Translate this page into:
Paraneoplastic multicentric reticulohistiocytosis: A clinicopathologic challenge
2 Department of Dermatology, St. John's Medical College and Hospital, Bangalore - 560 034, India
3 Department of Medical Oncology, St. John's Medical College and Hospital, Bangalore - 560 034, India
4 Department of Clinical Pathology, St. John's Medical College and Hospital, Bangalore - 560 034, India
Correspondence Address:
Rajalakshmi Tirumalae
Department of Pathology, St. John's Medical College, Bangalore-560 034
India
| How to cite this article: Tirumalae R, Rout P, Jayaseelan E, Shet A, Devi S, Kumar KR. Paraneoplastic multicentric reticulohistiocytosis: A clinicopathologic challenge. Indian J Dermatol Venereol Leprol 2011;77:318-320 |
Abstract
Multicentric Reticulohistiocytosis (MRH) is a rare, systemic non-Langerhans cell histiocytosis (non-LCH) with prominent joint and skin manifestations. It is mostly self limiting. However, 15-30% of the cases are associated with malignancy and carry a poor prognosis. We report the case of a 42-year-old man who presented with multiple reddish-brown papules that on biopsy showed aggregates of oncocytic histiocytes with several multinucleate giant cells. Immunostains were positive for CD 68, CD 45 and were negative for S-100, CD1a. An impression of multicentric reticulohistiocytosis (MRH) was made, with the recommendation to screen for malignancy. Electron microscopy of the skin lesions showed features consistent with non-Langerhans cell histiocytosis. The patient was later diagnosed with acute myeloid leukemia at a follow-up visit several months later. Thus, it appears prudent to screen and follow-up adults with MRH, to identify an underlying malignant condition.Introduction
Multicentric reticulohistiocytosis (MRH) is an uncommon disorder with prominent articular and cutaneous manifestations. [1] The disease generally presents in association with a range of infections and autoimmune disorders, and can rarely precede detection of certain malignancies. [2] It may be the presenting feature of an undetected malignancy i.e. a paraneoplastic syndrome. We describe the case of a 42-year-old gentleman who was diagnosed with MRH. Biopsy of the cutaneous lesions in this patient revealed CD 45-positive cells that were also positive for CD 68, in association with a hematologic malignancy. The clinical and pathological findings of this case are presented here and the literature pertaining to MRH has been reviewed.
Case Report
A 42-year-old man presented with low backache and weakness associated with intermittent, low-grade fever of six-months duration. The patient had also noticed skin lesions over his arms, trunk, and back that were present longer than six months. Physical examination was significant for the presence of pallor and moderate splenomegaly. The other systems were unremarkable. The skin of the abdomen and the trunk had multiple red-brown papules and nodules ranging in size from 0.3 - 0.6 cm, which were nonpruritic [Figure - 1].
 |
| Figure 1: Multiple reddish-brown papules and nodules over the trunk. Inset shows one papule with an erythematous base |
Pertinent laboratory findings on admission revealed pancytopenia with hemoglobin of 4.3 gm / dl, a total white cell count of 3000 / cu mm, and thrombocytopenia 90,000 cells per cu mm. Examination of the peripheral blood revealed a leucoerythroblastic blood picture, with occasional atypical cells. A bone marrow aspirate revealed a dry tap. The marrow biopsy revealed a few large atypical cells and extensive fibrosis.
A skin biopsy revealed nodular aggregates of histiocytes in the upper and mid-dermis with several multinucleate giant cells. These histiocytes had a deep pink / oncocytic cytoplasm and vesicular nuclei [Figure - 2]. The histiocytes were accompanied by scattered lymphocytes, but were remarkable for the absence of eosinophils. There were no foam cells / nuclear grooves. Immunostains of these lesions revealed that these cells were positive for CD 68, CD 45 and negative for S-100, CD1a and pancytokeratin. There was a low MIB-1 proliferation index. With these findings, a diagnosis of non-Langerhans cell histiocytosis, possibly multicentric reticulohistiocytosis was made. Screening for malignancy was recommended. Electron microscopy of the skin lesions confirmed the histiocytic nature of these cells and there were no Birbeck granules identified. Additionally, there was pleomorphic, electron-dense material within the cells, with concentric lamellae and myelin figures, consistent with non-Langerhans cell histiocytosis [Figure - 3].
