Translate this page into:
Bullous pilomatricoma: A stage in transition to secondary anetoderma?
Correspondence Address:
Premanshu Bhushan
Skin Institute and School of Dermatology, N-Block, Greater Kailash-1, New Delhi-110048
India
| How to cite this article: Bhushan P, Hussain SN. Bullous pilomatricoma: A stage in transition to secondary anetoderma?. Indian J Dermatol Venereol Leprol 2012;78:484-487 |
Abstract
Pilomatricoma is an uncommon hamartomatous tumor of the hair matrix. Bullous and anetodermic changes over pilomatricoma are rare. We report an 18-year-old male with an asymptomatic nodule with overlying cystic changes on the left arm of 6-month duration with clinical and histological features of both bullous and anetodermic modifications. We also reviewed the associated literature to conclude that there is sufficient overlap in these two entities. Both variants show a bullous or pseudobullous appearance clinically and loss of elastin, sparse collagen bundles separated by intense edema, and dilated lymphatics/blood vessels in the dermis overlying the tumor mass histologically. We therefore propose that bullous, pseudoampullary, anetodermic, and lymphangiectatic forms should be considered as synonymous or transitional to the ultimate scar-like anetodermic appearance.Introduction
Pilomatricoma (pilomatrixoma) is a benign hamartoma of the hair matrix presenting as a deep-dermal nodule usually situated on the head, neck, or upper extremities. Like other matricial neoplasms, mutations in genes encoding β-catenin have been reported in pilomatricomas. [1] Pilomatricomas may rarely be associated with syndromes or the overlying skin may be bullous or anetodermic. We report a rare case of multilocular bullous pilomatricoma associated with features of anetoderma. In view of the clinical and histological overlaps as outlined in this article, we argue that these variants should be considered synonymous or transient stages in the final outcome of anetodermic pilomatricoma.
Case Report
An 18-year-old male student presented with a solitary, firm, asymptomatic nodule on the lateral aspect of the left arm which enlarged over 6 months and cystic appearance was noticed on the overlying skin for the last 3 months. There was no history of any local trauma, scratch, or injection. Personal, past, and family history was unremarkable.
The skin overlying the nodule demonstrated erythematous, tense, thick-walled bullae, organized into two distinct sacs of 3 × 3 and 1.5 × 2 cm [Figure - 1]a. However, when vertical pressure was applied on the distal (smaller) sac or lateral pressure around the lesion, sacs became flaccid, simulating collapsed blisters [Figure - 1]b and depressed in the center (dimple sign) [Figure - 1]c. A finger could be inserted vertically into the larger sac which disappeared through a deep hernia-like defect in dermis (buttonholing) [Figure - 1]d. Beneath the sac-like protrusions, a deep nodular, non-tender, firm to hard mass of approximately 3 × 4 cm was palpated. There was no regional lymphadenopathy and rest of physical and systemic examination was normal. Blood counts, urinalysis, and serum biochemistry including serum calcium were normal.
 |
| Figure 1: Clinical findings. (a) Tense, erythematous bullae overlying a nodular mass on the left arm. (b) Blister collapsing into a loose sac on pressing the smaller blister. (c) Lesion dimpling on lateral pressure. (d) Lesion allowing buttonholing on vertical pressure |
A clinical suspicion of bullous/anetodermic pilomatricoma and bullous morphea was made. Initially routinely stained sections of a punch biopsy from the smaller bulla showed perivascular lymphohistiocytic dermal infiltrate, dilated lymphatics, with marked edema leading to disruption and separation of collagen bundles [Figure - 2]a with near total loss of elastic fibers, and mild collagen disruption on the Verhoeff-Van Gieson stain [Figure - 2]b. A histopathological impression of anetoderma was made. Considering the slow growth of the tumor, a curative excisional biopsy was performed under local anesthesia.
Macroscopic examination revealed an excised tissue measuring 1.5 x 3 cm in size with a large multiloculated bulla in close approximation to the overlying skin. A well-defined, hard tumor was present in the deeper layers of the dermis with a chalky white cut surface and lobulated appearance [Figure - 3]. On microscopic examination, sections showed normal epidermis with underlying dilated lymphatic channels lined by flattened endothelial cells surrounded by sparse lymphocytic infiltrate [Figure - 4]a. The well circumscribed tumor showed both basophilic cells and shadow (ghost) cells appearing as collections of pale staining cells with no cellular or nuclear details [Figure - 4]b. A final diagnosis of bullous pilomatricoma with anetoderma was made.
