Translate this page into:
Dermatoses in the first 72 h of life: A clinical and statistical survey
Correspondence Address:
Vanessa Zagne
Rua Cel Moreira Cesar 376/1302, Icara�, Niter�i, Rio de Janeiro, RJ
Brazil
| How to cite this article: Zagne V, Fernandes NC. Dermatoses in the first 72 h of life: A clinical and statistical survey. Indian J Dermatol Venereol Leprol 2011;77:470-476 |
Abstract
Background: The neonatal period is generally regarded as the first 28 days of extrauterine life. Skin disorders are commonly seen in the neonatal period, most of which are transient and limited to the first days or weeks of life. In spite of being so frequent, these transient conditions usually escape dermatologist's observations, and consequently few have been studied. Aims: The study was designed to identify the dermatoses in the first 72 h of life; to report the relationship among the most common dermatoses with the newborn's features; and to verify how often dermatoses are reported by the neonatologist. Methods: The authors carried out a cross-sectional study on newborn's dermatoses in a brazilian public hospital, including 203 healthy neonates, until 72 h of age, with skin disorders. Results: Out of 34 different skin diagnosed conditions, hypertrichosis lanuginosa, Mongolian spot, sebaceous hyperplasia, epidermal hyperpigmentation, erythema toxicum, and salmon patch were the most frequent ones. The dermatoses with statistical significance were: Mongolian spot and epidermal hyperpigmentation with the non-white newborns; erythema toxicum and cutis marmorata with the white newborns; salmon patch with the female sex; physiologic desquamation with the cesarean section; acrocyanosis with the first pregnancy birth and Bohn's nodules with the vaginal delivery. Conclusions: Thirty-four different types of dermatological alterations were identified in the healthy newborn within 3 days of life at the Maternity School of the Federal University of Rio de Janeiro. Underreporting of dermatoses with serious medical significance shows the importance of a dermatologist in the neonatal unit of a hospital.Introduction
The expression newborn baby (NB) defines babies who have just been born up to their 28 th day of extrauterine life (World Health Organization, 1948). [1],[2] The newborn skin can present with a vast range of conditions, from benign diseases to life-threatening ones. Dermatoses are quite frequent in this population, they are present from 96% [3] up to 99.3% [4] of all newborn babies, whenever an examination of the skin, oral mucosal membrane, genitals, and phaneros (hair and nails) is performed. [4],[5],[6] The newborn cutaneous alterations, as a general rule, involute more rapidly than those of adults. Therefore, many of the conditions regarded as severe are only transitory, and can even be the result of a physiologic action. [7],[8],[9] Not withstanding, it is important that even when transitory, these lesions are acknowledged so as not to cause worry, and so, receive the suitable treatment. [7] To make matters worse, they are hardly ever reported by neonatologists, and dermatologists demonstrate quite a low familiarity with them.
Therefore, the objectives of this study were: (i) to identify the dermatoses within the first 72 h of life; (ii) to report the relationship among the most common dermatoses of the newborn and mother′s features; and (iii) to verify how often the skin disorders are reported in the newborn′s file by the neonatologists.
Methods
A cross-sectional descriptive study by means of the dermatological examination on newborn babies (NBs) from 0 to 3 days of age, at the Rio de Janeiro Maternity School-UFRJ, excluding all those hospitalized in both, the Neonatal Intermediary Unit and the Neonatal Intensive Care Unit. A total of 203 newborn babies were submitted to the dermatological examination within the time span of 8 months (2004/2005). These examinations were performed by two dermatologists.
The dermatological examination was carried out once a week, in the morning, under natural sun light, including examination of the genitals, oral cavity, hair scalp, and nails. The variables analyzed were: mother and newborn (NB) skin color, number of pregnancies, type of birth delivery, and newborn sex. The skin color was classified in white and non-white, and the criteria were the color of the skin surface, the genitals and skin folds for the newborns; whereas for the mothers, it was only the skin surface color. Non-white included afro-descendants, oriental and Asian people, American Indians, and mestizos.
