Translate this page into:
Treatment of recalcitrant granulomatous rosacea with ALA-PDT: Report of a case
Correspondence Address:
Francesco Baglieri
Department of Dermatology, S. Elia Hospital, Via Luigi Russo 6, 93100 Caltanissetta (CL)
Italy
| How to cite this article: Baglieri F, Scuderi G. Treatment of recalcitrant granulomatous rosacea with ALA-PDT: Report of a case. Indian J Dermatol Venereol Leprol 2011;77:536 |
Sir,
Granulomatous rosacea (GR), considered as a distinct histological variant of rosacea, is a rare condition characterized clinically by an eruption of reddish papules or small nodules, on a thickened erythematous base, which appear indurated, and histologically by the presence of non-caseating epithelioid cell granulomas in the dermis.
The eyelids, lower part of the forehead, nasolabial folds, cheeks and perioral area are frequent sites of involvement. The course is chronic and unremitting. [1],[2]
Although the exact etiopathogenesis of GR is unknown, a role of delayed hypersensitivity reaction against keratinized cells, pilosebaceous structures and microbial organisms has been suggested. [3]
Treatment of GR is not different from classical rosacea and the use of oral antibiotics such as tetracycline, doxycycline, or minocycline is usually effective. [4] Nevertheless, tendency to relapse or recur may persist for several years, with an increase of antibiotic resistances.
The utilization of δ-aminolaevulinic acid-photodynamic therapy (ALA-PDT) for various potential nononcological indications has been widely explored, with some positive evidences for its efficacy in many inflammatory dermatoses. [5]
Rosacea associated erythema, papules, pustules, and flushing have been successfully treated with PDT. [6],[7]
A 50-year-old male patient presented with a 6-year history of facial erythema with multiple painful brownish-red papules and little nodules, on an infiltrated erythematous base, predominantly involving the chin, the cheeks and the neck below the mandible [Figure - 1].
 |
| Figure 1: Facial erythema with numerous brownish-red papules and nodules, on an infiltrated erythematous base |
During the last 2 years, before our examination, the patient had failed standard pharmacological treatments with tetracycline and its derivatives.
The results from routine laboratory tests were within normal limits. Serology for syphilis, HIV test (HIV 1-2), antinuclear antibodies, and an intradermal tuberculin test were negative. Chest radiography did not show signs of extracutaneous involvement.
Histopathological examination revealed multiple noncaseating epithelioid cell granulomas with surrounding mononuclear cell infiltrate and Langhans′ type giant cells in the superficial as well as deep dermis [Figure - 2].
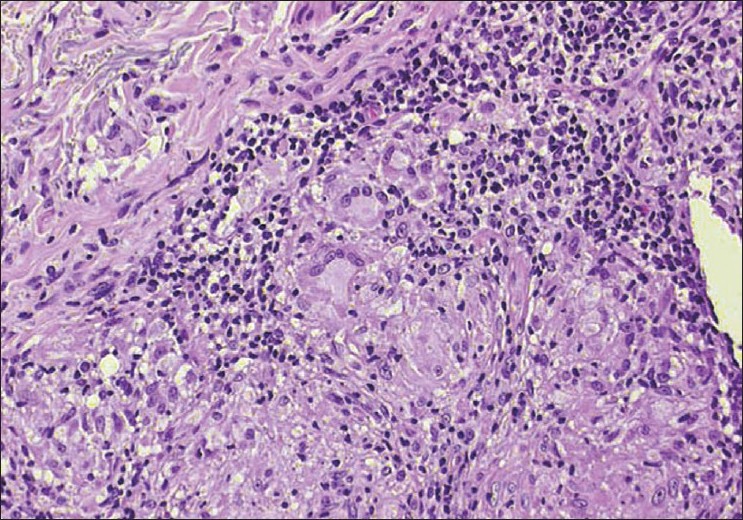 |
| Figure 2: Epithelioid cells granulomas with Langhan's type giant cells in the dermis (H and E, ×400) |
Given the resistance to the conventional therapy with systemic antibiotics, treatment with ALA--PDT was undertaken. The patient received six sessions of PDT with δ-aminolaevulinic acid (ALA) at a concentration of 20% prepared in a base cream, applied with an occlusive dressing for 3 h, given at 2-weeks intervals. Irradiation source was a tungsten lamp with a spectrum emission ranging from 400 to 700 nm, peaking at 630 nm, with a total light dose that was 40 J/cm 2 .
Improvement was evident after the third treatment and was estimated "good" after the sixth treatment, in absence of adverse events and collateral effects [Figure - 3].
 |
| Figure 3: The patient at (a) after the sixth treatment with ALA-PDT and (b) baseline |
Although the exact mechanism of PDT action in the rosacea treatment is still unclear, many findings suggest that it could be attributed to the antimicrobial and anti-inflammatory effects (photodestruction of Demodex mites and associated bacteria, T lymphocytes apoptosis, induction of matrix metalloproteinases MMP-1 and MMP-3 by dermal fibroblasts).
Porphyrins are synthesized in vivo from δ-aminolevulinic acid (ALA), particularly in pilosebaceous units that seems to be therefore the "target" structure in the mechanism of PDT action in the treatment of rosacea. [7]
| 1. |
Sánchez JL, Berlingeri-Ramos AC, Dueño DV. Granulomatous rosacea. Am J Dermatopathol 2008;30:6-9.
[Google Scholar]
|
| 2. |
Wilkin J, Dahl M, Detmar M, Drake L, Feinstein A, Odom R, et al. Standard classification of rosacea: Report of the National Rosacea Society Expert Committee on the Classification and Staging of Rosacea. J Am Acad Dermatol 2002;46:584-7.
[Google Scholar]
|
| 3. |
Helm KF, Menz J, Gibson LE, Dicken CH. A clinical and histopathologic study of granulomatous rosacea. J Am Acad Dermatol 1991;25:1038-43.
[Google Scholar]
|
| 4. |
Kennedy Carney C, Cantrell W, Elewski BE. Rosacea: A review of current topical, systemic and light-based therapies. G Ital Dermatol Venereol 2009;144:673-88.
[Google Scholar]
|
| 5. |
Nestor MS, Gold MH, Kauvar AN, Taub AF, Geronemus RG, Ritvo EC, et al. The use of photodynamic therapy in dermatology: Results of a consensus conference. J Drugs Dermatol 2006;5:140-54.
[Google Scholar]
|
| 6. |
Katz B, Patel V. Photodynamic therapy for the treatment of erythema, papules, pustules, and severe flushing consistent with rosacea. J Drugs Dermatol 2006;5:6-8.
[Google Scholar]
|
| 7. |
Zakhary K, Ellis DA. Applications of aminolevulinic acid-based photodynamic therapy in cosmetic facial plastic practices. Facial Plast Surg 2005;21:110-6.
[Google Scholar]
|
Fulltext Views
2,283
PDF downloads
2,868





