Translate this page into:
Newborn with multifocal lymphangioendotheliomatosis with thrombocytopenia
2 Department of Surgery, School of Medicine, Pontificia Universidad Cat�lica de Chile, Chile
3 Department of Pathology, School of Medicine, Pontificia Universidad Cat�lica de Chile, Chile
Correspondence Address:
Mar�a Soledad Zegpi
Vicku�a Mackenna 4686, Macul, Santiago
Chile
| How to cite this article: Zegpi MS, Zavala A, Puerto Cd, C�rdenas C, Gonz�lez S. Newborn with multifocal lymphangioendotheliomatosis with thrombocytopenia. Indian J Dermatol Venereol Leprol 2012;78:409 |
Sir,
The presence of multiple congenital vascular malformations is uncommon and if they are associated with hematologic and/or coagulation disorders, the diagnostic spectrum is reduced to two entities: Multifocal lymphangioendotheliomatosis with thrombocytopenia (MLE-T) and multiple Kaposiform hemangioendothelioma (K-HE) with Kasabach-Merritt syndrome (KM-S).
Here, the case of a newborn girl with multiple cutaneous vascular lesions, anemia, and thrombocytopenia is described and differential diagnosis is discussed.
A 53-day-old newborn girl-with an uncomplicated pregnancy delivered at 39 weeks-was born with multiple erythematous-violaceous skin lesions associated with anemia and thrombocytopenia. Skin biopsy suggested congenital hemangioma, and KM-S was suspected, therefore she was transferred to our center. On physical examination, approximately 15-20 erythematous-violaceous macules and papules were seen on the neck, trunk, and lower extremities; also, a violaceous nodule 15 mm in diameter on the right labium majus [Figure - 1]. Laboratory examinations revealed anemia (25% hematocrit), thrombocytopenia (81000 cells/μl), low fibrinogen (157 mg/dl), and elevated D Dimer (3895 ng/ml). The TORCHES study [perinatal infections (T: Toxoplasmosis), O: Other infections (HIV), R: Rubella, C: Cytomegalovirus, HE: Herpes simplex virus, and S: Syphilis] was negative. A brain echography ruled out any brain abnormality, and an abdominal echography ruled out visceral involvement. Upper and lower endoscopy revealed vascular malformations on the stomach and colon, with no signs of a hemorrhage [Figure - 1]b.
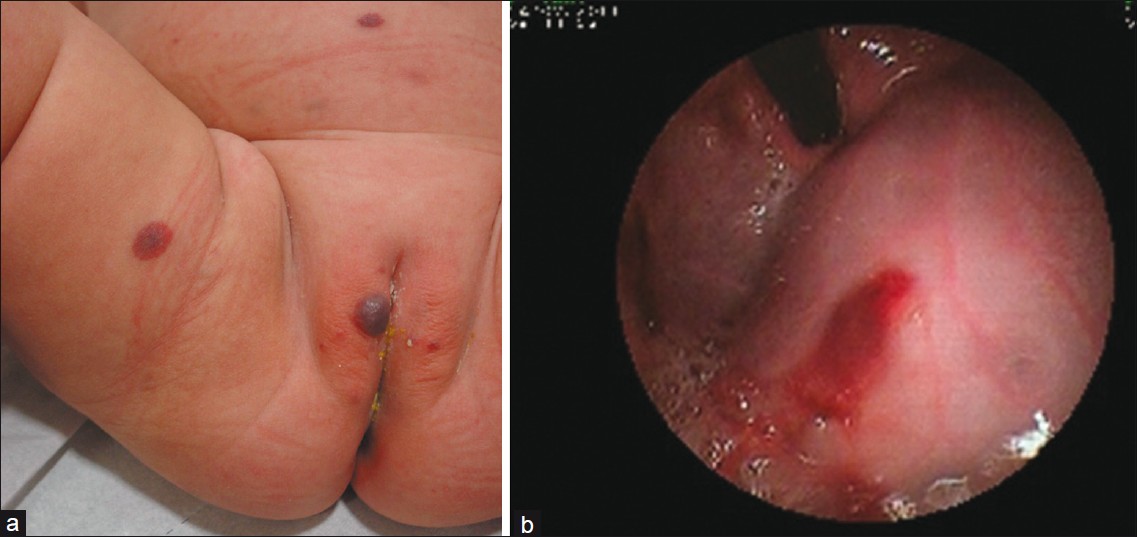 |
| Figure 1: (a) Erythematous - violaceous macules and papules on legs and abdomen and a purpuric nodule on right labium majora. (b) On upper GI endoscopy, an erythematous vascular malformation with no bleeding sings was observed |
Skin biopsy was re-examined showing a venous and capillary vascular tumor on the dermis, with telangiectasia, thrombosis, multifocal calcifications, and papillary endothelium hyperplasia with intraluminal projections [Figure - 2]. On immunohistochemistry, endothelial cells stained GLUT-1 and WT-1 negative, and D2-40 positive [Figure - 3], which was consistent with K-HE. However, clinical, laboratory and some histological findings suggested MLE-T.
