brittle nails are commonly seen in patients with anorexia nervosa and they have been attributed to the starvation, idiosyncratic eating habits, and malnutrition associated with this disorder. [12] Poor food and water intake contribute to and precipitate brittle nails in the elderly. [2]
The protein-losing enteropathy of Cronkhite-Canada syndrome (intestinal polyposis, malabsorption, pigmentation, alopecia and nail defects) is associated with dystrophic nails which undergo onycholysis, onychoschizia and onychomadesis with a peculiar, triangular, residual nail plate. [13] Onycholysis is defined as separation of the nail plate from the underlying nail bed, causing a proximal extension of free air while onychomadesis describes complete onycholysis, beginning at the nail plate′s proximal end, which results in complete nail shedding. [2]
Nail Changes in Mineral Deficiencies
Iron deficiency
Although nonspecific, pallor of the nail bed can be a sign of anemia and an indication that body stores of iron may be low. [2] Koilonychia refers to a reverse curvature in the transverse and longitudinal axes giving a concave dorsal aspect to the nail. [14] It is thought to occur due to a relatively low-set distal matrix compared to the proximal matrix that causes nail plate growth to occur in a downward direction as it grows towards the nail bed. [2] Koilonychia is classically a sign of iron-deficiency anemia. [15] Koilonychia reported in post-gastrectomy patients and those with Plummer-Vinson syndrome has also been attributed to the associated iron deficiency. [2] Interestingly, it occasionally occurs in patients with hemochromatosis. [10]
Iron deficiency can also result in brittle nails, [8] onycholysis and onychorrhexis. [2]
Calcium deficiency
Transverse leukonychia of all nails can be associated with severe hypocalcemia and good response has been reported to treatment with calcium. [16] Transverse leukonychia is characterized by transverse, opaque white bands that tend to occur in the same relative position in multiple nails. Measuring the distance of the line from the proximal nail fold gives a time reference from when nail insult occurred. [2] The hypotheses proposed for development of leuconychia in hypocalcemia include induction of digital arteriolar spasm and disorganization of the hard keratin of the nail. [16]
Onychomadesis can result from the neurovascular change associated with repeated episodes of drops in blood calcium levels or a chronic state of hypocalcemia with arteriolar spasm which results in an abrupt separation of the nail plate from the underlying nail matrix and nail bed. [2]
Other nail changes reported to be associated with hypocalcemia include brittle nails with onychorrhexis and longitudinal striations. [17] Hapalonychia, or soft nails, has been associated with a variety of nutritional deficiencies including low serum calcium. [2]
Zinc deficiency
Muehrcke′s nails (described earlier) can occur in association with acrodermatitis enteropathica. [2],[5] Transverse leukonychia can also occur in acrodermatitis enteropathica and its resolution has been reported following zinc supplementation. [18] Zinc deficiency is also associated with brittle nails, [8] onychorrhexis [2] and Beau′s lines. [4]
Other mineral deficiencies
Patients with reduced plasma magnesium levels can develop soft, flaky nails that are inclined to break or split. [2] Patients on prolonged total parenteral nutrition (TPN) tend to become selenium deficient; cases have been reported where the fingernails turned white in association with low serum and urinary selenium levels and the nail changes resolved dramatically after selenium therapy was instituted. [19],[20] Clubbing of nails is associated with the cretinism caused by iodine deficiency. [2]
Nail Changes in Vitamin Deficiencies
Fat-soluble vitamins
Hapalonychia (soft nails) has been associated with deficiencies of vitamins A and D among other causes. [2] Longitudinal melanonychia of the nail plate has been reported in vitamin D deficiency. [2] No specific nail changes have been reported with vitamin E deficiency, though vitamin E has been reported to help the nail changes of yellow nail syndrome. [21]
Water-soluble vitamins
Deficiency of B vitamins
