Translate this page into:
Cutaneous aspergillosis in a heart-transplant patient
Correspondence Address:
Ana Brinca
Praceta Dr. Mota Pinto, Av. Bissaya Barreto, Coimbra 3000-075
Portugal
| How to cite this article: Brinca A, Serra D, Brites MM, Tellechea �, Figueiredo A. Cutaneous aspergillosis in a heart-transplant patient. Indian J Dermatol Venereol Leprol 2011;77:719-721 |
Sir,
We describe the case of a 67-year-old female with three subcutaneous nodules that had been present for the previous 10 days. She suffered from type 2 diabetes mellitus for 10 years and had undergone heart transplantation for dilated cardiomyopathy 1 year earlier and was undergoing immunosuppression with prednisone 7.5 mg/day, tacrolimus 4 mg/day, and sirolimus 1 mg/day. She was febrile (38--39°C) and reported to have severe asthenia. She denied any respiratory, gastrointestinal, or urinary complaints. There was no palpable lymphadenopathy or hepatosplenomegaly. Chest examination revealed decreased breath sounds and dullness to percussion at the right base. Dermatological examination disclosed three firm and well-demarcated erythematous subcutaneous nodules, 2 cm in diameter, on the left thigh, abdomen, and right infraclavicular area [Figure - 1]. Nodules were only slightly painful.
Thoracic radiological evaluation documented a right pleural effusion and a large nodular opacity in the right inferior pulmonary lobe. Multiple cytological and histological examinations did not reveal neoplastic cells.
 |
| Figure 1: Skin lesion on the abdomen: erythematous subcutaneous nodule |
Histopathological analysis of the skin lesions revealed a massive dermal and hypodermic neutrophilic infiltration [Figure - 2], and wide, septated, uniform hyphae were identified on periodic acid Schiff stain [Figure - 3]. Skin culture as well as bronchial aspirate culture isolated Aspergillus fumigatus. Blood cultures were persistently negative for bacteria and fungi. Antihuman immunodeficiency virus serology was negative.
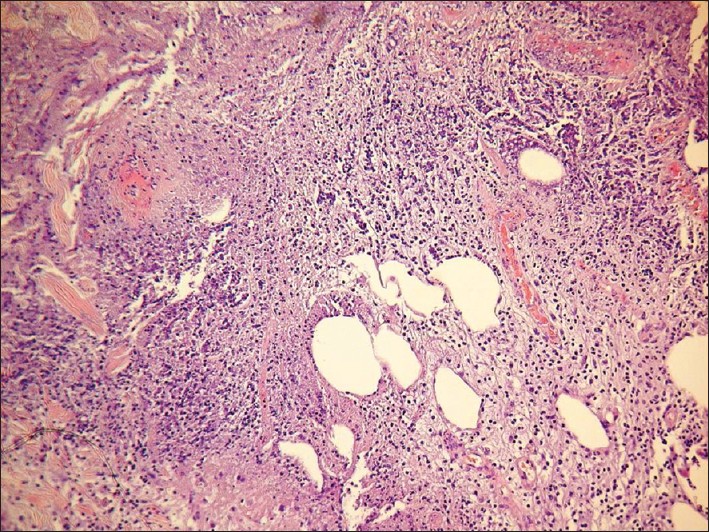 |
| Figure 2: Dermal and hypodermic neutrophilic infiltration (H and E, ×200) |
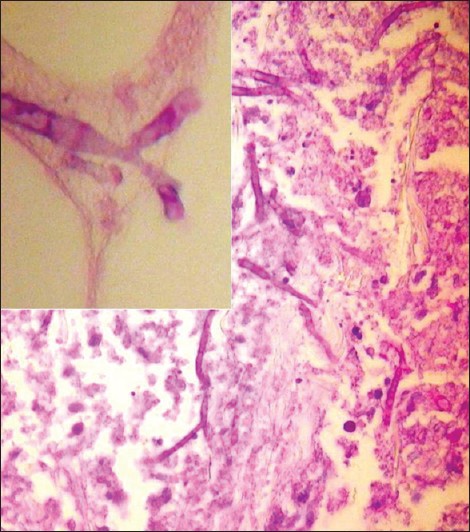 |
| Figure 3: Septated and branching hyphae (Periodic Acid Schiff, ×200; inset: ×40) |
The patient was diagnosed with cutaneous aspergillosis secondary to pulmonary aspergillosis. Insulin therapy was provided to achieve optimal glycemic control. She was started on therapy with liposomic amphotericin B (L AmB) at 5 mg/kg body weight/day intravenously while maintaining the immunosuppressive drugs. About 2 weeks later, following aggravation of the condition with the emergence of new skin lesions, L AmB and sirolimus were suspended, tacrolimus was reduced to 1.5 mg/day, and voriconazole (VOR) was started at 5 mg/kg body weight twice daily orally. Although a clinical improvement was observed almost immediately after 2 days of therapy, followed 7 days later by the regression of skin lesions, the patient died of an extensive acute ischemic cerebrovascular disease after 3 weeks of using VOR, which was confirmed by brain computed tomography.