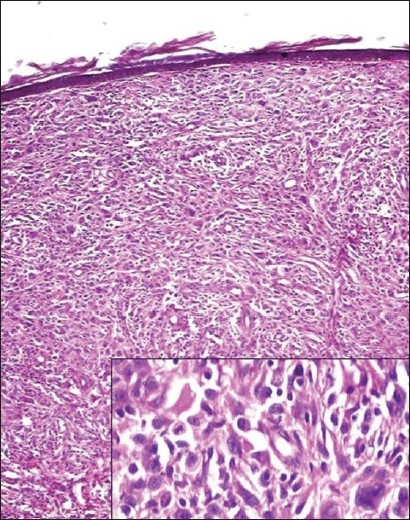 |
| Figure 2: Nodular aggregates of histiocytes in the upper and mid-dermis with several multinucleate giant cells (H and E, ×200). Inset shows histiocytes with an oncocytic cytoplasm (H and E, ×400) |
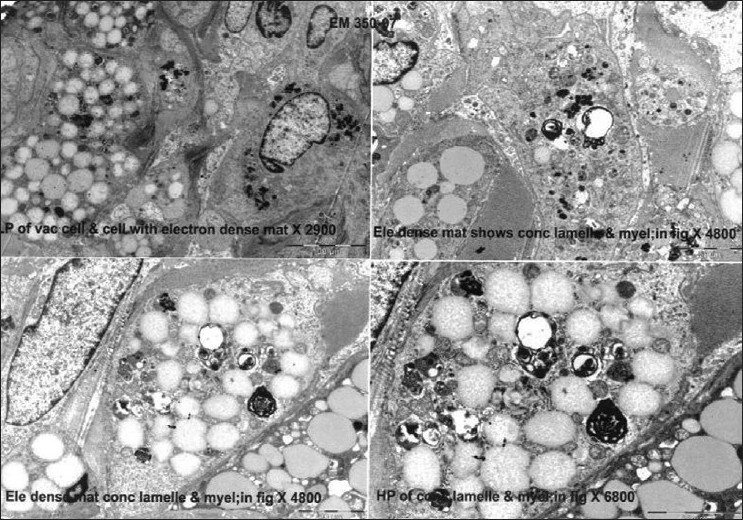 |
| Figure 3: Electron microscopy images showing cytoplasmic vacuoles, electron-dense material, and myelin figures within the histiocytes. Birbeck granules are absent |
Meanwhile, the patient sought treatment at another hospital and returned to us after three months, when it was noted that the skin lesions persisted. Peripheral blood smears at this point revealed 23% myeloblasts. A repeat bone marrow aspirate and flow cytometry confirmed the diagnosis of acute myeloid leukemia (positive for CD 13, CD 33, and CD 34). We went back to the skin biopsy and performed immunostains for myeloperoxidase (MPO), which was negative.
Discussion
Multicentric reticulohistiocytosis is a rare, multisystem histiocytic disorder, typically characterized by chronic, destructive, disfiguring polyarthritis and cutaneous nodules. [1],[2] It is more common in adults, with a female predilection. Visceral involvement is also documented. [3] Most of these lesions resolve spontaneously over years, but leave behind mutilated joints, if not recognized early.
What makes this disease intriguing is its association with autoimmune diseases, and particularly, malignancies. [2] Up to 31% of MRH in adults may be malignancy-associated. [4] Most often, they are concurrent with the diagnosis of malignancy, but they may precede the detection of the malignancy. [5] The list includes breast, gynecologic, colonic, and hematologic malignancies. [2],[6],[7] The largest reported series of malignancy-associated MRH consists of four cases. [4] In such instances, one can anticipate atypical clinical presentations such as the absence of joint involvement, as seen in our patient.
Multicentric reticulohistiocytosis is diagnosed on the basis of skin or synovial biopsies. [1] The finding of aggregates of oncocytic histiocytes with a ground-glass cytoplasm is typical. [4],[5] Immunoreactivity for histiocytic lineage markers such as CD 68, Ki-MP is seen. They lack CD1a and S100 expression, thus distinguishing them from langerhans cell histiocytosis (LCH). [4] Electron microscopy shows electron-dense pleomorphic cytoplasmic inclusions in 5 - 40% of the cases. [8] This was appreciated in our case.