Apart from iron deficiency, riboflavin deficiency and pellagra have also been implicated in the development of koilonychia. [2] Transverse leukonychia of all nails associated with pellagra has been reported which showed a good response to treatment with vitamin B3. [22] Pellagra can also be associated with Beau′s lines and onycholysis. [2] Furthermore, a case of pellagra has been reported where the patient developed half and half nails simultaneously with the onset of the skin lesions and the lesions regressed with nicotinamide therapy. [23] Half and half nails show a proximal white zone and a distal (20-60%) brownish sharp demarcation, the histology of which suggests an increase in vessel wall thickness and melanin deposition. It is commonly associated with renal failure. [14]
Deficiency of vitamin B6 (pyridoxine) can be associated with hapalonychia. [2] Biotin deficiency leads to dystrophic nails. The inborn errors of biotin metabolism, namely holocarboxylase synthetase deficiency and biotinidase deficiency are associated with nail dystrophy and onychoschizia apart from other cutaneous and neurological symptoms. All symptoms including nail changes respond to biotin supplementation. [8]
Nail hyperpigmentation is associated with vitamin B12 deficiency and its reversal on B12 supplementation is well reported in the literature. [24],[25],[26] The morphological patterns of hyperpigmentation include longitudinal melanonychia, [25],[26] diffuse bluish discolouration (reported in two dark-skinned patients) [27] as well as reticulate pigmentation. [24] The proposed mechanism of development of hyperpigmentation involves decreased reduced glutathione levels, which results in disinhibition of tyrosinase, an enzyme of melanogenesis. [26]
Vitamin C deficiency
Splinter haemorrhages can be seen in scurvy though they are classically associated with subacute bacterial endocarditis and are most frequently caused by trauma. They are formed by extravasation of red blood cells from longitudinally oriented nail bed vessels into adjacent longitudinally oriented troughs. [2] They appear as red to black thin longitudinal lines under the nail-plate. [1] Vitamin C deficiency has also been associated with koilonychia and hapalonychia. [2]
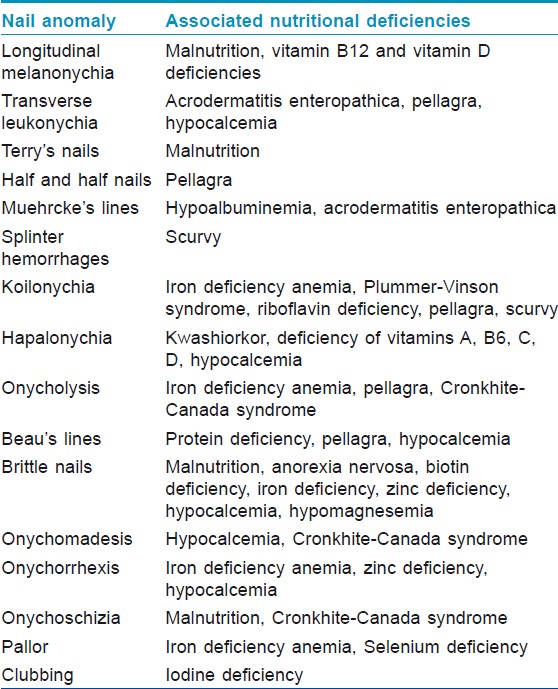
A summary of the important clinical nail anomalies and the associated nutritional deficiencies is provided in [Table - 1] since a variety of deficiencies can lead to a similar picture.
Nutritional supplements and the nails
A multitude of regimens exist for treatment of brittle nails, including biotin, application of essential fatty acids, and ingestion of vitamin C, pyridoxine, iron, vitamin D, calcium, amino acids, and gelatin. [2] Conflicting evidence exists for the use of vitamin E to treat yellow nail syndrome. [4] Other substances known to improve nail health but lacking objective evidence include gelatin, cystine, L-methionine, keratin, collagen, pantothenic acid, salt, millet, yeast, chromium and rhodanates. [4]
Extended iron supplementation appears to decrease the brittleness of already brittle nails even in patients without overt iron deficiency. Studies have also suggested that silicon supplementation can improve the appearance of brittle nails. However, the best documented so far is the use of biotin to treat BNS. Clinical trial evidence exists and the beneficial effects usually start after 2 to 3 months of supplementation. The optimal duration of the treatment has not been determined. [4] Whether supplementation is legitimately correcting an underlying biotin deficiency or improvement in nail brittleness is through some other mechanism is yet to be elucidated. [2]
An exhaustive review on the role of vitamins and minerals in nail health concluded that no evidence supports the use of vitamin supplementation for improving the nail health of well-nourished patients; brittle nail syndrome can benefit from supplementation with high dose biotin or silicon; and lastly, adequate intake of vitamins and minerals facilitates nail health. [4]
| 1. |
Tosti A, Piraccini BM. Biology of nails and nail disorders. In: Wolff K, Goldsmith LA, Katz SI, Gilchrest B, Paller AS, Leffell DJ, editors. Fitzpatrick's Dermatology In General Medicine. McGraw-Hill Companies Inc.; 2007. p. 778-94.
[Google Scholar]
|
| 2. |
Cashman MW, Sloan SB. Nutrition and nail disease. Clin Dermatol 2010;28:420-5.
[Google Scholar]
|
| 3. |
Leonard PJ, Morris WP, Brown R. Sodium, potassium, calcium and magnesium contents in nails of children with kwashiorkor. Biochem J 1968;110:22-3.
[Google Scholar]
|
| 4. |
Scheinfeld N, Dahdah MJ, Scher R. Vitamins and minerals: Their role in nail health and disease. J Drugs Dermatol 2007;6:782-7.
[Google Scholar]
|
| 5. |
Solomons NW. On the assessment of zinc and copper nutriture in man. Am J Clin Nutr 1979;32:856-71.
