Translate this page into:
1064 nm Q switched Nd: YAG laser treatment of nevus of Ota: An Indian open label prospective study of 50 patients
Correspondence Address:
Hemanta Kumar Kar
Department of Dermatology, STD and Leprosy, Dr. RML Hospital and PGIMER, Baba Kharak Singh Marg, New Delhi 110 001
India
| How to cite this article: Kar HK, Gupta L. 1064 nm Q switched Nd: YAG laser treatment of nevus of Ota: An Indian open label prospective study of 50 patients. Indian J Dermatol Venereol Leprol 2011;77:565-570 |
Abstract
Background: Nevus of Ota is very common in Asians. Estimated male to female ratio is 1:4.8. Patients seek treatment early in life due to psychological trauma and cosmetic disfigurement. The creation of high power, short pulse Q switched lasers has recently provided tools for considerable therapeutic advances in the treatment of dermal pigmented lesions. Aims: To determine the efficacy and side-effect profile of Q switched Nd:YAG Laser (QSNYL) in fifty Indian patients. Methods: Fifty patients of nevus of Ota underwent multiple treatments (average 5 sessions) at monthly intervals carried out over a period of 2 years with QSNYL (Med-lite C6). Of the 50 patients, 2 were males; and the rest were females. Skin types treated included phototype IV and V. The response after subsequent treatments was documented through serial photographs that were taken before and after every treatment session. Response to the treatment was graded based on quartile grading scale. Results: Near total improvement was seen in 8%, marked improvement in 22%, moderate improvement in 38% and 32% patients reported less than 25% clearing of the lesion. All patients reported some improvement. Transient postinflammatory hyperpigmentation was observed in 4 (8%) patients, which cleared with use of sunscreens and bleaching agents within 2 months. No textural change or scarring was observed in any patient. Conclusions: QSNYL is an easy-to-perform and effective treatment in cases of nevus of Ota in Indian patients with few side effects.Introduction
Nevus of Ota (Oculodermal melanocytosis) is a dermal melanocytic hamartoma that presents in childhood or at adolescence as bluish/slate gray hyperpigmentation along the first or second branch of trigeminal nerve. The pigmentation progressively increases in size and color till puberty. It was first described by Pusey in 1916 in which the patient had both facial and scleral pigmentation. [1] In 1939, the condition was described by the Japanese dermatologist Ota and named nevus of Ota, and it was then its clinical description was given.
In Asian population, it affects 0.014%-0.034% of the population. Age of onset is bimodal, with a larger peak at birth and a smaller peak at adolescence. Nearly all lesions appear by 30 years of age. [2] Distribution is usually unilateral on areas supplied by the ophthalmic and maxillary division of trigeminal nerve(forehead, temple, nose, eyelid, ear and occasionally the scalp). Some patients have ocular lesions characterized by pigmentation of sclera, cornea, iris and retina. Rarely there is involvement of the hard palate. [2],[3] Females are more commonly involved, male:female ratio is 1:4.8.
Most patients seek treatment early in life or in adolescence due to the psychological trauma and cosmetic disfigurement. Treatment options were limited prior to the advent of lasers. Q-switched Nd:YAG laser (QSNYL) has been used successfully to treat a variety of benign, dermal, pigmented lesions, including nevus of Ota lesions. They have changed the approach in managing this condition and have become the mainstay of therapy.
There are several studies which have shown efficacy of Q- switched Nd:YAG laser in photo type II - IV; however, the data in Indian skin is lacking. Results in light complexion individuals cannot be extrapolated to type IV and V skin. There is also a high risk of post-inflammatory hyperpigmentation. Our study was to determine the efficacy and side effect profile of Q Switched Nd:YAG Laser (QSNYL) in an open labeled prospective study involving fifty Indian patients with nevus of Ota.
