Translate this page into:
Panniculitis associated with Sjögren's syndrome
2 Department of Dermatology, Shuang Ho Hospital, Taipei Medical University, New Taipei City, Taiwan
Correspondence Address:
Ming-Hsiu Lin
Department of Dermatology, Shuang Ho Hospital, Taipei Medical University, No.291, Jhongjheng Rd, Jhonghe District, New Taipei City
Taiwan
| How to cite this article: Huang YC, Lin MH. Panniculitis associated with Sjögren's syndrome. Indian J Dermatol Venereol Leprol 2012;78:491-493 |
Sir,
Various cutaneous manifestations are occasionally associated with Sjögren′s syndrome (SS) including purpura and urticaria, usually with either a leukocytoclastic, or with lymphocytic vasculitis. [1] Panniculitis associated with SS is a rare cutaneous manifestation. Here, we report a case of a SS patient with septal panniculitis.
A 32-year-old male patient presented himself with a 3-month history of tender, indurated nodules and plaques on bilateral legs. He denied other family history and drug history. Review of systems showed the findings of arthralgia, dry eyes and dry mouth. He did not have cough, sore throat and fever. The result of the physical examination showed several erythematous nodules and plaques over anterior and lateral aspect of bilateral legs, and fine scales over some plaques [Figure - 1].
 |
| Figure 1: Several tender erythematous plaques over the lateral aspect of lower leg. The arrow pointed the lesion of incisional biopsy |
The findings of laboratory tests showed a positive anti-nuclear antibody (Ab) (1: 2560 with a speckled pattern), anti-Ro antibody (> 240.00 IU/mL), anti-La antibody (45.10 IU/mL), rheumatoid factor (165.0 IU/ mL), elevated erythrocyte sedimentation rate (94 mm/h), and decreased hemoglobin (12.3 g/ dL). Test results for liver and renal function, urine analysis, anti-double strand DNA Ab, anti-Sm Ab, anti-RNP Ab, anti-cardiolipin Ab and complement were all within normal limits. The result of chest X-ray film was normal. A Schirmer′s test was performed and showed the finding of 1 mm on bilateral eyes. Sialoscintigraphy showed the findings of impaired parenchymal and excretory function of bilateral parotid glands and submandibular salivary glands. He received the diagnosis of SS. Histological examination of the skin specimen revealed the finding of mild basal vacuolization with perivascular and periappendageal lymphohistiocytic infiltrate in the dermis. There was a septal lymphohistiocytic panniculitis [Figure - 2] and [Figure - 3]. Direct immunofluorescence (DIF) staining showed the picture of deposition of granular C3 along the dermoepidermal (DE) junction and positive nuclear IgG stain in the keratinocyte without any dermal vessels deposit. His cutaneous lesions resolved after he received celecoxib and colchicine for 6 weeks. He continuously received hydroxychloroquine for controlling his underlying SS.
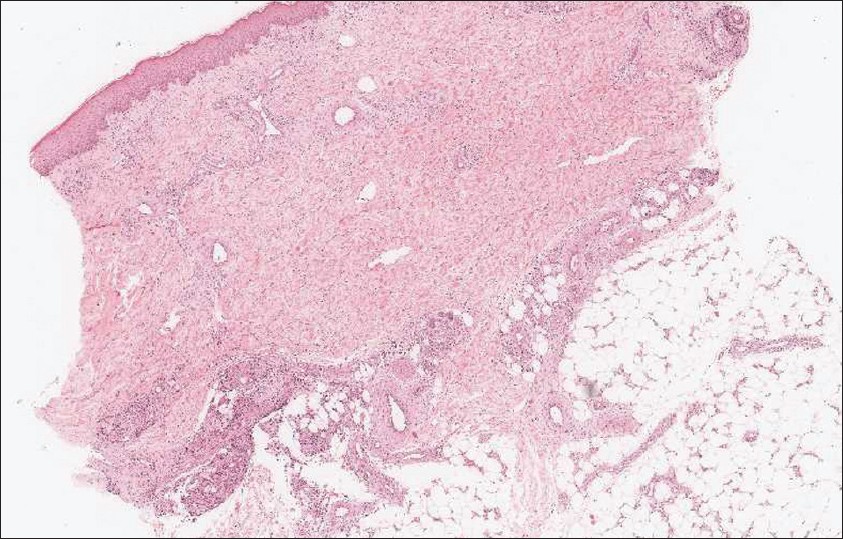 |
| Figure 2: Low power view of skin biopsy showed perivascular and periappendage inflammatory cells infiltration and septal panniculitis (H and E, ×40) |
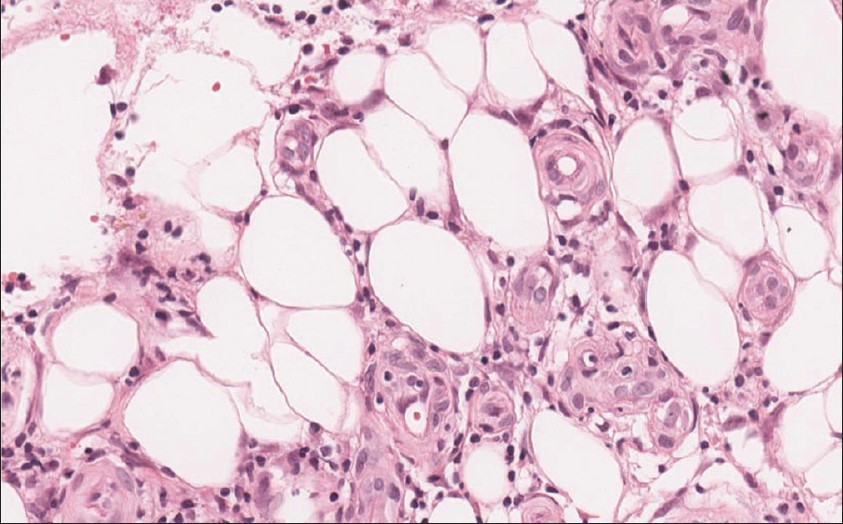 |
| Figure 3: Lymphohistiocytic infiltration within subcutaneous adipose tissue (H and E, ×400) |
The clinical differential diagnosis of this patient included erythema nodosum (EN), lupus profoundus and other kinds of panniculitis. The pathological examination showed the finding of septal panniculitis with interface change, mild perivascular lymphohistiocytic infiltration in the dermis and positive DIF. All of these findings highly implied connective tissue disease-related panniculitis. The lupus panniculitis should be considered as the first differential diagnosis. But, we did not see the typical pathological change in lupus panniculitis, such as lobular panniculitis and hyalinized fat necrosis with negative reaction in the mucin staining. Clinically, we could exclude infectious diseases (streptococcal infection and Mycobacterium tuberculosis) and other connective tissue disease such as dermatomyositis and rheumatoid arthritis, which might trigger panniculitis.
