Translate this page into:
Primary cutaneous CD30+ lymphoproliferative disorder in an atopic dermatitis patient on cyclosporine therapy
2 Department of Dermatology, Asahikawa Medical College, Asahikawa, Japan
3 Department of Dermatology, Asahikawa Kousei Hospital, Asahikawa, Japan
Correspondence Address:
S Nakamura
Department of Dermatology, Asahikawa Medical College, Midorigaoka Higashi 2-1-1-1, Asahikawa, 078-8501, Hokkaido
Japan
| How to cite this article: Nakamura S, Takeda K, Hashimoto Y, Mizumoto T, Ishida-Yamamoto A, Iizuka H. Primary cutaneous CD30+ lymphoproliferative disorder in an atopic dermatitis patient on cyclosporine therapy. Indian J Dermatol Venereol Leprol 2011;77:253 |
Sir,
The risk of lymphoma in atopic dermatitis (AD) is controversial, and both positive and negative correlation has been reported. The relation may rather be related to its therapy. Additionally, increment of middle-aged AD might be related. The age of 9.6% of AD in Japan was over 46 years. Recently, beneficial effect of cyclosporine for AD has been established. However, after using cyclosporine for AD, primary cutaneous CD30+ lymphoproliferative disorder (including lymphomatoid papulosis (LyP), primary cutaneous anaplastic large cell lymphoma (ALCL), and borderline lesion) is sporadically observed. [1],[2],[3],[4] Recent report indicated that CD30+ T lymphocytes are up-regulated in the lesional skin of AD by mast cells which show the regulatory roles on both innate and acquired immunities. [5]
A 57-years-old man was treated by topical corticosteroid ointment and antihistamine by a local dermatologist because of itchy chronic eruptions under a diagnosis of AD for about 20 years. He had no methotrexate administration or PUVA therapy. It was not clear whether he received steroid administration treatment. Because of the lack of response, he was referred to our hospital [[Figure - 1]a]. Total body analyses including CT and Ga scintigraphy did not disclose any systemic manifestations including mycosis fungoides or cutaneous lymphoma. Histopathology of the skin lesion was consistent with AD [[Figure - 1]b and c].
 |
| Figure 1: (a) Lichenified, scaly, erythematous plaques on the back. (b) Histopathological findings. (H and E, �100). Inflammatory infiltrate is observed on the upper dermis. Hyperkeratosis, acanthosis, and parakeratosis. Epidermal spongiosis and lymphoid cell infiltration. (c) CD30+ lymphocytes were scarce |
We started pre-prandial administration of cyclosporine (150 mg/twice a day; 2.2 mg/kg/day). The concentration of trough level was 65 ng/ml. The maximum concentration of cyclosporine was got at 1 h and showed 770 ng/ml. Atopic erythema and itching were decreased dramatically. After eight weeks of treatment, exudative erythematous plaque was detected on his right thigh [[Figure - 2]a]. Topical application of betamethasone 17-valerate ointment was not effective and peripheral reddish nodules were developed. Cyclosporine was discontinued and skin biopsy was performed for the tumor [[Figure - 2]b]. Superficial lymph nodes were not palpable. Skin biopsy disclosed dense lymphoid cell infiltrate in the upper dermis [[Figure - 3]a] and anaplastic large cells with bizarre morphology [[Figure - 3]b]. The anaplastic cells were CD3+ and CD30+ [[Figure - 3]c].Anaplastic lymphoma kinase (ALK) 1 protein and EB virus were negative. T cell receptors gene rearrangement of the skin nodule was negative. CT, Ga scintigraphy, MRI, PET-CT, bone marrow aspiration, gastric and colon endoscopies did not detect any systemic manifestations. Peripheral blood analyses disclosed no abnormality, either. Liver function tests, BUN and serum creatinine levels were also normal. Serum soluble interleukin-2 receptor and thymidine kinase activity were 294 U/ml (normal:149-519 U/ml), and 4.8 U/l (<5 U/ml), respectively. Serum IgE was 37.1 IU/ml (0-170I U/ml). Thymus and activation-regulated chemokine (TARC; chemokine of Th2) was 1,455 pg/ml (<450 pg/ml). We diagnosed this case as a CD30+ lymphoproliferative disorder (Type A LyP) by those histological examinations, laboratory examinations, and clinical features. Skin nodules subsided spontaneously without any specific treatment. His AD has been favorably treated by corticosteroid ointment, skin emollients and antihistamine administration.