The differential diagnoses to be considered on biopsy include reticulohistiocytoma, xanthogranuloma, malignant histiocytosis, and a specific infiltrate such as leukemia. [5] Reticulohistiocytoma is usually a solitary lesion, but can have a similar histology. They express factor XIIIa, which is lacking in most cases of MRH, and may serve as a distinguishing feature. [9] This is not universal and one has to then rely on clinical correlation. Malignant histiocytosis displays obvious cytological atypia and a high mitotic rate, which is clearly absent in the current biopsy. We have also performed a MIB1 count, which is low. It is always prudent to rule out a leukemic infiltrate, as some of them may share a histiocytic morphology. [10] This is accomplished by immunostains for myeloperoxidase, which is negative in our case. The putative cell of origin is said to be related to the dermal dendrocyte, driven into proliferation by a cocktail of cytokines such as TNF alpha and Interleukins. [5]
This case taught us some valuable lessons. All non-LCH are not necessarily innocuous. A diagnosis of MRH in adults should trigger caution. These patients must be screened for malignancy and followed up closely. Selective use of immunostains is essential to exclude other mimics. It is important to be aware of this entity and its atypical presentation, as the prognosis is entirely dependent on the underlying pathology.
Acknowledgments
The authors express their gratitude to Dr. Gayathri R and Dr. Shankar SK, Department of Neuropathology, NIMHANS, Bangalore for the electron microscopy and Dr. Almut Boer, Dermatologikum, Hamburg for some of the immunostains.
| 1. |
Gorman JD, Danning C, Schumacher HR, Klippel JH, Davis JC Jr. Multicentric Reticulohistiocytosis Case Report with immunohistochemical analysis and literature review. Arthritis Rheum 2000;43:930-8.
[Google Scholar]
|
| 2. |
Baghestani S, Khosravi F, Dehghani Zahedani M, Mahboobi A. Multicentric reticulohistiocytosis presenting with papulonodular skin eruption and polyarthritis. Eur J Dermatol 2005;15:196-200.
[Google Scholar]
|
| 3. |
Barrow MV, Holubar K. Multicentric reticulohistiocytosis. A review of 33 patients. Medicine 1969;48:287-305.
[Google Scholar]
|
| 4. |
Snow JL, Muller SA. Malignancy associated Multicentric Reticulohistiocytosis: A clinical, histological and immunophenotypic study. Br J Dermatol 1995;13:71-6.
[Google Scholar]
|
| 5. |
Zelger BW, Sidoroff A, Orchard G, Cerio R. Non-Langerhans cell histiocytoses. A new unifying concept. Am J Dermatopathol 1996;18:490-504.
[Google Scholar]
|
| 6. |
Hinchman KF, Wu JJ, Soden CE Jr, Waldman J, Dyson SW. Multicentric reticulohistiocytosis associated with Burkitt lymphoma and adenocarcinoma. Cutis 2008;82:113-4.
[Google Scholar]
|
| 7. |
Kishikawa T, Miyashita T, Fujiwara E, Shimomura O, Yasuhi I, Niino D, et al. Multicentric reticulohistiocytosis associated with ovarian cancer. Mod Rheumatol 2007;17:422-5.
[Google Scholar]
|
| 8. |
Berti E, Zelger B, Caputo R. Reticulohistiocytosis in Pathology and genetics of skin tumours. In: LeBoit P, Burg G, Weedon D, Sarasin A, editors. Lyon: IARC Press; 2006. p. 224-5.
[Google Scholar]
|
| 9. |
Zelger B, Cerio R, Peter Soyer H, Misch K, Orchard G, Wilson-Jones E. Reticulohistiocytoma and Multicentric Reticulohistiocytosis. Am J Dermatopathol 1994;16:577-84.
[Google Scholar]
|
| 10. |
Pande S, Werner B, Boer A. Leukemia cutis - clinicopathologic study of 34 patients. Dermatopathol Practical and Conceptual 2007. Available from: http://www.derm101.com . [Last accessed on 2010 June 1].
[Google Scholar]
|
Fulltext Views
3,209
PDF downloads
3,018