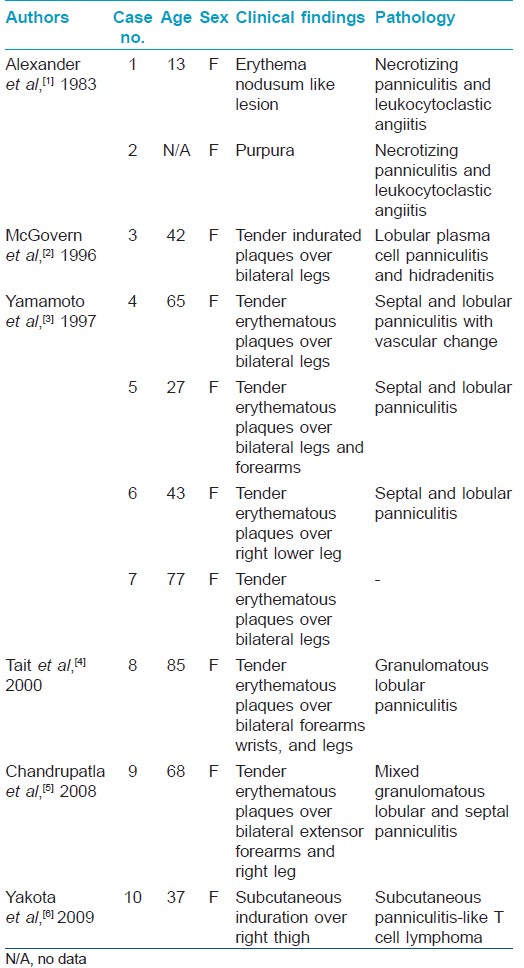
Panniculitis associated with SS is a rare cutaneous manifestation. Only 9 cases (and 1 with subcutaneous panniculitis-like T cell lymphoma) have been reported in the English literature. [Table - 1] summarizes the clinical and pathological characteristics of these patients. The clinical manifestation usually shows multiple tender erythematous plaques, most commonly over the extremities with symmetrical distribution. The histopathology of panniculitis varies, and mixed lobular and septal panniculitis is most common. The clinical or pathological findings in our patient were both compatible with the SS-related panniculitis.
To our best knowledge, an interface change and positive DIF in our patient have not been reported in the literature. We suggested that like lupus and dermatomyositis panniculitis, SS-related panniculitis could be accompanied with epidermal and dermal change. Based on the observation of our patient and the reports in the literature, we suggested that these pathological changes highly implied connective tissue disease, which is mostly related to the patient′s underlying SS.
We have reported this case to reinforce the relation between SS and panniculitis. The panniculitis could precede the diagnosis of SS. Connective tissue disease, not only the more common lupus erythematosus and dermatomyositis but also SS, should be kept among the differential diagnoses of otherwise unexplainable panniculitis.[6]
| 1. |
Alexander EL, Provost TT. Cutaneous manifestations of primary Sjögren's syndrome: A reflection of vasculitis and association with antiRo (SSA) antibodies. J Invest Dermatol 1983; 80:386-91.
[Google Scholar]
|
| 2. |
McGovern TW, Erickson AR, Fitzpatrick JE. Sjögren's syndrome plasma cell panniculitis and hidradenitis. J Cutan Pathol 1996; 23: 170-4.
[Google Scholar]
|
| 3. |
Yamamoto T, Yokoyama A, Yamamoto Y, Mamada A. Erythema nodosum associated with Sjögren's syndrome. Br J Rheumatol 1997:36:707-8.
[Google Scholar]
|
| 4. |
Tait CP, Yu LL, Rohr J. Sj¨ gren's syndrome and granulomatous panniculitis. Australas J Dermatol 2000; 41:187-9.
[Google Scholar]
|
| 5. |
Chandrupatla C, Xia L, Stratman EJ. Granulomatous panniculitis associated with Sjögren syndrome. Arch Dermatol 2008; 144: 815-6.
[Google Scholar]
|
| 6. |
Yokota K, Akiyama Y, Adachi D, Shindo Y, Yoshida Y, Miyoshi Fy et al. Subcutaneous panniculitis-like T-cell lymphoma accompanied by Sjo¨gren's syndrome. Scand J Rheumatol 2009;38:494-5
[Google Scholar]
|
Fulltext Views
3,874
PDF downloads
1,269