Methods
Fifty Indian patients with nevus of Ota underwent multiple treatments (average - five sessions) carried at monthly intervals over a period of 2 years (study period from 2007 to 2009) with QSNYL (Med-lite C6, Hoya Con Bio Inc., Fremont, CA, USA). These patients were obtained from out patient department at our hospital and a substantial fraction was referred from other hospitals in the city. None of the patients had received any prior treatment for their lesions. The diagnosis was made on clinical appearance in the skin and the eyes, and skin biopsies were not performed. An informed consent was taken from all patients included in the study. Of the 50 patients, there were 42 females and 8 males. Most were in the age group 21-40 years. There were 19 patients in age group 21-30 years, 23 in age group 31-40 years, 5 in age group 41-50 years, and 3 were more than 50 years of age. Six patients (12%) had bilateral involvement. Skin type treated included photo type IV and V. Sun protection with a broad spectrum sunscreen lotion was advised at the start of therapy and continued throughout the duration of treatment. Topical anesthesia with eutectic mixture of lignocaine and prilocaine was advised 2 h under occlusion prior to laser if the patient desired. No other topical therapy was advised during the treatment. All personnel in the laser room wore appropriate eye protection glasses during treatment. The patient wore a silicone coated lead shield provided by the manufacturer. The area within the orbital rim was not treated.
Therapy was initiated with 1064 nm Q Switched Nd:YAG Laser at 3 mm spot size and fluence 2.5-3 J/cm 2 . End point was immediate whitening of the lesion. The fluence was subsequently increased on subsequent sessions based on the therapeutic response and patient tolerability to a maximum of 8.5 J/cm 2 . The pulse duration was <7 ns. Minimum number of sessions performed were 5 and maximum 15. The end point for treatment was taken as near total improvement or till a maximum of 15 sessions whichever was earlier. However, patients who had completed a minimum of five sessions were included in the study.
Treatment was performed with the hand piece held perpendicular, with minimum overlap. The entire lesion was covered in a single pass.
Evaluation of results was made on visual inspection as well as comparing serial photographs that were taken before starting treatment and after every laser session. Response to treatment in terms of clearance of the lesion was graded based on a quartile grading scale as minimal, moderate, marked, and near total.
Grade I: < 25% improvement, minimal improvement
Grade II: 26%-50% improvement, moderate improvement
Grade III: 51-75% improvement, marked improvement
Grade IV: Greater than 75% improvement, near total improvement
Patients who had no improvement or worsening were also documented. Complications such as hyperpigmentation, hypopigmentation, scarring and erythema were also recorded.
Results
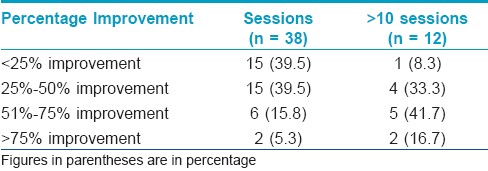
Majority of the patients at the end of the treatments reported some improvement. Near total improvement was seen in 8%, marked improvement in 22%, moderate improvement in 38% and 32% patients reported less than 25% clearing of the lesion. [Figure - 1], [Figure - 2], [Figure - 3], [Figure - 4] and [Figure - 5] demonstrate various grades of clinical improvement. Based on the dermatologist′s clinical assessment of the 50 patients, the mean grade of clinical improvement after treatment was 2.06. Patients were arbitrarily divided into two groups based on the number of treatment sessions received: 5-10 sessions and more than 10 sessions. There were 38 patients who had received 5-10 sessions and 12 patients had received >10 sessions [Table - 1]. On comparing the percentage improvement with the number of sessions using Chi-square test, P<0.05 at 90% confidence interval, we found a statistical correlation between the number of treatment sessions and the therapeutic outcome. The age of patients did not in any way influence the treatment outcome.
Out of the 12 patients in the group who received >10 sessions. 8.3% (1) patient had less than 25% improvement and 33.3% (4) patients had 25-50% response. Out of these, 1 patient with <25% response and 2 patients with 25%-50% response were cases of bilateral nevus of Ota. The remaining three patients with bilateral involvement were administered <10 sessions and had <25% response. Overall, patients who had bilateral involvement did not respond well to QS Nd: YAG laser.
 |
| Figure 1: Clinical photograph of a patient before and after nine sessions with Grade I (minimal) improvement |
 |
| Figure 2: Clinical photograph of a patient before and after seven sessions with Grade I (minimal) improvement |
 |
| Figure 3: Clinical photograph of a patient before and after eleven sessions with Grade II (moderate) improvement |
 |
| Figure 4: Clinical photograph of a patient before and after seven sessions with Grade III (marked) improvement |
 |
| Figure 5: Clinical photograph of a patient before and after ten sessions with Grade IV (near total) improvement |
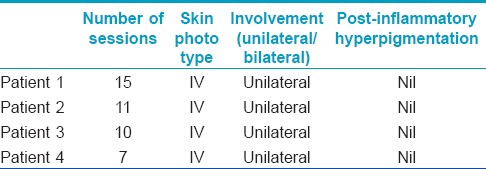
We observed >75% improvement in 4 (8%) patients. Two patients had received <10 sessions and 2 had received >10 sessions. There was no added improvement after 10 sessions in these two patients. Probably, 10 sessions would be appropriate to decide the outcome of laser in a patient, but this may still vary with individual patient characteristic [Table - 2]. However, this number is small in our study to draw a definite conclusion. [Table - 3] shows the patient characteristic and the number of treatments sessions in patients who had 51%-75% improvement after the laser treatment.

