Translate this page into:
Exacerbation reaction (Hypersensitivity) in Post-kala-azar dermal leishmaniasis with Miltefosine
Correspondence Address:
Sheena Bansal
Department of Dermatology, 4th Floor, College Building, Lokmanya Tilak Municipal Medical College and General Hospital, Sion, Mumbai - 400 022
India
| How to cite this article: Bansal S, Ghate SS, Jerajani H. Exacerbation reaction (Hypersensitivity) in Post-kala-azar dermal leishmaniasis with Miltefosine. Indian J Dermatol Venereol Leprol 2011;77:214-217 |
Sir,
The hypersensitivity and inflammatory reactions after initiation of treatment are known to occur in various diseases like syphilis (and rarely in leptospirosis and Lyme disease) [1],[2] and lepromatous leprosy, known as Jarisch-Herxheimer (J-H) reaction and Type 1 lepra reaction respectively. While J-H reaction occurs within few minutes of treatment with penicillin, Type 1 lepra reaction can occur within six months of treatment with multi-drug therapy.
We, hereby, report the case of a 20-year-old patient hailing from Patna, Bihar who presented with asymptomatic light coloured lesions all over body since 10 years and red nodules over trunk, face and extremities since two years. He also gave history suggestive of visceral leishmaniasis (VL) at the age of eight years. The intervening period was completely symptom free. Clinical examination revealed hypopigmented coalescing macules and erythematous nodules and plaques over face, trunk and extremities [[Figure - 1]a and b]. On investigation, the hematological parameters were as follows: hemoglobin: 11 g/dl, complete blood count (CBC): 9700/cumm, differential leukocyte count (DLC) (neutrophils: 67%, lymphocytes: 26%, eosinophils: 2%) and monocytes: 3%, platelet count: 1,46,000/cumm, erythrocyte sedimentation rate (ESR): 15 mm at end of 1 h. Liver function tests showed serum bilirubin: 0.6 mg/dl, SGOT: 45 IU/l and SGPT: 55 IU/l. Renal profile showed serum creatinine to be 0.9 mg/dl. The slit skin smears for Leishman-Donovan (LD) bodies were negative and the tissue culture on Novy-MacNeal-Nicolle (NNN) medium did not grow Leishmania donovani. The histopathology from a nodule showed diffuse dermal infiltration with lymphocytes, plasma cells and dermal macrophages [[Figure - 2]a] containing the organisms [[Figure - 2]b]. Giemsa stain showed histiocytes with intracellular reddish purple granules suggestive of LD bodies leading to a final diagnosis of post-kala-azar dermal leishmaniasis (PKDL). Owing to the reports of high resistance (as high as 60%) to conventional therapy of VL with sodium stibogluconate in endemic region in Bihar, [3] India, we decided to treat the patient with tablet miltefosine 50 mg twice a day for a period of three months, in accordance to the previous reports. [4],[5]
 |
| Figure 1: (a)Erythematous plaques on the forearm in a case of post-kala-azar dermal leishmaniasis Figure 1b: Hypopigmented patches, erythematous nodules on the back in the same patient |
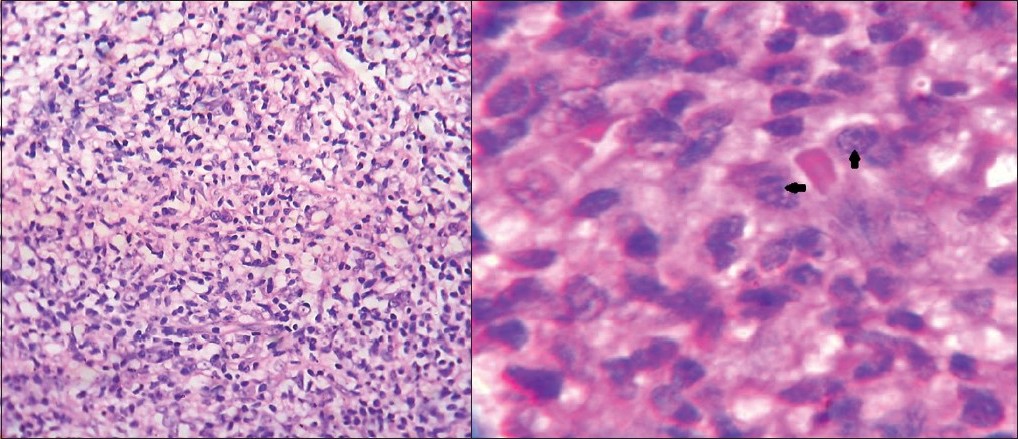 |
| Figure 2: (a)Biopsy from the plaque showing dense lymphohistiocytic infiltrate in the dermis (H and E, ×400) Figure 2b: Dermal macrophages containing Leishman– donovan bodies (Giemsa stain, ×1000) |
We noted a flare up in form of increased erythema and edema of nodules and evidence of necrosis over few plaques after 15 days of initiating miltefosine therapy with no change in hypopigmented macules [[Figure - 3]a and b]. Patient refused the biopsy this time and since he was completely asymptomatic and no systemic involvement was noticed with not much changes in hematological parameters except rise in CBC to 11,200/cumm, DLC (neutrophils: 70%, lymphocytes: 28%, eosinophils: 2%) and rise in ESR to 25 mm during the reaction period, the treatment was continued without any additional treatment. Patient was kept under strict supervision. One week later, the erythema and edema started subsiding and after two weeks erythema disappeared completely leaving behind hyperpigmentation [[Figure - 4]a and b].At the end of three months, all the erythematous nodules subsided leaving behind hyperpigmentation. Meanwhile, we came across two more cases of PKDL, natives of Bihar, who were again treated with tab miltefosine in the same dosages. This time also, we noticed increased erythema and edema of pre-existing nodules after 20 days of initiation of treatment in the patient presenting with erythematous nodules which resolved over a period of two weeks while the treatment was continued. While the other patient who presented with scaly plaques over face, did not report any exacerbation during the treatment.