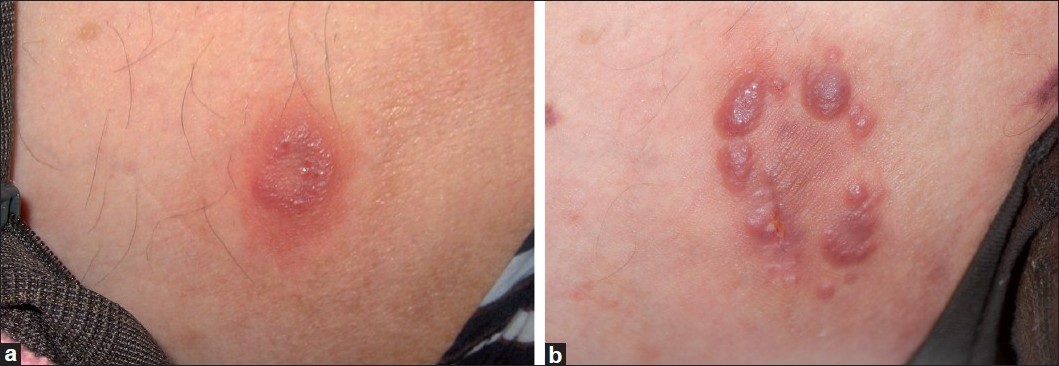 |
| Figure 2: Clinical presentations on the right thigh. (a) Exudative erythematous plaque was detected. (b) The nodules were still enlarging following the discontinuation of cyclosporine |
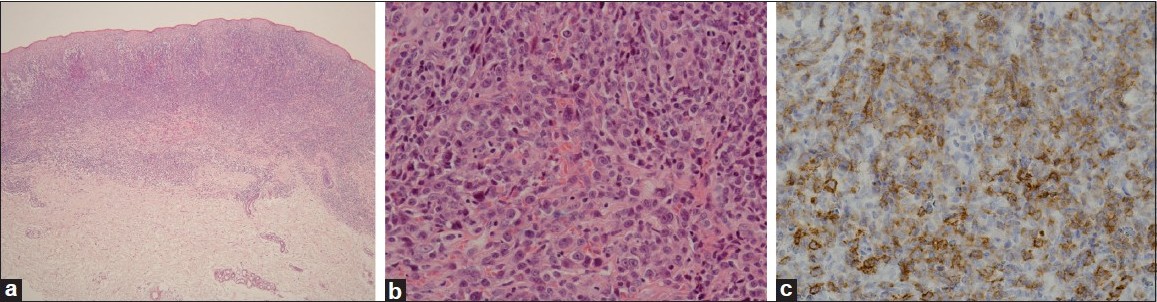 |
| Figure 3: Histopathological findings. (a) Low magnification (�20). Numerous mononuclear cell infiltrates are noted in the upper dermis. (b) Bizarre-shaped cells with conspicuous nucleolus (�200). (c) Most of the infiltrated cells were CD30+ (�200) |
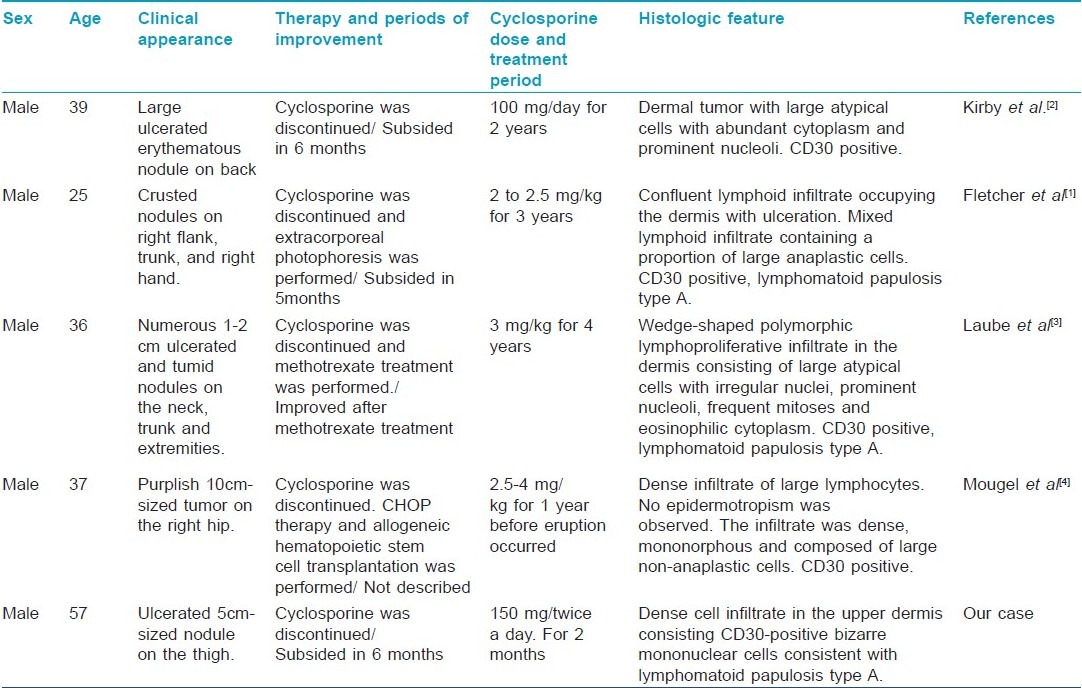
CD30+ lymphoproliferative disorder in AD patients during cyclosporine therapy is rare and only four cases have been described [Table - 1]. [1],[2],[3],[4] Cyclosporine is also used for psoriasis, which is accompanied by similar lymphoproliferative disorder. While some reports suggest no significant relation between AD and lymphoma, others suggest the positive correlation between cutaneous lymphoproliferative disorder and AD. [1] As shown in [Table - 1], CD30+ lymphoproliferative disorder in AD patients treated by cyclosporine, three of the five reported cases showed the LyP type histopathology and four of the five cases showed resolution of the lesion without progression to genuine lymphoma.
Recent reports indicate that CD30+ T lymphocytes are up regulated in the lesional skin of AD. This is induced by interleukin-8, macrophage inflammatory protein (MIP)-1α, and MIP-1β derived from mast cells. This novel activation pathway does not depend on the classical IgE pathway and this pathway may be observed in psoriasis as well as in Hodgkin lymphoma. [5] Mast cells may have a regulatory role on both innate and acquired immunity. [5] In our case, numerous CD30+ T lymphocytes were