Translate this page into:
Highly aggressive Buschke-löwenstein tumor of the perineal region with fatal outcome
Correspondence Address:
Zoran Radovanovic
Department of Surgical Oncology, Oncology Institute of Vojvodina, Institutski put 4, Sremska Kamenica
Serbia
| How to cite this article: Radovanovic Z, Radovanovic D, Semnic R, Nikin Z, Petrovic T, Kukic B. Highly aggressive Buschke-löwenstein tumor of the perineal region with fatal outcome. Indian J Dermatol Venereol Leprol 2012;78:648-650 |
Sir,
Giant condyloma acuminatum, better known as Buschke-Löwenstein tumor (BLT), is a rare disease caused by human papillomavirus (HPV) with an incidence of 0.1% in general population and a male-to-female ratio of 2.7:1. [1],[2] It is characterized by invasive growth and high recurrence rate after treatment, with possible malignant transformation. Although it was first described by Buschke and Löwenstein in 1925, there are still many controversies regarding the treatment of this disease. We report a case of male patient who died due to complications of BLT of the perianal region.
A 63-year-old male patient presented to the outpatient clinic of our hospital complaining of a large perianal mass that he had for 3 years. The mass grew slowly, but the patient had been embarrassed to seek medical help. Finally, due to pain, pus-like discharge, bleeding, and intolerable fetid odour, the patient was forced to come to the hospital. He was in a poor condition and examination revealed large cauliflower-like tumor mass measuring 12 × 9 cm 2 in the perianal and left gluteal region, with many fistulas spreading to the gluteal region on both sides followed by infection and pus discharge [Figure - 1]. Incisional biopsy confirmed giant condyloma on histology. Colonoscopy and CT scan showed perineal localization of the tumor without extension to the pelvis and invasion of other structures. An extensive surgical excision was performed with en bloc removal most of the fistulas. Due to infection, the wound was left opened for secondary healing. Colostomy was performed to prevent fecal contamination and facilitate healing.
 |
| Figure 1: BLT of the left gluteal and perianal region |
Histopathological examination of the resected tumor revealed papillomatosis, hyperkeratosis, parakeratosis, acanthosis, and mild koilocytosis [Figure - 2]. The keratinocytes appeared well differentiated, stained lightly with eosin, and possessed a small nucleus. The ratio of nucleus-to-cytoplasm was low. There was no vascular and perineural invasion, nuclear atypia neither loss of polarity, but individual cell keratinization and horn pearls were present. The basal cell layer of invasive strands was composed of typical well-developed cells, and the basal membrane was intact. In stroma, one could find a dense lymphocytic infiltrate. Many samples were taken and nowhere one could find criteria for squamous cell carcinoma within BLT.
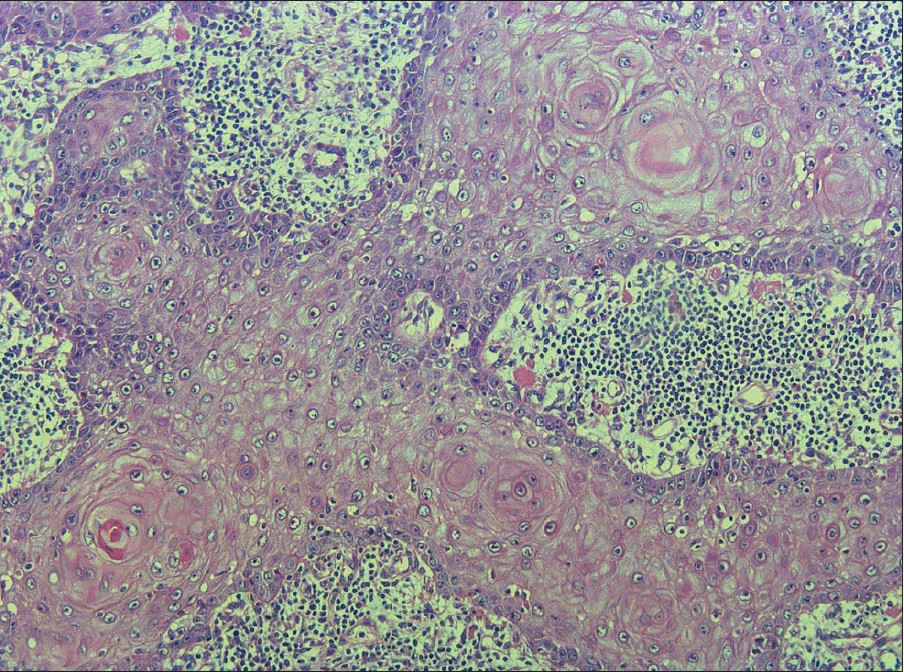 |
| Figure 2: Histological section shows condylomata acuminata with the propensity to ulcerate and infiltrate into deeper tissues. Pathological changes included papillomatosis, hyperkeratosis, parakeratosis, hyperacanthosis, and mild koilocytosis (H and E, ×100) |
The patient was regularly followed up and 3 months after the operation, suspected local recurrence was noted. The patient received four treatments of chemotherapy with a combination of 5-fluorouracil (5-FU) plus cisplatin (CDDP) and external beam irradiation (25 Gy in five fractions through three portals). However, control MRI examination showed double-sized recurrent tumor with invasion of complete perineal floor, anocutaneous and presacral space up to the S3 level. The patient died due to septic complications 11 months after initial diagnosis [Figure - 3] and [Figure - 4].