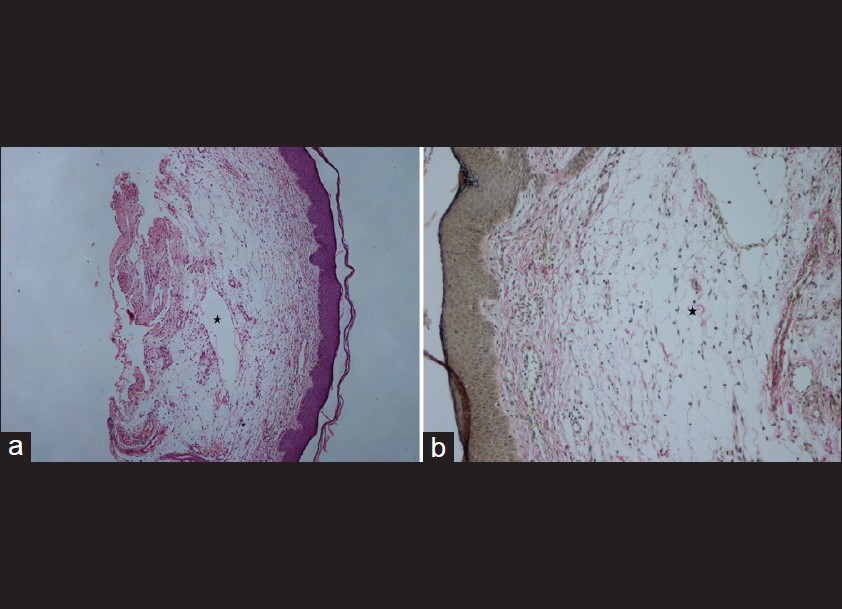 |
| Figure 2: Histopathological findings of punch biopsy specimen. (a) Dilated lymphatics (*) in upper dermis, with marked edema leading to disruption and separation of collagen bundles (H and E, ×40). (b) Near total loss of elastic fibers (*) and mild collagen disruption (Verhoeff-Van Gieson stain, ×100) |
 |
| Figure 3: Gross specimen of excised material showing multilocular bullae nearing epidermis and a solid tumor present in the deep dermis with a chalky white cut surface and lobulated appearance |
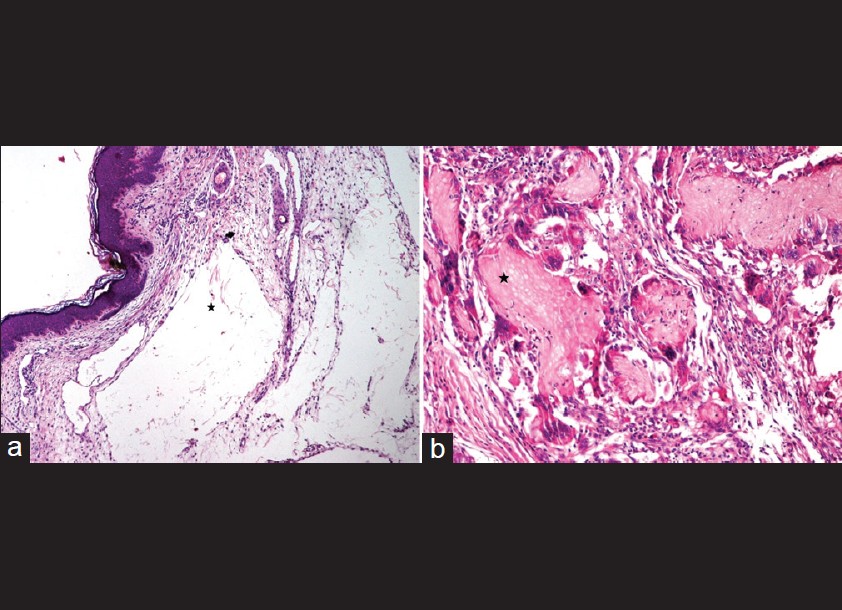 |
| Figure 4: Histopatholgical findings of excised tissue. (a) Normal epidermis with underlying dilated lymphatic channels (*) lined by flattened endothelial cells surrounded by sparse lymphocytic infiltrate (H and E, ×100). (b) The well-circumscribed tumor showed both basophilic cells and shadow (ghost) cells (*) appearing as collections of pale staining cells with no cellular or nuclear details (H and E, × 400) |
Discussion
Bullous pilomatricoma is rare and a recent review identified only 16 reports of bullous pilomatricoma mostly affecting the 10-20 years age group. [2] Clinical characteristics of bullous pilomatricoma reported include semitransparent, erythematous, bluish, or skin colored, heavily folded or striae-like flaccid blisters overlying a solitary firm to hard nodule. [2],[3] The bullous form is seen mainly on the shoulder and upper limbs in contrast to head and neck for non-bullous pilomatricoma. [2] The dimpling sign as seen in our case has been previously reported in pilomatricoma and some other tumors besides the classical dermatofibroma. [4]
Anetodermic pilomatricoma or lymphangiectatic pilomatricoma is also rarely reported and probably constitute 2% of pilomatricomas. [5] Though it is more commonly reported in the elderly, the appearance may be similar. The lesions have been described as rapidly growing erythematous bullae, [5] nodular-cystic lesions with loosely folded erythematous surface, [6] soft, atrophic, pink translucent skin, [7] pink to translucent, atrophic, scar-like skin, [8] or soft-wrinkled pedunculated lesion over firm subcutaneous mass. [9] Thus, it appears that both bullous and anetodermic variants reported in the literature have similar nodulocystic, bullous lesions. In our case, the patient had bullous lesions showing the dimpling sign as well as the classical buttonholing sign of anetoderma.