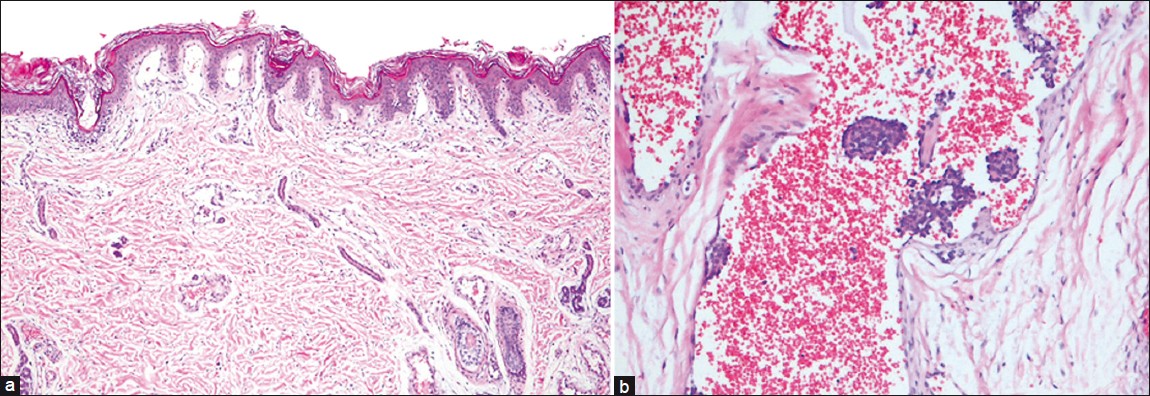 |
| Figure 2: (a) A low magnification of the lesion shows superficial and deep vascular lesions, some sub-epidermal telangiectasia and an increased number of vessels on dermis (H and E, ×100). (b) On dermis, dilated vessels, some with calcified occlusions, others with thrombi, and yet others with a papillary aspect of endothelium hyperplasia towards the vascular lumen. These findings are characteristic of lymphatic differentiated lesions (H and E, ×200) |
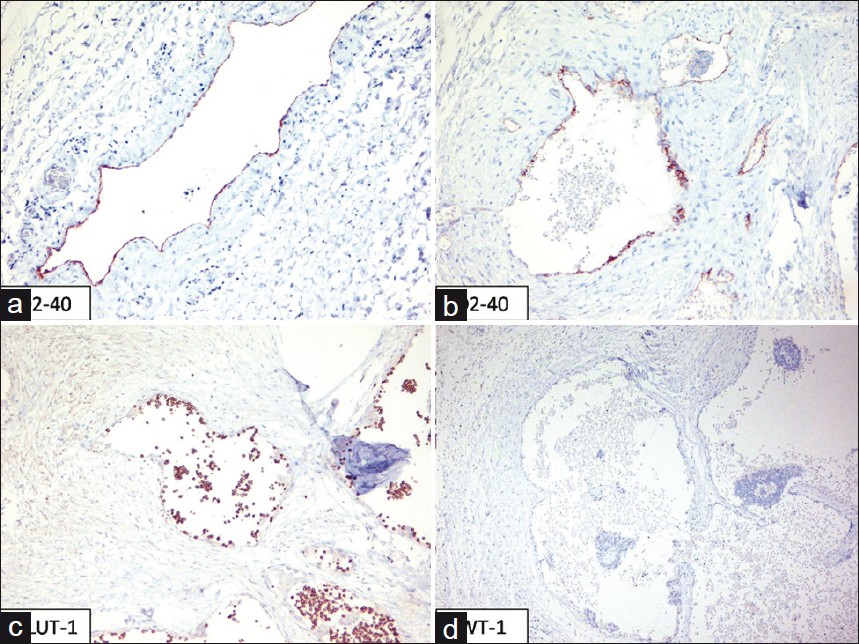 |
| Figure 3: Endothelial cells stain positive for D2 - 40 (a) D2 - 40 Positive control (b) (magnification, �200) (c), and WT-1 (d) and negative for GLUT-1 |
MLE-T was described in 2004 by Norton et al. [1] Since then, 13 cases have been reported in the literature. [2] MLE-T is characterized by multiple (few up to hundreds) vascular skin lesions since birth, which progressively grow in size and number. [1] Vascular lesions include red-brown macules and flat or indurated papules, some with central pallor and others with central scar-like areas. [1] MLE-T develops vascular gastrointestinal malformations, producing bleeding in variable quantity, ranging from silent anemia to massive bleeding, with one fatal case reported. Hemorrage may be present since birth [3] up to the first 2-3 years of age. [2] MLE-T also presents refractory thrombocytopenia that worsens with transfusions. [3],[4] In MLE-T vascular lesions may appear in other organs, eg, lungs, thyroid gland, liver, kidneys, brain, etc. [4]
Histologically, MLE-T shows elongated vessels with thin walls of a single layer of endothelial cells, with papillary intraluminal projections. [1],[4] Endothelial cells stain negative for GLUT-1 and positive for lymphatic markers D2-40 and LYVE-1. [2]
K-HE, first described in 1993 by Zukerberg et al., [5] is a vascular neoplasm with local aggressiveness. Most cases of K-HE arise within the first 10 years, though adult K-HE cases have also been described. [6] K-HE usually develops KM-S and lymphangiomatosis, especially in children. K-HE compromises skin (75% of cases) [6] and retroperitoneum (18% cases). [2],[7] An indurated, erythematous-purpuric plaque is its most characteristic skin lesion. Other skin findings include purpuric macules, papules with telangiectasia, and deep nodules. [6],[8] Most K-HE cases have a single lesion, [6] though one case with multiple cutaneous lesions [8] and four [9] involving different organs have been described. Gastrointestinal compromise has been described in one case. [10]
Histologically, K-HE shows endothelial spindle cells surrounding crescentic vessels containing hemosiderin granules and thrombi. On immunohistochemistry, endothelial cells stain positive for D2-40 and negative for GLUT-1.