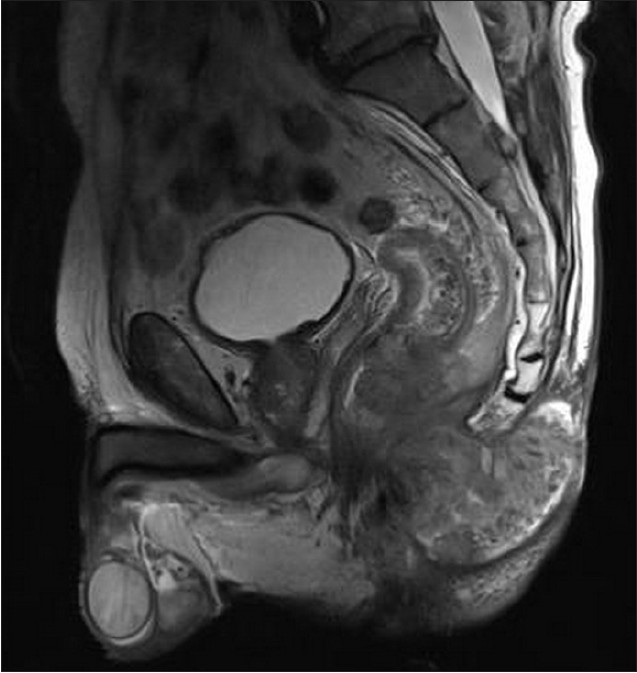 |
| Figure 3: T2 TSE 4 mm thick sagital images of the pelvis (3T imager Trio Siemens). Recurrent aggressive tumor of the gluteal region with invasion of precoccygeal space and perirectal fascia infiltration at 8 cm above the anocutaneous line. Broad intraluminal extension in rectum can be seen. Other segments of rectal wall are uniformly thickened. Perineal floor musculature is dislocated, but not invaded. Bony structures are without infiltration. Tumor is heterogenous in structure with dominant fibrous component. Obturator lymph nodes are enlarged - 13 mm (not shown) |
 |
| Figure 4: Control MRI examination 5 months after (the same MRI protocol and MR imager). Double-sized recurrent tumor with invasion of complete perineal floor, anocutaneous, and presacral space up to the S3 level. Extended invasion of the rectum |
The hallmark of BLT is the high rate of recurrence and malignant transformation. In analysis of 42 cases reported in the literature, Chu et al. found 66% recurrence rate and transformation into squamous cell carcinoma in 55% of cases with overall mortality of 20% (all occurring in patients with recurrence). [3] Similar to the majority of reported cases, our patient was not immunocompromised and appeared to have no other special risk factors other than the long delay in seeking treatment. However, growth of the recurrent tumor was fast and treatment modalities were unsuccessful. Sobrado et al. also reported a similar case of rapid tumor recurrence 1 month after surgical excision. [4]
The optimal treatment for BLT is still being debated because of the lack of a consistent series of patients. Without well-defined treatment protocol for BLT, many treatment options can be found in the literature with very different results. In some cases, radiotherapy can be successful, even total regression can be seen, but there are evidence of anaplastic transformation and extensive appearance of new condylomas after its use. Without clear recommendation regarding dose and fractions, the use of radiotherapy is controversial. Some other modalities are often used like: cryosurgery, CO 2 laser surgery, podophyllin, intralesional bleomycin, 13-cis retinoic acid, systemic chemotherapy, topical 5-FU, imiquimod, and interferon-α. [5] Because of the lack of demonstrated effectiveness of these modalities, especially in large lesions, front-line management of BLT includes radical surgical excision. Even with radical surgery, the risk of recurrence is high because of the potential spillage of tumor cells during the operation. [3]
In summary, BLT is easily diagnosed as long as one is aware of its clinical existence and characteristic macroscopic and histological appearances. Before treatment, tumor biopsy and CT or MRI need to be performed to confirm diagnosis and determine the extent of invasion. Although there have been reports of successful treatment with various more conservative modalities, failure seems to be more common, and the treatment of choice remains surgery. Adjuvant treatment with chemo- and radiotherapy was unsuccessful in our case. Local recurrence is likely, therefore adequate follow-up is essential.
| 1. |
Hicheri J, Jaber K, Dhaoui MR, Youssef S, Bouziani A, Doss N. Giant condyloma (Buschke-Löwenstein tumor). A case report. Acta Dermatovenerol Alp Panonica Adriat 2006;15:181-3.
[Google Scholar]
|
| 2. |
Trombetta LJ, Place RJ. Giant condyloma acuminatum of the anorectum: Trends in epidemiology and management: Report of a case and review of the literature. Dis Colon Rectum 2001;44:1878-86.
[Google Scholar]
|
| 3. |
Chu QD, Vezeridis MP, Libbey NP, Wanebo HJ. Giant condyloma acuminatum (Buschke-Lowenstein tumor) of the anorectal and perianal regions. Analysis of 42 cases. Dis Colon Rectum 1994;37:950-7.
[Google Scholar]
|
| 4. |
Sobrado CW, Mester N, Nadalin W, Nahas SC, Bocchini SF, Habr-Gama A. Radiation induced total regression of a highly recurrent giant perianal condyloma: Report of a case. Dis Colon Rectum 2000;43:257-60.
[Google Scholar]
|
| 5. |
Browder JF, Araujo OE, Myer NA, Flowers SP. The interferons and their use in condyloma acuminata. Ann Pharmacother 1992;26:42-5.
[Google Scholar]
|
Fulltext Views
3,347
PDF downloads
1,031