[Google Scholar]
|
| 6. |
Longnecker MP, Stram DO, Taylor PR, Levander OA, Howe M, Veillon C, et al. Use of selenium concentration in whole blood, serum, toenails, or urine as a surrogate measure of selenium intake. Epidemiology 1996;7:384-90.
[Google Scholar]
|
| 7. |
Satia JA, King IB, Morris JS, Stratton K, White E. Toenail and plasma levels as biomarkers of selenium exposure. Ann Epidemiol 2006;16:53-8.
[Google Scholar]
|
| 8. |
Sarkany R, Breathnach S, Morris A, Weismann K, Flynn P. Metabolic and Nutritional Disorders. In: Burns T, Breatnach S, Cox N, Griffiths C, editors. Rook's Textbook of Dermatology. John Wiley and Sons; 2010. p. 59.58-59.76.
[Google Scholar]
|
| 9. |
Ghosn SH, Kibbi AG. Cutaneous manifestations of liver diseases. Clin Dermatol 2008;26:274-82.
[Google Scholar]
|
| 10. |
Fawcett RS, Linford S, Stulberg DL. Nail abnormalities: Clues to systemic disease. Am Fam Physician 2004;69:1417-24.
[Google Scholar]
|
| 11. |
Iorizzo M, Pazzaglia M, Piraccini B, Tullo S, Tosti A. Brittle nails. J Cosmet Dermatol 2004;3:138-44.
[Google Scholar]
|
| 12. |
Gupta MA, Gupta AK, Haberman HF. Dermatologic signs in anorexia nervosa and bulimia nervosa. Arch Dermatol 1987;123:1386-90.
[Google Scholar]
|
| 13. |
Cox N, Coulson I. Systemic disease and the skin. In: Burns T, Breatnach S, Cox N, Griffiths C, editors. Rook's Textbook of Dermatology. John Wiley and Sons; 2010. p. 62.57-62.58.
[Google Scholar]
|
| 14. |
De Berker D, Baran R. Disorders of Nails. In: Burns T, Breatnach S, Cox N, Griffiths C, editors. Rook's Textbook of Dermatology. John Wiley and Sons; 2010. p. 65.1-65.17.
[Google Scholar]
|
| 15. |
Marks J, Shuster S. Anaemia and skin disease. Postgrad Med J 1970;46:659-63.
[Google Scholar]
|
| 16. |
Foti C, Cassano N, Palmieri VO, Portincasa P, Conserva A, Lamuraglia M, et al. Transverse leukonychia in severe hypocalcemia. Eur J Dermatol 2004;14:67-8.
[Google Scholar]
|
| 17. |
Simpson JA. Dermatological changes in hypocalcaemia. Br J Dermatol 1954;66:1-15.
[Google Scholar]
|
| 18. |
Reich H, Opitz K, Bertram HP, Fegeler K. Successful zinc treatment of a severe case of acrodermatitis enteropathica. Dtsch Med Wochenschr 1976;101:1724-6.
[Google Scholar]
|
| 19. |
Kien CL, Ganther HE. Manifestations of chronic selenium deficiency in a child receiving total parenteral nutrition. Am J Clin Nutr 1983;37:319-28.
[Google Scholar]
|
| 20. |
Ishida T, Himeno K, Torigoe Y, Inoue M, Wakisaka O, Tabuki T, et al. Selenium deficiency in a patient with Crohn's disease receiving long-term total parenteral nutrition. Intern Med 2003;42:154-7.
[Google Scholar]
|
| 21. |
Al Hawsawi K, Pope E. Yellow nail syndrome. Pediatr Dermatol 2010;27:675-6.
[Google Scholar]
|
| 22. |
Donald GF, Hunter GA, Gillam BD. Transverse leukonychia due to pellagra. Arch Dermatol 1962;85:530-1.
[Google Scholar]
|
| 23. |
Cakmak SK, Gönül M, Aslan E, Gül U, Kiliç A, Heper AO. Half-and-half nail in a case of pellagra. Eur J Dermatol 2006;16:695-6.
[Google Scholar]
|
| 24. |
Ridley CM. Pigmentation of fingertips and nails in vitamin B12 deficiency. Br J Dermatol 1977;97:105-6.
[Google Scholar]
|
| 25. |
Noppakun N, Swasdikul D. Reversible hyperpigmentation of skin and nails with white hair due to vitamin B12 deficiency. Arch Dermatol 1986;122:896-9.
[Google Scholar]
|
| 26. |
Niiyama S, Mukai H. Reversible cutaneous hyperpigmentation and nails with white hair due to vitamin B12 deficiency. Eur J Dermatol 2007;17:551-2.
[Google Scholar]
|
| 27. |
Carmel R. Hair and fingernail changes in acquired and congenital pernicious anemia. Arch Intern Med 1985;145:484-5.
[Google Scholar]
|
Fulltext Views
60,638
PDF downloads
4,289