There were 16 patients of photo type IV and 19 patients of photo type V. However, on comparing the percentage improvement and the skin type, no statistically significant difference was observed (P > 0.05).
There was no recurrence until 6 months from the time of the last treatment session. No significant adverse effects were observed during or immediately after the treatment. Pricking sensation during treatment and post treatment erythema were common which resolved within few hours. Transient post-inflammatory hyper pigmentation was observed in 4 (8%) patients, which cleared with the use of sunscreens and bleaching agents within 2 months. No textural change or scarring was observed in any patient.
Discussion
The treatment options for nevus of Ota prior to the advent of lasers has been limited. These included cryotherapy, [4] dermabrasion, [5] surgical excision, [6] and cosmetic camouflage. The surgical treatment options were associated with significant scarring and permanent pigment alteration. Q switched (QS) lasers have changed the management of pigmentary lesions to a great extent. Q stands for quality. [7] Q switching is a means of shuttering the laser output so that it is delivered in extremely short pulses of high intensity radiation.
Lasers are monochromatic electromagnetic radiation source used to treat various skin disorders. Anderson and Parrish theory of selective photo-thermolysis states that the laser light must be of wavelength that is well absorbed by the target chromophore (absorption spectrum from 250 to 1200 nm) and not the surrounding structures, the pulse duration should be less than or equal to the thermal relaxation time of the target to avoid collateral thermal damage, and finally sufficient fluence should be used to produce the desired effect. [8],[9],[10] An additional photoacoustic effect is produced when high energy is delivered in short time, produces shock waves and leads to explosion of the target. [11],[12] Q switched lasers QS Nd:YAG (1064 nm), Ruby (694 nm) and Alexandrite (755 nm) produce ultrashort bursts of laser light that specifically target the melanosomes in the dermal melanocytes. [13],[14] Pulse duration is in nano seconds which closely matches to the thermal relaxation time of the melanosomes. [15]
The treatment of pigmentary lesions in darker skin type is associated with risk of pigment alteration. Of all the Q switched lasers available, Q Switched Nd:YAG is best suited for Indian skin type. [15],[16] This wavelength is weakly absorbed by epidermal melanin and has deeper penetration in the dermis. The newer lasers have a larger spot size which allows deeper penetration; minimizing tissue splatter and textural changes. [17] The melanophages subsequently clear the melanin from previously targeted melanocytes. Recurrence is due to the residual melanocytes that have not been targeted or which did not contain sufficient melanin for eradication. Risk of recurrence is estimated between 0.6% and 1.2%. [18],[19]
There have been previous studies in which Q switched lasers have been used for treating nevus of Ota. Geronemus [20] treated 15 patients with QS ruby laser with greater than 50% clearing in all cases. The efficacy of QS ruby laser was later confirmed in another study involving 114 patients which demonstrated good clinical results with few side effects. [21] Later, QS Nd:YAG and QS Alexandrite were used successfully to treat this condition. [22],[23]
The creation of high power, short pulse lasers has recently provided tools for considerable therapeutic advances in the treatment of dermal pigmented lesions. Med-lite C6 laser was used in our study. This laser emits at two wavelengths; the fundamental 1064 nm and 532 nm. For nevus of Ota we operated at 1064 nm, very short pulse duration of <7 ns, 3-mm spot size and a repetition rate of 2 Hz. Nano second pulse duration helps in delivering higher peak power. It has a direct beam delivery hand piece which allows a more uniform top hat profile. It also has a larger spot size which allows for deeper penetration of the target surface, allowing sufficient energy being delivered to the target melanocytes in the dermis. The beam characteristically produces minimum tissue splatter and minimal hot spots in the tissues, thereby minimizing side effects. Finally, the newer QS Nd: YAG laser is ideal in Indian skin type.