The diagnosis was based upon the clinical characteristics dispensing the performance of cutaneous biopsies.
The statistical analysis was performed by the Chi-square (χ2 ) test and the criteria of significance adopted were of level 5%. Only those more frequent dermatoses (over ten cases) were submitted to the statistical testing.
Results
A total of 203 newborn babies were included in the study. A total of 118 (58.1%) were white, and 85 (41.9%) non-white. A total of 105 (51.7%) were female, and 98 male (48.3%); 190 had been born weighing 2500 g or plus (93.6%), whereas 13 (6.4%) had been born weighing less than 2500 g. Only 13 (6.4%) were premature and one post-term (0.5%). A total of 110 (54.1%) were delivered vaginally, out of them three with the use of forceps; whereas 93 (45.8%) were delivered by cesarean section (48.5%). In the case of the mothers, 104 (51.1%) were white, and 98 non-white. A total of 114 (56.4%) were multiparae and 88 (43.6%) primiparae.
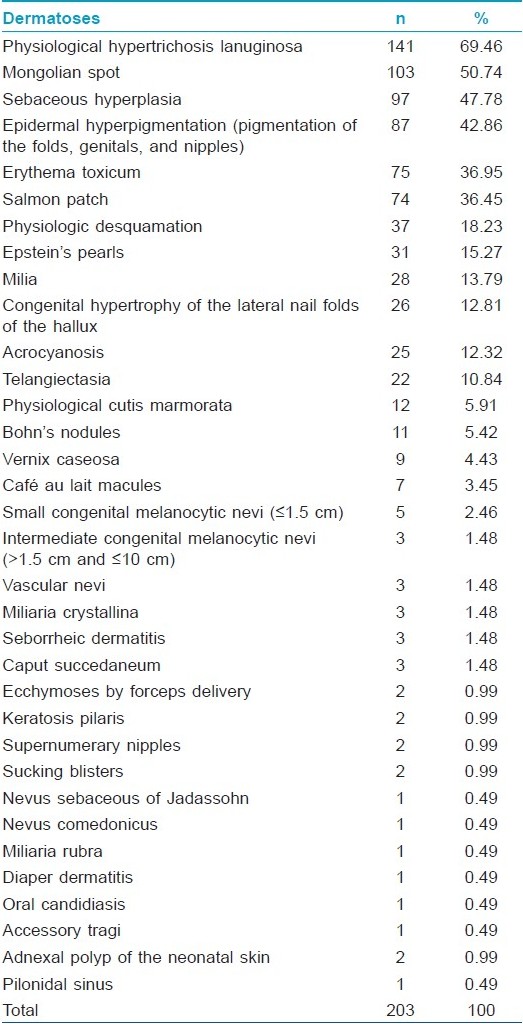
Altogether, 34 dermatological alterations were identified from all the 203 newborn babies included in the study [Table - 1]. Out of them, 106 newborn babies (86.7%) presented more than one dermatosis, nevertheless, the highest number of diagnosed dermatoses in one subject was only nine and the average was 3.9 [Figure - 1], [Figure - 2], [Figure - 3], [Figure - 4], [Figure - 5], [Figure - 6], [Figure - 7] and [Figure - 8].
