Translate this page into:
Localized bullous pemphigoid at urostomy site
Correspondence Address:
Ana Batalla
Dermatology Service, Complejo Hospitalario de Pontevedra, C/Dr. Loureiro Crespo n�2. 36002 Pontevedra
Spain
| How to cite this article: Batalla A, Pe�n G, De la Torre C. Localized bullous pemphigoid at urostomy site. Indian J Dermatol Venereol Leprol 2011;77:625 |
Abstract
Localized bullous pemphigoid occurs in less than one-third of the cases of bullous pemphigoid and it usually appears on the shins. Localized bullous pemphigoid around a stoma site is very uncommon, with few reports in the literature. We report a case of localized bullous pemphigoid at urostomy site and we review its main characteristics. We highlight the importance of considering bullous pemphigoid in chronic bullous lesions on peristomal skin.Introduction
Localized presentation of bullous pemphigoid (BP) occurs in up to 20% of all cases of BP. [1],[2] It may be classified into one scarring form, generally located in head and neck (currently considered a variant of the mucous membrane pemphigoid), and another nonscarring form usually affecting legs, and less frequently palms or soles. [1],[3] Localized BP has also been described on amputation stumps, scars, after ultraviolet radiation and after radiotherapy. [1],[2],[3] The location around a stoma site is infrequent. We report a case of localized BP at urostomy site and discuss the main characteristics of this variant of BP.
Case Report
A 77-year-old man, with cystectomy and urostomy due to surgical intervention for urinary bladder cancer, presented with a 2-month history of itchy blisters and erosions on the abdomen, without improvement despite topical antibiotics. The peristomal area had only been cleaned with saline solution and subsequent placement of gauzes. Physical examination revealed well-marked eroded plaques surrounding the urostomy, on the right lower quadrant of his abdomen [Figure - 1]. Isolated blisters of 15 mm in diameter were also present. Nikolsky′s sign and Asboe-Hansen sign were negative. There were no other skin lesions, and mucous membranes were not affected. The main differential diagnoses were a primary bullous dermatosis and acute contact dermatitis. Skin biopsy specimen revealed a subepidermal blister with eosinophils and erythrocytes within the cleft. In the upper dermis, there was slight edema and inflammatory infiltrate mainly composed of lymphocytes and eosinophils [Figure - 2]. Direct immunofluorescence microscopy from the perilesional skin showed linear deposits of complement fraction 3 (C3) [Figure - 3] and immunoglobulin G (IgG) at the basal layer zone. The diagnosis of peristomal BP was made. Treatment with clobetasol propionate 0.05% cream 10 g daily produced a rapid clinical improvement, with no active lesions and with most of the eroded plaques almost completely healing after a 2-week treatment. The patient had to continue 10 g weekly clobetasol propionate for 2 months, until a complete recovery.
 |
| Figure 1: Well-delineated eroded plaques surrounding the urostomy site |
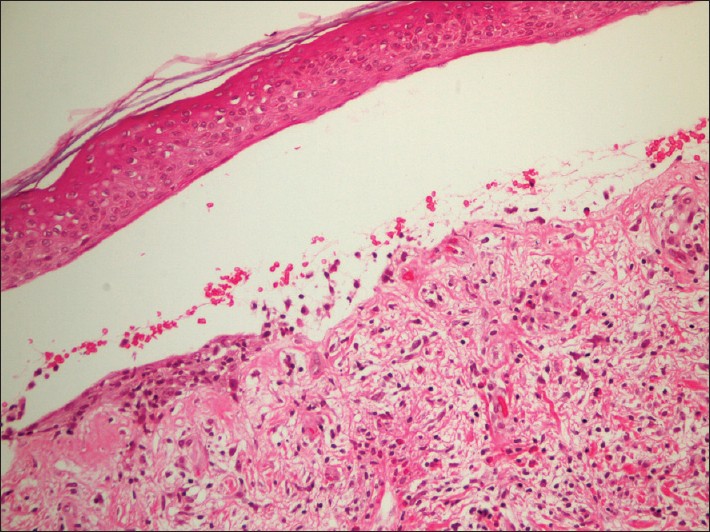 |
| Figure 2: Subepidermal blister with erythrocytes and eosinophils within the cleft and inflammatory infiltrate with lymphocytes and eosinophils in the upper dermis (H and E, ×200) |
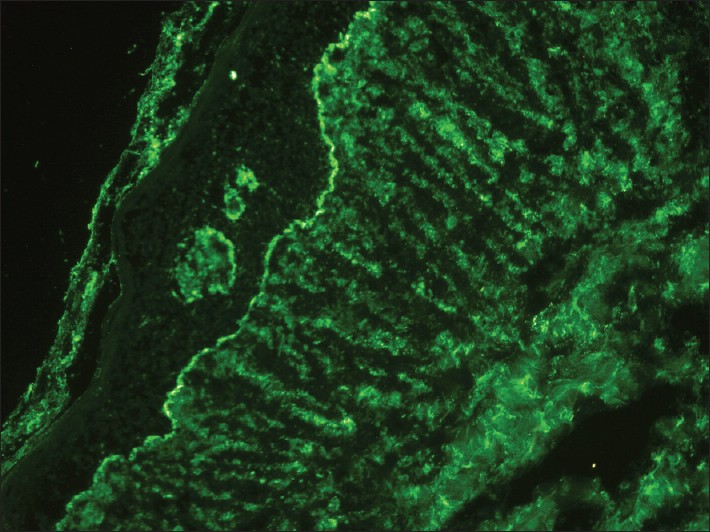 |
| Figure 3: Linear deposit of C3 at the basal layer zone (direct immunofluorescence study, ×200) |
Discussion
BP can present with only localized lesions, or the localized disease may precede generalization by weeks or months, therefore a long-term follow-up is necessary in these patients. [1],[4],[5],[6] The association of BP and malignancy has been suggested, but studies have not showed statistical significance. [7]
Due to the localization of BP on areas of cutaneous injury, a Koebner phenomenon has been suggested. [1],[3] Furthermore, trauma could lead to a predisposition to develop blisters through modifications of the basement membrane zone, which would permit antigen presentation, followed by subsequent autoimmunization. [1],[3],[4] The affected area in the case reported was exposed to continuous trauma and irritation, in agreement with these hypotheses.