 |
| Figure 3: (a)Increased erythema and evidence of necrosis over the plaque in the same patient after 15 days of initiation of miltefosine treatment Figure 3b: Increase in erythema in the plaques with no change in hypopigmented patches after 15 days of initiation of therapy |
 |
| Figure 4: (a)Post inflammatory hyperpigmentation in the same patient after one month of therapy Figure 4b: Post inflammatory hyperpigmented patches and persistent hypopigmented patches over back after completion of therapy |
Miltefosine, a novel drug used in the treatment of leishmaniasis, is an alkylphosphocholine and a membrane-active synthetic ether-lipid analogue which was originally developed for the treatment of cutaneous metastasis from mammary carcinomas. It has been proved to be an effective treatment for human visceral leishmaniasis. The leishmaniacidal activities of miltefosine have been associated with perturbation of the alkyl-phospholipid metabolism and the biosynthesis of alkyl-anchored glycolipids and glycoproteins. It brings about apoptosis-like death in all the forms of Leishmania parasite. Apoptosis greatly affects the host-parasite relationship, since strict control of the population of the parasite is required for the survival of the parasite inside the vector as well as in the macrophage. [6] It causes frequent but mild gastrointestinal side effects such as vomiting and diarrhea which do not require the discontinuation of therapy. Rarely, it may also cause increase in serum aspartate aminotransferase and serum creatinine. [7]
The exacerbation reaction in PKDL or VL has not been reported with miltefosine so far, not even with the conventional treatments like sodium stibogluconate and amphotericin B. The exacerbation in our two cases was noticed only in the nodules while the patches remained free of reaction suggesting hypersensitivity reaction in nodules due to probably increased load of organisms. Thus, we like to hypothesize that some hypersensitivity reactions are occurring in patients with PKDL after treatment with miltefosine, but this needs to be validated by studies with larger number of subjects and also the immunological basis of the same needs to be investigated. Thus, this is a call to dermatologists and physicians in the regions endemic for the disease to carry out such studies and report the incidence of such reactions, if noticed.
| 1. |
Vaughan C, Cronin CC, Walsh EK, Whelton M. The Jarisch-Herxheimer reaction in leptospirosis. Postgrad Med J 1994;70:118-21.
[Google Scholar]
|
| 2. |
Maloy AL, Black RD, Segurola RJ Jr. Lyme disease complicated by the Jarisch-Herxheimer reaction. J Emerg Med 1998;16:437-8.
[Google Scholar]
|
| 3. |
Croft SL, Sundar S, Fairlamb AH. Drug resistance in Leishmaniasis. Clin Microbiol Rev 2006;19:111-26.
[Google Scholar]
|
| 4. |
Sundar S, Kumar K, Chakravarty J, Agrawal D, Agrawal S, Chhabra A, et al. Cure of antimony-unresponsive Indian post-kala-azar dermal leishmaniasis with oral miltefosine. Trans R Soc Trop Med Hyg 2006;100:698-700.
[Google Scholar]
|
| 5. |
Ramesh V, Ansari NA, Jain RK, Salotra P. Oral miltefosine in the treatment of post-kala-azar dermal leishmaniasis. Clin Exp Dermatol 2008;33:103-5.
[Google Scholar]
|
| 6. |
Verma NK, Dey CS. Possible mechanism of miltefosine-mediated death of leishmania donovani. Antimicrob Agents Chemother 2004;48:3010-15.
[Google Scholar]
|
| 7. |
Jha TK, Sundar S, Thakur CP, Bachmann P, Karbwang J, Fischer C, et al. Miltefosine, an oral agent, for the treatment of indian visceral leishmaniasis. New Engl J Med 1999;341:1795-800.
[Google Scholar]
|
Fulltext Views
3,244
PDF downloads
2,410