Histopathological hallmarks of pilomatricoma are the basophilic cells and eosinophilic shadow cells. [1] The bullous variant in addition shows dilated lymphatic vessels and intense lymphedema in the superficial dermis as a common pathologic feature. [2],[3],[10] Focal loss or marked reduction of elastic fibers in the dermis above the pilomatricoma-mimicking anetoderma is also seen. [3],[10] Collagen fiber disruption has also been observed in 7 of 16 cases reported. [2] Anetoderma also has histological hallmark evidence of focal loss of elastic fibers. Anetodermic pilomatricoma and its bullous appearance are also reportedly associated with attenuated collagen and loss of elastic fibrils. [6],[7],[8],[9],[11] Furthermore, dilated lymphatic vessels in the overlying dermis, [11] accentuated dermal vasodilatation, [6] edematous dermis, [8] dilated blood, and lymphatic vessels [5] are also reported in anetodermic variants of pilomatricoma. Thus, the essential histological pictures of both anetodermic and bullous variants are similar. In our case, both the lymphatic dilatation and lack of elastic tissue could be demonstrated.
The etiopathogenesis of bullous change in pilomatricoma is not yet well understood. It is believed to be a passive process as a result of physical obstruction by the tumor with resultant lymphedema or as a result of elastinolytic enzymes produced by the infiltrating cells leading to lack of support and consequent lymphangiectasia/lymphedema or probably as a combination of the two. [2] Molecular characterization of anetodermic pilomatricoma with a bullous appearance also suggests that this development is more likely to be mechanical forces disrupting the dermal integrity rather than any intrinsic property of the tumor cells. [11]
Overall, our case of bullous pilomatricoma with clinical as well as histological features of anetoderma suggests that these entities have significant overlap. Similar convergence was also noted in the reports of these cases in the literature. Inui et al. also observed that Anglo-French literature refers to bullous pilomatricoma as secondary anetoderma over pilomatricoma. [12] It is possible to hypothesize that with time, the bullous nature will reduce and predominantly anetodermic picture will emerge as a result of collagen disruption and elastic fiber loss. We agree with Inui et al. and therefore propose that bullous pilomatricoma should be considered as synonymous or as a stage in transition to the ultimate anetodermic pilomatricoma.
| 1. |
McCalmont TH. Adnexal neoplasms. In: Bolognia JL, Jorizzo JL, Rapini RP, editors. Dermatology. 2nd ed. Gurgaon: Mosby; 2009. p. 1698-9.
[Google Scholar]
|
| 2. |
Chen SY, Wu F, Qian Y, Zhu L, Tu YT, Huang CZ. Pilomatricoma with bullous appearance: A case report and review of literature. Int J Dermatol 2011;50:615-8.
[Google Scholar]
|
| 3. |
De Giorgi V, Alfaioli B, Massi D, Gori A, Sestini S, Papi F, et al. Bullous pilomatricoma: A particular and rare dermal bullous disorder. Acta Derm Venereol 2009;89:189-90.
[Google Scholar]
|
| 4. |
Meffert JJ, Peake MF, Wilde JL. 'Dimpling' is not unique to dermatofibromas. Dermatology 1997;195:384-6.
[Google Scholar]
|
| 5. |
Fernandes BF, Al-Hinai A, Belfort RN, Castiglione E, Arthurs B, Burnier MN Jr. Anetodermic variant of a periorbital pilomatricoma. Ophthal Plast Reconstr Surg 2008;24:419-21.
[Google Scholar]
|
| 6. |
De Souza EM, Ayres Vallarelli AF, Cintra ML, Vetter-Kauczok CS, Brocker EB. Anetodermic pilomatricoma. J Cutan Pathol 2009;36:67-70.
[Google Scholar]
|
| 7. |
Fujioka M, Gozo N, Osamu M, Tsuneyuki Y, Takehisa Y. Secondary anetoderma overlying pilomatrixomas. Dermatology 2003;207:316-8.
[Google Scholar]
|
| 8. |
Jones CC, Tschen JA. Anetodermic cutaneous changes overlying pilomatricomas. J Am Acad Dermatol 1991;25:1072-6.
[Google Scholar]
|
| 9. |
Shames BS, Nassif A, Bailey CS, Saltzstein SL. Secondary anetoderma involving a pilomatricoma. Am J Dermatopathol 1994;16:557-60.
[Google Scholar]
|
| 10. |
Yiqun J, Jianfang S. Pilomatricoma with a bullous appearance. J Cutan Pathol 2004;31:558-60.
[Google Scholar]
|
| 11. |
Li L, Zeng Y, Fang K, Xiao Y, Jin H, Ray H, et al. Anetodermic pilomatricoma: Molecular characteristics and trauma in the development of its bullous appearance. Am J Dermatopathol 2012;34:e41-5.
[Google Scholar]
|
| 12. |
Inui S, Kanda R, Hata S. Pilomatricoma with a bullous appearance. J Dermatol 1997;24:57-9.
[Google Scholar]
|
Fulltext Views
3,740
PDF downloads
1,654