Although both entities are associated with coagulopathy, their mechanisms are different. MLE-T coagulopathy is due to chronic coagulation within the abnormal tumor vessels and consumption of coagulation factors, [2] showing D dimer elevation, slight thrombocytopenia, and minor fibrinogen reduction. In contrast, in K-HE, coagulopathy occurs due to KM-S with severe thrombocytopenia, important fibrinogen reduction, and slight D dimer elevation.
MLE-T and K-HE share similar clinical and histological findings. The presented case had clinical and laboratory findings suggestive of MLE-T. However, histological findings-mainly the presence of thrombi, telangiectasia, calcifications, and lymphatic differentiation-have already been described in K-HE lesions. Therefore, this case was compatible with both entities. Nevertheless, since clinical and laboratory findings were distinctive of MLE-T, the diagnosis was made.
In conclusion, MLE-T and K-HE share similar clinical and histological characteristics, and they both express D-240 in their cells suggesting a lymphatic differentiation. Therefore, we believe that these may be two clinical-pathologic variations of the same entity.
| 1. |
North PE, Kahn T, Cordisco MR, Dadras SS, Detmar M, Frieden IJ. Multifocal Lymphangioendotheliomatosis with Thrombocytopenia. Arch Dermatol 2004;140:599-606.
[Google Scholar]
|
| 2. |
Campbell CM, Beckum KM, Hammers YA, North PE, Drolet BA, Theos A. Multiple congenital red-brown macules, thrombocytopenia, and gastrointestinal bleeding. Diagnosis: Multifocal lymphangioendotheliomatosis with thrombocytopenia (MLT). Pediatr Dermatol 2010;27:395-6.
[Google Scholar]
|
| 3. |
Piggott KD, Riedel PA, Baron HI. Multifocal lymphangioendotheliomatosis with thrombocytopenia: A rare cause of gastrointestinal bleeding in the newborn period. Pediatrics 2006;117:e810-3.
[Google Scholar]
|
| 4. |
Maronn M, Catrine K, North P, Browning MB, Kerschner JE, Noel R, et al. Expanding the phenotype of multifocal lymphangioendotheliomatosis with thrombocytopenia. Pediatr Blood Caner 2009;52:531-4.
[Google Scholar]
|
| 5. |
Zukerberg LR, Nickoloff BJ, Weiss SW. Kaposiform hemangioendothelioma of infancy and childhood. An aggressive neoplasm associated with Kasabach-Merritt syndrome and lymphangiomatosis. Am J Surg Pathol 1993;17:321-8.
[Google Scholar]
|
| 6. |
Vetter-Kauczok CS, Ströbel P, Bröcker EB, Becker JC. Kaposiform hemangioendothelioma with distant lymphangiomatosis without an association to Kasabach-Merritt-Syndrome in a female adult! Vasc Health Risk Manag 2008;4:263-6.
[Google Scholar]
|
| 7. |
Tsang WY, Chan JK. Kaposi-like infantile hemangioendothelioma. A distinctive vascular neoplasm of the retroperitoneum. Am J Surg Pathol 1991;15:982-9.
[Google Scholar]
|
| 8. |
Gianotti R, Gelmetti C, Alessi E. Congenital cutaneous multifocal kaposiform hemangioendothelioma. Am J Dermatopathol 1999;2:557-61.
[Google Scholar]
|
| 9. |
Veening MA, Verbeke JI, Witbreuk MM, Kaspers GJ. Kaposiform (spindle cell) hemangioendotelioma in a child with an unusual presentation. J Pediatr Hematol Oncol 2010;32:240-2.
[Google Scholar]
|
| 10. |
Burgos L, Gutiérrez JC, Barrena S, De la Torre C, Suárez O, Luis AL. Atypical vascular tumors of the gastrointestinal tract: Four uncommon cases. Cir Pediatr 2009;22:125-7.
[Google Scholar]
|
Fulltext Views
2,545
PDF downloads
2,373