 |
| Figure 1: Physiological hypertrichosis lanuginosa |
 |
| Figure 2: Mongolian spot |
 |
| Figure 3: Vernix caseosa and physiological epidermal hyperpigmentation of the folds |
 |
| Figure 4: Erythema toxicum |
 |
| Figure 5: Salmon patch |
 |
| Figure 6: Physiologic desquamation |
 |
| Figure 7: Bohn's nodules |
 |
| Figure 8: Adnexal polyp of the neonatal skin at the external area of the right nostril |
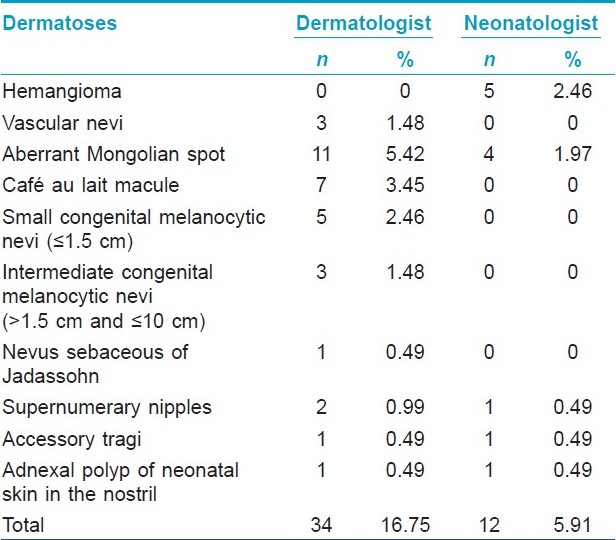
Out of the 203 subjects, 34 (16.75%) presented with serious medical significance according to the dermatologist and 12 (5.91%) according to the neonatologist, nevertheless, both agreed in seven diagnosis (20.58%) [Table - 2].
Discussions
In this study, we observed a lack of correlation between the mother′s and babie′s skin colors. The system of skin color inheritance, defined by Mendel as polygenic, is very complex. Brazil is a country marked by great interracial marriage, thus explaining why a black mother can have a white baby, if his father is white, or vice versa. Besides that, in general, all neonates are significantly lighter than adults and are able to reach adult levels of pigmentation by 6 months of age. [10]
The Mongolian spot was highly associated with the non-white skin color [Table - 3]. A greater incidence has been reported in non-white, [4],[11] black, and oriental babies. [12],[13],[14] As far as the localization areas are concerned, a greater incidence was on the nates and caudal lumbar regions, which is in conformity with the present medical literature. [12],[13],[14],[15],[16] Eleven newborn babies presented aberrant Mongolian spots on their knees, back, shoulders, dossa of the feet and hands, [16] face, and scalp. [17] In 8 out of 11 cases, the caudal lumbar region and/or natal regions also presented lesions. Among the subjects, only two were white babies. Multiple lesions have already been described, they are generally followed by lesions in the caudal lumbar region or natal region. [14]
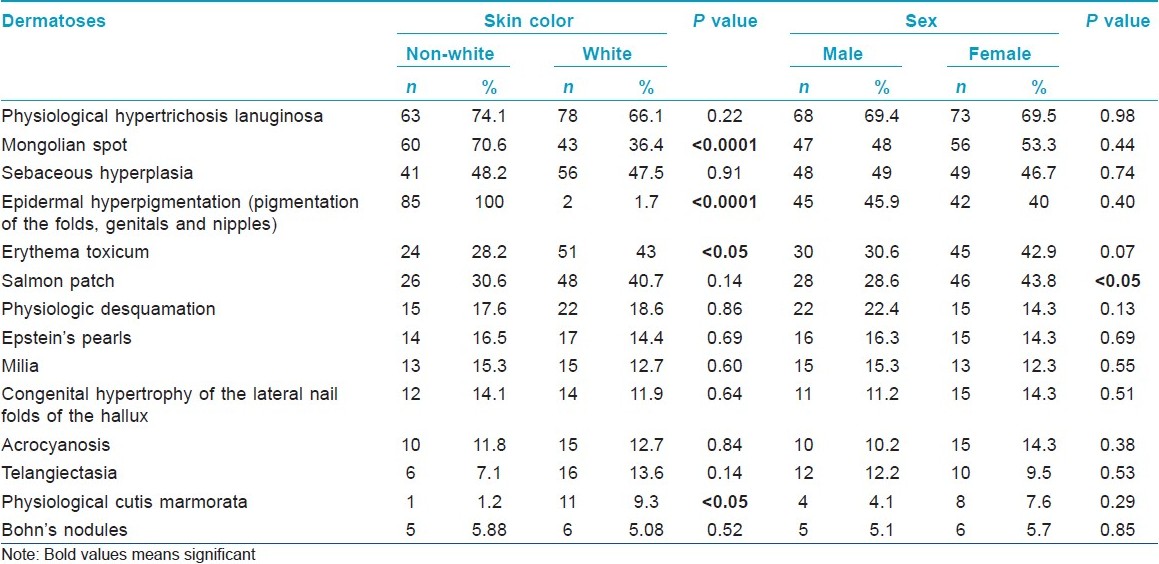
Physiologic desquamation was significantly higher among newborn babies who were delivered from cesarean sections [Table - 4]. There is only one observation in which type of birth and physiologic desquamation were correlated, however, among those newborn babies delivered vaginally. [18] The vernix caseosa sheds off within the first weeks of life. [19] The newborn babies who were born with greater amount of vernix likely to suffer from a major desquamation later on.