In our study, all patients responded well to treatment with 30% patients having more than 50% clinical improvement. We noticed that the therapeutic response was directly proportional to the number of treatment sessions. However, after 10-12 sessions there was no added improvement in the patients. In those patients who do not show initial improvement, few more sessions should always be attempted. Previous studies have shown that patients with bilateral nevus of Ota have more erythema after the laser due to more peri-vascular pigment and are at a higher risk of post inflammatory hyperpigmentation. To avoid this, we started the laser at a low fluence with gradual increment in the fluence as compared to previous studies which use high fluence for treating this condition. To prevent post inflammatory hyperpigmentation topical bleaching agents are also prescribed along with sunscreens in previous studies. [24] However, we limited topical medication to use of sunscreen only.
In our study poor prognostic factor was patients with bilateral nevus of Ota. When we compare our results to that in the phototypes II-III, the results in the type IV-V skin are better. Skin phototype may be another factor that determines the prognosis but no comparative data is available to support this. We also observed a direct correlation between the number of sessions and the treatment outcome, but after 10-12 sessions no added benefit was observed. However, multiple sessions should always be attempted, preferably a minimum of 10 sessions before we stop the treatment.
When the results of QS Nd: YAG laser are compared to QS Alexandrite laser, patients found a better tolerance to the latter. [25] However, QS Nd: YAG laser is found to be more effective after 3 or more sessions. Hypopigmentation is a commonly reported problem with QS ruby laser. [26] Overall, QS Nd: YAG laser is better suited to our skin type though the only limitation is that noticeable improvement may appear late and clinicians need to consider repeated treatments in such cases.
The side effects were few and all of them were reversible. The side effects in our study were comparable with the other Indian study by Aurangabadkar [3] who reported transient hyperpigmentation (10%), hypopigmentation (2%) with no textural change or scarring.
Conclusion
Overall, QS Nd:YAG laser is a good treatment option in nevus of Ota. Patients may require up to 10 sessions for adequate response. Bilateral nevus of Ota is associated with greater risk of post inflammatory hyper pigmentation and responds poorly. On comparing our results with results in lighter skin type, Indians do not show such a dramatic response.
In conclusion, we suggest that QSNYL is an easy-to-perform and effective treatment in cases of nevus of Ota in Indian patients. Patients may require multiple sessions at low fluence. There are few side effects which are transitory in nature.
| 1. |
Bhattacharya SK, Girgla HS, Singh G. Naevus of Ota. Int J Dermatol 1973;12:344-7.
[Google Scholar]
|
| 2. |
Cowan TH, Balistocky M. The nevus of Ota or oculodermal melanocytosis. Arch Opthalmol 1961;65:483-92.
[Google Scholar]
|
| 3. |
Aurangabadkar S. Q-switched Nd:YAG Laser Treatment of Nevus of Ota: An Indian Study of 50 Patients. J Cutan Aesthet Surg 2008;1:80-4.
[Google Scholar]
|
| 4. |
Hosaka Y, Onizuka T, Ichinose M, Yoshimoto S, Okubo F, Hori S, et al. Treatment of nevus of Ota by liquid nitrogen cryotherapy. Plast Reconstr Surg 1995;95:703-11.
[Google Scholar]
|
| 5. |
Hata Y, Matsuka K, Ito O, Matsuda H, Furuichi H, Ishizu N, et al. Treatment of nevus of Ota: Combined skin abrasion and carbon dioxide snow method. Plast Reconstr Surg 1996;97:544-54.
[Google Scholar]
|
| 6. |
Kobayashi T. Microsurgical treatment of naevus of Ota. J Dermatol Surg Oncol 1991;17:936-41.
[Google Scholar]
|
| 7. |
Kilmer SL, Garden JM. Laser treatment of pigmented lesions and tattoos (review). Semin Cutan Med Surg 2000;19:232-44.
[Google Scholar]
|
| 8. |
Anderson RR, Parrish JA. Selective photothermolysis: Precise microsurgery by selective absorption of pulsed radiation. Science 1983;220:524-7.
[Google Scholar]
|
| 9. |
Anderson RR, Margolis RJ, Watanabe S, Flotte T, Hruza GJ, Dover JS. Selective photothermolysis of cutaneous pigmentation by Q switched Nd: YAG laser pulses at 1064nm, 532nm, 355nm. J Invest Dermatol 1989;93:28-32.