Localized BP tends to occur on the legs. [4] The location at a stoma site is uncommon. [3],[6],[7] To the best of our knowledge, only nine cases of peristomal BP have been described in the literature, and the present case is the third report of a BP surrounding a urostomy. [1],[2],[3],[4],[5],[6],[7],[8],[9],[10]
When localized BP appears around a stoma it should be indentified and differentiated from other dermatological conditions, including epidermolysis bullosa acquisita, pyoderma gangrenosum, infection, and especially irritant and allergic contact dermatitis. [2],[3],[5],[7] Cutaneous irritant reactions caused by physical trauma from peristomal hernias, bag changes, or the leakage from the stoma, are frequent complications in stoma patients. Allergic contact dermatitis to dressings and cleaners can occur on peristomal skin. [5] Systematic epicutaneous tests and direct and indirect immunofluorescence studies lead to a correct diagnosis. [3],[5]
Microscopically, both localized and generalized BP demonstrate identical histological features, which have been previously described in our patient. Confirmation of the diagnosis requires direct immunofluorescence studies to detect the presence of IgG or C3 at the epidermal basal layer. [2],[9] Indirect immunofluorescence techniques may demonstrate circulating antibasement membrane antibodies, and serological test may determine antibodies to hemidesmosomal antigens (BP180 and BP230). [6] In the case herein reported, circulating antibodies to BP180 were detected by enzyme immunoassay.
In the treatment of localized BP high-potency topical corticosteroids should be tried initially. Oral tetracycline has been proven efficacious. Other alternatives include oral nicotinamide and in refractory cases, systemic corticosteroids in monotherapy or in combination with other immunosuppressive agents. [1],[2] The combination of dapsone and oral corticosteroids has also showed satisfactory results in recalcitrant disease. [10]
In conclusion, we stress that differential diagnosis of chronic, nonhealing bullous and erosive lesions on peristomal skin should include localized BP.
| 1. |
Marzano AV, Vezzoli P, Colombo A, Serini SM, Crosti C, Berti E. Peristomal bullous pemphigoid. J Dermatol 2010;37:840-2.
[Google Scholar]
|
| 2. |
Vande-Maele DM, Reilly JC. Bullous pemphigoid at colostomy site: Report of a case. Dis Colon Rectum 1997;40:370-1.
[Google Scholar]
|
| 3. |
Salomon RJ, Briggaman RA, Wernikoff SY, Kayne AL. Localized bullous pemphigoid. A mimic of acute contact dermatitis. Arch Dermatol 1987;123:389-92.
[Google Scholar]
|
| 4. |
Guillot B, Doassans S, Degrave B, Crozet I, Basset-Seguin N, Dandurand M. Peristomal subepidermal autoimmune blistering disease. Eur J Dermatol 1999;9:385-6.
[Google Scholar]
|
| 5. |
Cecchi R, Paoli S, Giomi A. Peristomal bullous pemphigoid. J Eur Acad Dermatol Venereol 2004;18:515-6.
[Google Scholar]
|
| 6. |
Caproni M, Ketabchi S, Antiga E, Fabbri P. Bullous pemphigoid initially localized around a urostomy. Int J Dermatol 2006;45:1387-9.
[Google Scholar]
|
| 7. |
Egan CA, Florell SR, Zone JJ. Localized bullous pemphigoid in a patient with B-cell lymphoma. South Med J 1999;92:1220-2.
[Google Scholar]
|
| 8. |
Ng CS, Wolfsen HC, Kozarek RA, Brubacher LL, Kayne AL. Chronic parastomal ulcers: Spectrum of dermatoses. J ET Nurs 1992;19:85-90.
[Google Scholar]
|
| 9. |
Asbrink E, Hovmark A. Clinical variations in bullous pemphigoid with respect to early symptoms. Acta Derm Venereol 1981;61:417-21.
[Google Scholar]
|
| 10. |
Balachandran C, Rai VM. Localised bullous pemphigoid in the breast. Indian J Dermatol Venereol Leprol 2006;72:158-9.
[Google Scholar]
|
Fulltext Views
3,314
PDF downloads
2,241