The presence of the acrocyanosis was significantly higher in newborn babies whose mothers were delivering for the first time [Table - 4]. Out of the 24 newborns who presented acrocyanosis, 16 were delivered vaginally. As these deliveries are usually harder and slower, we might consider that the pressure suffered by the fetus while still inside the uterus and the birth canal might explain the relationship, in which case, that has not yet been fully described.
The physiological cutis marmorata occurred a significantly amongst the white colored skin subjects [Table - 3]. It might be that case in which it is easier to observe this type of lesion on lighter-colored skin subjects. This association has not been described by other authors so far.
The Bohn′s nodule and the Epstein′s pearls are microkeratocysts, the first located on the palatal raphe and the second, on the alveolar ridges. [16] The available literature refers to the imprisonment of the epithelial cells in the place of fusion of the alveolar processes. [20] The Bohn′s nodule presented a significant association with the vaginal deliveries [Table - 4], yet, this association has not been reported.
A congenital flesh-colored, firm, pedunculated papule with a smooth surface has been observed at the external area on the right nostril, which was excised at the age of 2 years. A histopathologic examination showed the presence of vellus hair, stretched capillary, and nervous lemniscus, which is compatible with hamartoma. Despite being located on the nostril, presented a distinct evolution, as it did not detach spontaneously from the skin surface, after 1 week of life, like the adnexal polyp of the neonatal skin (APNS); it was morphologically and histologically similar to the APNS. There are previous descriptions, by the literature, of ectopic lesions located on lower eyelid, cheek, preauricular region, scapular region, axilla, arm, hypochondrium, scrotum and labia majora; [21] and of two non-ectopic cases (lesions on the breast) observed beyond the neonatal period (in a 53-day-old and in a 370-day-old infants). [22] By that, we chose to classify it as an ectopic adnexal polyp of the neonatal skin beyond the neonatal period, and we believe that the APNS should be considered one of the small tumors seen not only on the trunk, not only in neonates, but also in other sites and in infants and children. However further studies are necessary to confirm our hypothesis.
We considered dermatoses with serious medical significance, those with clinical relevance as they could be part of syndromes, be sign of extra-cutaneous diseases or cause complications depending on their location [8] [Table - 2]. We believe that those five lesions diagnosed by the neonatologist as hemangioma were actually salmon patches. Aberrant Mongolian lesions were described in association with inborn errors of metabolism, [23],[24],[25] cleft lip, [26] and cutis marmorata telangiectatica congenital. [27] Cafι au lait spots depending on their size or multiplicity can be related to the diagnosis of genetic diseases. [28] Congenital melanocytic nevi may be precursors of cutaneous melanoma. [9] Nevus sebaceous of Jadassohn has potential to develop a variety of benign and, less commonly, malignant neoplasms. Supernumerary nipples can be associated with nephrourinary malformations. [29] Accessory tragi can be part of syndromes involving the first branchial arch. [30] The polyp was located in the right nostril and could cause partial obstruction and aesthetical problems.
Underreporting of dermatoses with serious medical significance by a non-dermatologist has already been described. [31],[32] as the dermatologist has a more specific knowledge about cutaneous diseases [Table - 2].