[Google Scholar]
|
| 10. |
Dover JS, Margolis RJ, Polla LL, Watanabe S, Hruza GJ, Parrish JA, et al. Pigmented guinea pig skin irradiated with Q-Switched ruby laser pulses: Morphologic and histologic findings. Arch Dermatol 1989;125:43-9.
[Google Scholar]
|
| 11. |
Hruza GJ, Margolis RJ, Watanabe S. Selective photothermolysis of pigmented cells by Q-switched Nd: YAG laser pulses. J Invest Dermatol 1987;88:496.
[Google Scholar]
|
| 12. |
Kilmer SL, Anderson RR. Clinical uses of Q-switched ruby and Q-switched Nd: YAG lasers for treatment of tattoos. J Dermatol Surg Oncol 1993;19:330-8.
[Google Scholar]
|
| 13. |
Polla LL, Margolis RJ, Dover JS, Whitaker D, Murphy GF, Jacques SL, et al. Melanosomes are a primary target of Q-switches ruby laser irradiation in guinea pig skin. J Invest Dermatol 1987;89:281-6.
[Google Scholar]
|
| 14. |
Murphy GF, Shepard RS, Paul BS, Menkes A, Anderson RR, Parrish JA. Organelle specific injury to melanin-containing cells in human skin by pulsed laser irradiation. Lab Invest 1987;49:680-5.
[Google Scholar]
|
| 15. |
Watanabe S, Flotte TJ, Margolis R. The effect of pulse duration on selective pigmented cell injury by dye lasers. J Invest Dermatol 1987;88:523.
[Google Scholar]
|
| 16. |
Grevelink JM, Duke D, van Leeuwen RL, Gonzalez E, DeCoste SD, Anderson RR. Laser treatment of tattoos in darkly pigmented patients: Efficacy and side effects. J Am Acad Dermatol 1996;34:653-6.
[Google Scholar]
|
| 17. |
Kilmer SL, Farinelli WF, Tearney G. Use of a larger spot size for the treatment of tattoos increases clinical efficacy and decreases potential side effects. Lasers Surg Med Suppl 1994;6:51.
[Google Scholar]
|
| 18. |
Chan HH, Kono T. Nevus of Ota: Clinical aspects and management. Skinmed 2003;2:89-98.
[Google Scholar]
|
| 19. |
Chan HH, Leung RS, Ying SY, Lai CF, Chua J, Kono T. Recurrence of nevus of Ota after successful treatment with Q-switched lasers. Arch Dermatol 2000;136:1175-6.
[Google Scholar]
|
| 20. |
Geronemus RG. Q-switched ruby laser therapy of nevus of Ota. Arch Dermatol 1992;128:1618-22.
[Google Scholar]
|
| 21. |
Watanabe S, Takahashi H. Treatment of nevus of Ota with the Q-switched ruby laser. N Engl J Med 1994;331:1745-50.
[Google Scholar]
|
| 22. |
Alster TS, Williams CM. Treatment of nevus of Ota by the Q-switched Alexandrite laser. Dermatol Surg 1995;21:592-6.
[Google Scholar]
|
| 23. |
Apfelberg DB. Argon and Q-switched Neodymium Yttrium-Aluminum-Garnet laser treatment of nevus of Ota. Ann Plast Surg 1995;35:150-3.
[Google Scholar]
|
| 24. |
Lee B, Kim YC, Kang WH, Lee ES. Comparison of characteristics of acquired bilateral nevus of Ota-like macules and nevus of Ota according to therapeutic outcome. J Korean Med Sci 2004;19:554-9.
[Google Scholar]
|
| 25. |
Chan HH, King WW, Chan ES, Mok CO, Ho WS, Van Krevel C, et al. In vivo trial comparing patients' tolerance of Q-switched Alexandrite (QS Alex) and Q-switched Neodymium: Yttrium-Aluminum-Garnet (QS Nd-YAG) lasers in the treatment of nevus of Ota. Lasers Surg Med 1999;24:24-8.
[Google Scholar]
|
| 26. |
Chan HH, Ying SY, Ho WS, Kono T, King WW. An in vivo trial comparing the clinical efficacy and complications of Q-switched 755 nm alexandrite and Q-switched 1064 nm (Nd-YAG) lasers in the treatment of nevus of Ota. Dermatol Surg 2000;26:919-22.
[Google Scholar]
|
Fulltext Views
16,367
PDF downloads
3,107





