Translate this page into:
Frequency of birthmarks and transient skin lesions in newborns according to maternal factors (diseases, drugs, dietary supplements, and tobacco)
2 Department of Dermatology, Complexo Hospitalario Universitario de Santiago de Compostela (CHUS), SERGAS, Faculty of Medicine, Santiago de Compostela, Spain
3 Departement of Pediatrics, Hospital Arquitecto Marcide, �rea Sanitaria de Ferrol, SERGAS, Ferrol, Spain
Correspondence Address:
Benigno Monteagudo
Department of Dermatology, Hospital Arquitecto Marcide, Avenida da Residencia s/n, Ferrol, 15405 A Coru�a
Spain
| How to cite this article: Monteagudo B, Labandeira J, Le�n-Mui�os E, Carballeira I, Cabanillas M, Su�rez-Amor �, Gonz�lez-Vilas D, Fern�ndez-Prieto R, Toribio J. Frequency of birthmarks and transient skin lesions in newborns according to maternal factors (diseases, drugs, dietary supplements, and tobacco). Indian J Dermatol Venereol Leprol 2011;77:535 |
Sir,
Many studies have examined the impact of maternal diseases and the use of illicit drugs, medication, and dietary supplements during pregnancy on the health of newborns. Interestingly, only Boccardi et al. and Sachdeva et al. have correlated these factors with the presence of birthmarks and transient benign cutaneous lesions. [1],[2] Our goal here is to analyse the influence of these maternal factors on the frequency of 17 neonatal dermatoses.
We conducted a prospective study between May 2008 and November 2009, on 1000 newborns in the first 3 days of life at a perinatal clinic at Hospital Arquitecto Marcide, Ferrol Healthcare Area, Spain. Prevalence of neonatal skin lesions was determined by means of clinical diagnosis. [3] A data collection protocol was followed in each case to identify: (1) maternal factors (diseases, toxic habits, medications, and dietary supplements) and (2) neonatal parameters (gestational age and birthweight).
Data for the quantitative variables was categorised into groups. The qualitative variables were presented as a percentage and were analysed using the χ2 -test. The programme SPSS version 15.0 was used for the statistical analysis. Significance was established as P<0.05.
[Figure - 1] shows the percentage of mothers with toxic habits, diseases, and medications and dietary supplements taken during pregnancy (in 989 mothers). [Table - 1] shows the variations in the frequency of skin lesions according to the maternal parameters. There were no significant differences in the prevalence of dermatoses in relation to maternal diseases. There were statistically significant differences for the salmon patches and erythema toxicum neonatorum in relation to toxic habits, vernix caseosa to drug intake during pregnancy, and palatal cyst, vernix caseosa and jaundice in relation to dietary supplements.
 |
| Figure 1: Percentage of mothers with toxic habits, diseases, and medications or dietary supplements taken during pregnancy |
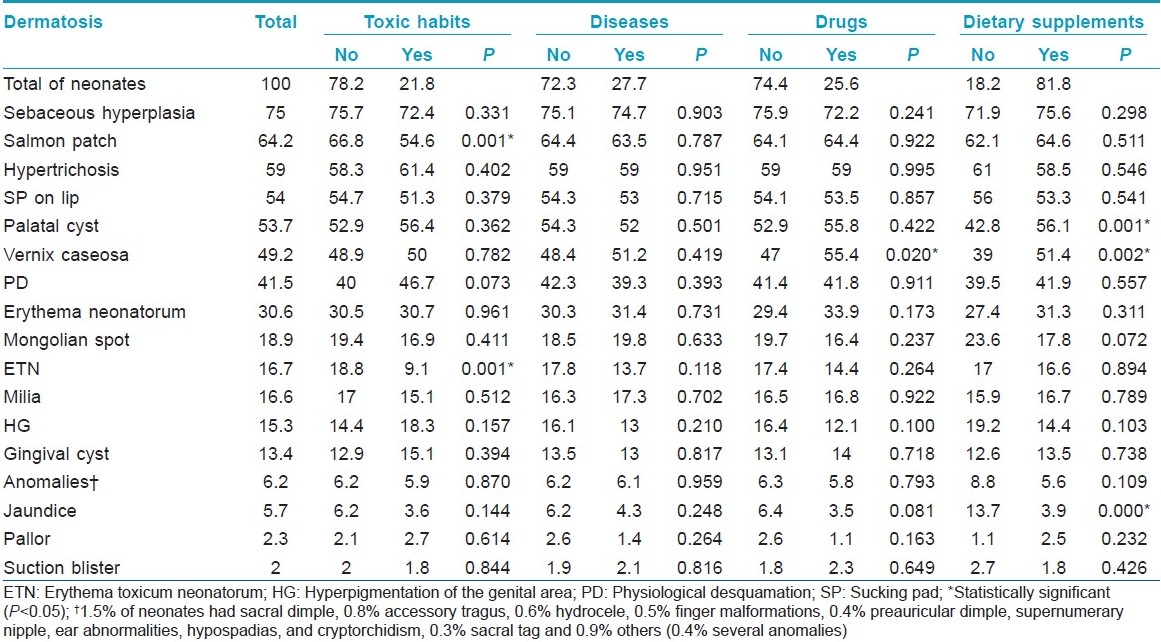
The dermatoses with significant association were related to smoking and the specific group taking medication or a dietary supplement. There was less prevalence of salmon patch and erythema toxicum neonatorum in infants of smoking mothers [Figure - 2]. A higher frequency of vernix caseosa was related to the administration of medication (when drug classes were individualised, there was no longer a significant difference), and dietary supplements (significant for iodine and iron) during pregnancy [Figure - 3]. Maternal intake of iodine and folic acid was associated with a higher prevalence of palatal cysts. The intake of iodine, folic acid, and iron was associated with a lower risk of jaundice in the first 3 days of life.