This study enabled the characterization of the newborn babies dermatoses profile within a public institution. It is important that dermatologists are familiarized with it, so that they can recognize and treat it in the appropriate way. Neonatal dermatoses evaluation performed by both, the dermatologist and the neonatologist simultaneously, makes it possible for the achievement of a more accurate diagnosis. The neonatal unit dermatologist can make sure that a more detailed guidance is given to the mothers about physiological dermatoses that might come up in that period, sorting out doubts and excessive worries.
Acknowledgments
We wish to thank the Puericulture and Pediatrics Martagγo Gesteira Ethics Committee for the analysis and approval of the project.
We would like to thank Dr. Rita Guιrios Bornia, Head of the Medical Department of the Maternity School of the Federal University of Rio de Janeiro, for allowing us to carry out this research at the School Maternity.
We would also like to demonstrate our appreciation to the statisticians Mrs. Rosβngela Noι for the outstanding help in the outlining of the study, computerizing the data bank and in the analysis of the results and also for supervising the design and the final data analyses.
We want to show our gratitude to Dr. Geraldo Augusto Gomes, otolaryngologist, who carried out the excision of the ectopic adnexial polyp of the neonatal skin beyond the neonatal period and to Dr. Juan Piρeiro-Maceira for histopathological examination.
| 1. |
Orlandi OV, Sabrá A. O recém-nascido a termo. In: Rezende J, editor. Obstetrícia. 10 th ed. Rio de Janeiro: Guanabara Koogan SA; 2005. p. 380-6.
[Google Scholar]
|
| 2. |
Rezende J. Patologia do feto e do recém-nascido. In: Rezende J, editor. Obstetrícia. 9 th ed. Rio de Janeiro: Guanabara Koogan SA; 2002. p. 1366-77.
[Google Scholar]
|
| 3. |
Moosavi Z, Hosseini T. One year survey of cutaneous lesions in 1000 consecutive Iranian newborns. Pediatr Dermatol 2006;23:61-3.
[Google Scholar]
|
| 4. |
Rivers JK, Frederiksen PC, Dibdin C. A prevalence survey of dermatoses in the Australian neonate. J Am Acad Dermatol 1990;23:77-81.
[Google Scholar]
|
| 5. |
Pereira LB, Gontijo B, Silva CM. Dermatoses neonatais. An Bras Dermatol 2001;76:505-37.
[Google Scholar]
|
| 6. |
Pereira LB. Prevalência de dermatoses no recém-nascido: Estudo comparativo entre dois hospitais de Belo-Horizonte. Belo Horizonte: Universidade Federal de Minas Gerais; 1997.
[Google Scholar]
|
| 7. |
Wallach, D. Diagnosis of common, benign neonatal dermatoses. Clin Dermatol 2003;21:264-8.
[Google Scholar]
|
| 8. |
McLaughlin MR, O'Connor NR, Ham P. Newborn skin: Part II. Birthmarks. Am Fam Physician 2008;77:56-60.
[Google Scholar]
|
| 9. |
Magaña-Garcia M, González-Campos N. Lesiones cutáneas en un millar de recién nacidos. Estudio de casos y controles. Gac Méd Méx 1997;133:407-11.
[Google Scholar]
|
| 10. |
Post PW, Krauss AN, Walcman S, Auld PA. Skin reflectance of newborn infants from 25 to 44 weeks gestacional age. Hum Biol 1976;48:541-57.
[Google Scholar]
|
| 11. |
Jacobs AH, Walton RG. The incidence of birthmarks in the neonate. Pediatrics 1976;58:218-22.
[Google Scholar]
|
| 12. |
Cordova A. The mongolian spot. A study of ethnic differences and a literature review. Clin Pediatr 1981;20:714-9.
[Google Scholar]
|
| 13. |
Hidano A, Purwoko R, Jitsukawa K. Statistical survey of skin changes in Japanese neonates. Pediatr Dermatol 1986;3:140-4.
[Google Scholar]
|
| 14. |
Pratt AG. Birthmarks in infants. Arch Dermatol 1953;63:302-5.