detected in skin tumors after cyclosporine administration, which was not apparent in the pre-existing AD lesion. We could not get the samples and not detect the change in the number of mast cells or cytokines derived from mast cells of the skin during the tumor progression and regression in this case. Cyclosporine, besides its well-known immunosuppressive effect, might have changed the cytokine balance including mast cell-derived cytokines.
Our case indicates the potential risk of cutaneous CD30+ lymphoproliferative disorder in cyclosporine-treated AD. Cyclosporine-induced lymphoproliferative disorder, albeit rare, should be kept in mind during the cyclosporine treatment of AD.
| 1. |
Fletcher CL, Orchard GE, Hubbard V, Whittaker SJ, Edelson RL, Russel-Jones R. CD30+ cutaneous lymphoma in association with atopic eczema. Arch Dermatol 2004;140:449-54.
[Google Scholar]
|
| 2. |
Kirby B, Owen CM, Blewitt RW, Yates VM. Cutaneous T-cell lymphoma developing in a patient on cyclosporin therapy. J Am Acad Dermatol 2002;47:S165-7.
[Google Scholar]
|
| 3. |
Laube S, Stephens M, Smith AG, Whittaker SJ, Tan BB. Lymphomatoid papulosis in a patient with atopic eczema on long-term cyclosporine therapy. Br J Dermatol 2005;152:1346-8.
[Google Scholar]
|
| 4. |
Mougel F, Dalle S, Balme B, Houot R Thomas L. Aggressive CD30 large cell lymphoma after cyclosporine given for putative atopic dermatitis. Dermatology 2006;213:239-41.
[Google Scholar]
|
| 5. |
Fischer M, Harvima IT, Carvalho RF, Moller C, Naukkarinen A, Enblad G, et al. Mast cell CD30 ligand is upregulated in cutaneous inflammation and mediates degranulation-independent chemokine secretion. J Clin Investig 2006;116:2748-56.
[Google Scholar]
|
Fulltext Views
2,353
PDF downloads
2,662