 |
| Figure 2: Generalized erythema toxicum neonatorum on the back |
 |
| Figure 3: Vernix caseosa in skin folds |
Maternal toxic habits during pregnancy were associated with less frequent salmon patch and erythema toxicum neonatorum. The prevalence of these two dermatoses rose with higher birthweight and gestational age of the newborn. [4] Exposure to smoking shortened the length of pregnancy and reduced the weight of the newborns by an average of 200 g. This partly explains the association of salmon patch and erythema toxicum neonatorum in nonsmokers. Some authors believe that salmon patch reflects persistence of the foetal circulatory model. At present erythema toxicum neonatorum is considered to be an immune response to microbial colonization on the part of commensal microbes within hair follicles. Since smoking affects the cardiovascular system and innate immunity, a "direct" influence on the pathogenesis of these two cutaneous conditions cannot be ruled out.
A history of maternal disease during pregnancy significantly affects foetal health. Interestingly in our study, it did not significantly influence the onset of neonatal dermatoses. [2]
In our study, the intake of medication during pregnancy was significantly associated with an increased frequency of vernix caseosa in the newborn. This contradicts the findings of Boccardi et al., who found little relationship. [1]
The intake of dietary supplements was associated with increased prevalence of palatal cysts and vernix caseosa and decreased frequency of jaundice. An inadequate supply of nutrients during pregnancy is associated with significant foetal and perinatal morbidity. This deficiency increases the possibilities of low birthweight, prematurity, malformations, and impaired immune function, facilitating the development of infections. Palatal cysts and vernix caseosa are less common in premature and very low birthweight infants. [5] This could be one of the reasons that an adequate supply of nutrients is related to the presence of these two conditions. Furthermore, adequate nutrients reduce the onset of jaundice, which occurs, among other predisposing factors, when there is low birthweight, lower gestational age, and congenital infections (the presence of which is reduced with adequate nutrition).
In conclusion, we found a relation among the prevalence of salmon patch and erythema toxicum neonatorum and smoking, vernix caseosa and medication intake, and palatal cyst, vernix caseosa and jaundice and dietary supplementation. Further studies would be needed to confirm these findings in terms of the degree of exposure to smoking and the dose and duration of medication taken.
| 1. |
Boccardi D, Menni S, Ferraroni M, Stival G, Bernardo L, La Vecchia C, et al. Birthmarks and transient skin lesions in newborns and their relationship to maternal factors: A preliminary report from northern Italy. Dermatology 2007;215:53-8.
[Google Scholar]
|
| 2. |
Sachdeva M, Kaur S, Nagpal M, Dewan SP. Cutaneous lesions in new born. Indian J Dermatol Venereol Leprol 2002;68:334-7.
[Google Scholar]
|
| 3. |
Monteagudo B, Labandeira J, León-Muiños E, Carballeira I, Corrales A, Cabanillas M, et al. Prevalence of birthmarks and transient skin lesions in 1,000 spanish newborns. Actas Dermosifiliogr 2011;102:264-9.
[Google Scholar]
|
| 4. |
Ferahbas A, Utas S, Akcakus M, Gunes T, Mistik S. Prevalence of cutaneous findings in hospitalized neonates: A prospective observational study. Pediatr Dermatol 2009;26:139-42.
[Google Scholar]
|
| 5. |
Gokdemir G, Erdogan HK, Köslü A, Baksu B. Cutaneous lesions in Turkish neonates born in a teaching hospital. Indian J Dermatol Venereol Leprol 2009;75:638.
[Google Scholar]
|
Fulltext Views
2,459
PDF downloads
2,477