Fungal infections can cause significant morbidity and even mortality among transplant recipients. After Candida, Aspergillus is the most common genus causing opportunistic fungal infections in these patients. [1] It includes over 185 species, but the most common causative agents of opportunistic infections in humans are Aspergillus flavus, A. fumigatus, A. niger, A. terreus, and A. ustus.[2]
Cutaneous lesions are rare and are usually due to hematogenous dissemination from an underlying infected organ, more commonly the lungs - secondary cutaneous aspergillosis (SCA). More rarely, cutaneous lesions are due to direct inoculation - primary cutaneous aspergillosis - especially in the settings of burns or trauma. Risk factors for invasive aspergillosis include prolonged and severe neutropenia, glucocorticoid therapy, hematopoietic stem cell or solid-organ transplantation, advanced acquired immunodeficiency syndrome, and chronic granulomatous disease. [3] Cutaneous lesions occur in 5-10% of the patients with invasive aspergillosis and, on rare occasions, can be the presenting sign of systemic infection, as had occurred in our patient. In the presenting case, multiple subcutaneous nodules were the revealing lesions of SCA. When the histopathological examination of the cutaneous lesion revealed findings consistent with aspergillosis, a pulmonary primary focus of infection was searched for and found in our patient. Although the radiological findings pointed out to pulmonary neoplasia, this was not confirmed by various histopathological and cytological samples that, indeed, confirmed the infectious nature of the pulmonary mass.
Amphotericin B has been the classical antifungal drug of choice. As the initial therapy for invasive aspergillosis, VOR has shown better response rates, improved survival, and fewer severe adverse effects compared with amphotericin B. [4],[5] Itraconazole and caspofungin are other treatment options. In our patient, who was undergoing immunosuppression with prednisone, tacrolimus, and sirolimus, L AmB was the initial choice to maintain the immunosuppressive drugs because VOR may significantly increase the plasma concentrations of sirolimus, making it mandatory to suspend it.
Early diagnosis and prompt treatment are crucial in the setting of cutaneous aspergillosis, especially in SCA, as it represents an invasive infection with major morbidity and mortality potentials. Therefore, cutaneous nodular lesions arising in the setting of immunosuppression should always lead to search for a systemic infectious focus.
This case has the particularity to demonstrate the risk of fungal infections in transplant recipients even after 1 year of immunosuppression. Previous reports refer to this as a complication occurring in the early posttransplant course. Also, it reminds us that cerebrovascular disease is a leading cause of death in the elderly people, particularly those with diabetes mellitus.
| 1. |
Husain S, Alexander BD, Munoz P, Avery RK, Houston S, Pruett T, et al. Opportunistic mycelial fungal infections in organ transplant recipients: Emerging importance of non-Aspergillus mycelial fungi. Clin Infect Dis 2003;37:221-9.
[Google Scholar]
|
| 2. |
Mohapatra S, Xess I, Swetha JV, Tanveer N, Asati D, Ramam M, et al. Primary cutaneous aspergillosis due to Aspergillus niger in an immunocompetent patient. Indian J Med Microbiol 2009;27:367-70.
[Google Scholar]
|
| 3. |
Denning DW, Stevens DA. Antifungal and surgical treatment of invasive aspergillosis: Review of 2,121 published cases. Rev Infect Dis 1990;12:1147-201.
[Google Scholar]
|
| 4. |
Herbrecht R, Denning DW, Patterson TF, Bennett JE, Greene RE, Oestmann JW, et al. Voriconazole versus amphotericin B for primary therapy of invasive aspergillosis. N Engl J Med 2002;347:408-15.
[Google Scholar]
|
| 5. |
Muñoz P, Singh N, Bouza E. Treatment of solid organ transplant patients with invasive fungal infections: Should a combination of antifungal drugs be used? Curr Opin Infect Dis 2006;19:365-70.
[Google Scholar]
|
Fulltext Views
3,052
PDF downloads
1,328





