Translate this page into:
Exfoliative dermatitis with leukemia cutis in a patient with chronic myeloid leukemia: A rare association
2 Department of Oncology, PSG Institute of Medical Science and Research, Peelamedu, Coimbatore - 641 004, India
Correspondence Address:
Reena Rai
Department of Dermatology, PSG Institute of Medical Science and Research, Peelamedu, Coimbatore - 641 004
India
| How to cite this article: Raj A, Rai R, Rangarajan B. Exfoliative dermatitis with leukemia cutis in a patient with chronic myeloid leukemia: A rare association. Indian J Dermatol Venereol Leprol 2011;77:208-210 |
Sir,
A 75-year-old male presented with exfoliative dermatitis in November 2008. During admission, all routine blood investigations were normal expect for the raised white blood cell (WBC) count (32.1 Χ 10 3 /UL) and platelet count (613 Χ 10 3 /UL). Peripheral smear showed normochromic normocytic blood picture with neutrophilic leukocytosis and thrombocytosis. Skin biopsy revealed features suggestive of chronic superficial dermatitis. The patient improved with emollients and was discharged and advised to repeat WBC and platelet count after a month and the patient was lost to follow-up.
The patient presented in October 2009 with another episode of exfoliative dermatitis. His investigations were normal except for the raised WBC count (80.1 Χ 10 3 /UL) and platelet count (61.1 Χ 10 3 /UL) and hemoglobin was 9.8 g/dL. Peripheral smear showed marked leukocytosis with anemia with a shift to left, up to the myeloblast stage. A diagnosis of chronic myeloid leukemia (CML) was made. Bone marrow trephine biopsy showed total count increased in number, neutrophils 40%, band forms 17%, metamyelocytes 08%, myelocytes 11%, promyelocytes 08%, and myeloblasts 03%. His liver and renal function tests were normal. Diagnosis of CML was confirmed with immunophenotyping, where polymerase chain reaction (PCR) was found to be positive for BCR-ABL gene. Ultrasound abdomen showed splenomegaly. Biopsy of the skin revealed features suggestive of chronic superficial dermatitis.
Fifteen days later, the patient developed multiple tender erythematous ulcerative nodules over both lower limbs [1],[2] [Figure - 1]. Biopsy of the nodule showed angiocentric and diffuse dermal infiltration by atypical myeloid cells of neutrophilic series, suggestive of leukemic infiltrates in the skin [Figure - 2]. So, a diagnosis of luekemia cutis was made. The patient was administered Tablet Imatinib 600 mg/day by the oncologist and a month later there was complete resolution of lesions [Figure - 3].
 |
| Figure 1: Leukemia cutis |
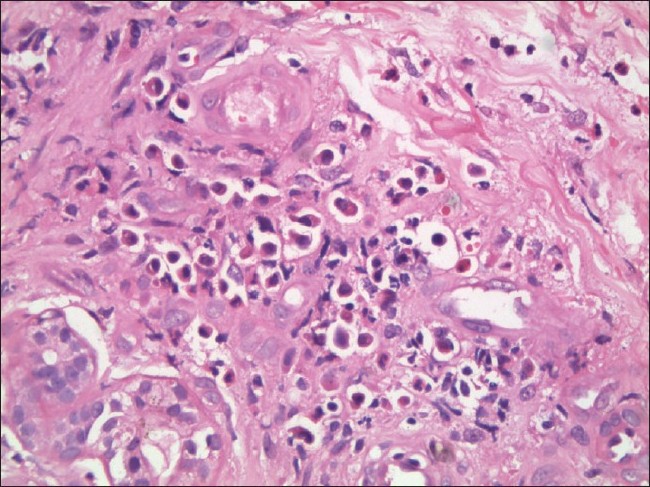 |
| Figure 2: Angiocentric and diffuse dermal infiltration by atypical myeloid cells of neutrophilic series, suggestive of leukemic infiltrates in the skin (H and E, �400) |
 |
| Figure 3: One month of therapy |
Exfoliative erythroderma manifests as erythema and scaling of the body, affecting more than 90% of the skin surface. Apart from skin disorders, it is most commonly associated with adult T cell lymphoma, leukemias and myelodysplasias. [3] Erythroderma with leukemia cutis in patients with CML is not reported.
Leukemia cutis is an uncommon cutaneous eruption coexistent with leukemia. . Adult T cell leukemia/lymphoma is the commonest cause for leukemia cutis seen in 40-60%, followed by AML (13%). [4],[5],[6] Although specific skin eruptions like leukemia cutis are seen in acute myelomonocytic leukemia and acute monocytic leukemia, [7,8] leukemic cells in the skin are rare in CML with an incidence of 2-8%. [9],[10]
The prognosis of leukemia cutis is inconsistent. The prognosis is even poorer after the skin infiltration has occurred. Tumorous infiltration into skin accompanied by blast crisis of CML has a poor prognosis. [6],[9] However, skin infiltration of leukemia cutis responded well to chemotherapy with Imatinib in our patient, with complete resolution within 3 months of therapy.
| 1. |
Cho -Vega JH, Mederios LJ, Prieto VG, Vega F. Leukemia Cutis. Am J Clin Pathol 2008;129:130-42.
[Google Scholar]
|
| 2. |
Beynet D, Oro AE. Leukemia Cutis presenting as a Sister Mary Joseph nodule. Arch Dermatol 2004;140:1170-1.
[Google Scholar]
|
| 3. |
Freedberg IM. Exfoliative dermatitis. In: Fitzpatrick TB, Eisen AZ, Wolff K, Freedberg IM, Austen KF, editors. Dermatology in General Medicine. 5 th ed. New York: McGraw Hill; 1999. p. 534-7.
[Google Scholar]
|
| 4. |
Agis H, Weltermann A, Fonatsch C, Haas O, Mitterbauer G, Mullauer L, et al. A Comparative study on demographic, hematological, and cytogenetic findings and prognosis in acute myeloid leukemia with and without leukemia cutis. Ann Hematol 2002;8:90-5.
[Google Scholar]
|
| 5. |
Desch JK, Smoller BR. The spectrum of cutaneous diseases in luekemias. J Cutan Pathol 1993;20:407-10.
[Google Scholar]
|
| 6. |
Ansell JE, Bhawan J, Pechet L. Luekemia Cutis in blast transformation of chronic myelocytic leukemia; Tdt positive blasts and response to vincristine and prednisone. J Cutan Pathol 1980;7:302-9.
[Google Scholar]
|
| 7. |
Kaddu S, Zenahlik P, Beham - Schmid C, Kerl H, Cerroni L. Specific Cutaneous infiltrates in patients with myelogenous leukemia: A clinicopathologic study of 26 patients with assessment of diagnostic criteria. J Am Acad Dermatd 1999;40:966-78.
[Google Scholar]
|
| 8. |
Yazawa H, Saga K, Omori F, Jimbow K, Sasagawa Y. The chilblain-like eruption as a diagnostic clue to the blast crisis of chronic myelocytic leukemia. J Am Acad Dermatol 2004;50:42-4.
[Google Scholar]
|
| 9. |
Su WP, Buechner SA, Li CY. Clinicopathologic correlation in Leukemia Cutis. J Am Acad Dermatol 1984;11:121-9.
[Google Scholar]
|
| 10. |
Buecher SA, Li CY, SuWP. Leukemia Cutis; A histopathologic study of 42 cases. Am J Dermatopathol 1985;7:109-19.
[Google Scholar]
|
Fulltext Views
2,887
PDF downloads
2,354