[Google Scholar]
|
| 15. |
Saraçli T, Kenney JA, Scott RB. Common skin disorders in the newborn negro infant. J Pediatr 1963;62:358-62.
[Google Scholar]
|
| 16. |
Nanda A, Kaur S, Bhakoo N, Dhall K. Survey of Cutaneous Lesions in Indian Newborns. Pediatr Dermatol 1989;6:39-42.
[Google Scholar]
|
| 17. |
Leung AK, Kao CP. Extensive mongolian spots with involvement of the scalp. Pediatr Dermatol 1999;16:371-2.
[Google Scholar]
|
| 18. |
Valle LE, Gomez JL, Rausa PM. Dermatosis en el recien nacido. Rev Argent Dermatosifilol 1989;70:102-11.
[Google Scholar]
|
| 19. |
Lin RL, Tinkle LL, Janniger CK. Skin care of the healthy newborn. Cutis 2005;75:25-30.
[Google Scholar]
|
| 20. |
Jorgenson RJ, Saphiro SD, Salinas CF, Levin LS. Intraoral findings and anomalies in neonates. Pediatrics 1982;69:577-82.
[Google Scholar]
|
| 21. |
Hidano A, Kobayashi T. Adnexal polyp of neonatal skin. Br J Dermatol 1975;92:659-62.
[Google Scholar]
|
| 22. |
Hiroko K. Adnexal polyp of neonatal skin observed beyond the neonatal period. Acta Derm Venereol 1998;78:391-2.
[Google Scholar]
|
| 23. |
Paller AS, Mancini AJ. Cutaneous disorders of the newborn. In: Paller AS, Mancini AJ, editors. Hurwitz Clinical Pediatric Dermatology: A Textbook of Skin Disorders of Childhood and Adolescence. 3 rd ed. Philadelphia: Elselvier Saunders; 2006. p. 17-47.
[Google Scholar]
|
| 24. |
Snow TM. Mongolian spots in the newborn: Do they mean anything? Neonatal Netw 2005;24:31-3.
[Google Scholar]
|
| 25. |
Ashrafi MR, Shabanian R, Mohammadi M, Kavusi S. Extensive Mongolian spots: A clinical sign merits special attention. Pediatr Neurol 2006;34:143-5.
[Google Scholar]
|
| 26. |
Igawa HH, Ohura T, Sugihara T, Ishikawa T, Kumakiri M. Cleft lip Mongolian spot: Mongolian spot associated with cleft lip. J Am Acad Dermatol 1994;30:566-9.
[Google Scholar]
|
| 27. |
Torrelo A, Zambrano A, Happle R. Large aberrant mongolian spots coexisting with cutis marmorata telangiectatica congênita (phacomatosis pigmentovascularis type V or phacomatosis cesiomarmorata). J Eur Acad Dermatol Venereol 2006;20:308-10.
[Google Scholar]
|
| 28. |
Korf BR. Diagnostic outcome in children with multiple café au lait spots. Pediatrics 1992;90:924-7.
[Google Scholar]
|
| 29. |
Urbani CE, Betti R. Accessory mammary tissue associated with congenital and hereditary nephrourinary malformations. Int J Dermatol 1996;35:349-52.
[Google Scholar]
|
| 30. |
Resnick KI, Soltani K, Bernstein JE, Fathizadeh A. Accessory tragi and associated syndromes involving the first branchial arch. J Dermatol Surg Oncol 1981;7:39-41.
[Google Scholar]
|
| 31. |
Alper J, Holmes LB, Mihm MC. Birthmarks with serious medical significance: Nevocellular nevi, sebaceous nevi, and multiple café au lait spots. J Pediatr 1979;95:696-700.
[Google Scholar]
|
| 32. |
Osburn K, Schosser RH, Everett MA. Congenital pigmented and vascular lesions in newborn infants. J Am Acad Dermatol 1987;16:788-92.
[Google Scholar]
|
Fulltext Views
4,973
PDF downloads
2,431





