Translate this page into:
Primary cutaneous follicle center lymphoma responsive to interferon alfa-2a
2 Department of Pathology, Istanbul Medical Faculty, Istanbul University, Istanbul, Turkey
Correspondence Address:
Ilkin Zindanci
Department of Dermatology, Goztepe Training and Research Hospital, Istanbul
Turkey
| How to cite this article: Kavala M, Zindanci I, Sudogan S, Can B, Turkoglu Z, Kocaturk E, Koc M, Buyukbabani N. Primary cutaneous follicle center lymphoma responsive to interferon alfa-2a. Indian J Dermatol Venereol Leprol 2011;77:729 |
Abstract
Follicular lymphoma is the most common type of primary cutaneous B-cell lymphomas with a predilection for the scalp, forehead, and trunk. Herein we report a case of primary cutaneous follicle center lymphoma on the scalp of 72-year-old female. The diagnosis was made histopathologically, confirming the presence of centrocytes and centroblasts. Complete resolution was achieved following administration of subcutaneous interferon α-2a at a dose of 4.5 × 10 6 IU three times weekly for 3 months.Introduction
Primary cutaneous follicle center lymphoma (PCFCL) or Crosti lymphoma has been classified in the spectrum of primary cutaneous B-cell lymphomas, being the most common type. [1] It is defined as neoplastic proliferations of follicle center cells, usually centrocytes and centroblasts in the skin. [2]
Case Report
A 71-year-old woman referred to our clinic with asymptomatic nodules on the scalp, that first appeared 6 months ago. She had been diagnosed as having herpes zoster and treated with Valacyclovir without any improvement. Upon examination, sharply demarcated, erythematous papules and nodules measuring 2-10 mm in diameter clustered at the right frontotemporal and parietal region were recorded [Figure - 1] and [Figure - 2]. She was otherwise well. The findings of a routine blood screening were normal. Serum antibodies for hepatitis C and Borrelia burgdorferi and HIV-ELISA (enzyme-linked immunosorbent assay) were negative. Serum IgE level was normal. Histological examination revealed a dense lymphoid infiltrate in papillary dermis extending into the deep dermis consisting of centrocytes and centroblasts with sparse histiocytes [Figure - 3]a and b. Immunohistochemical study demonstrated predominantly CD20+ B lymphocytes interspersed with small T lymphocytes [Figure - 3]c and d. The immunostain with CD10 antibody showed a weak positivity in B cells. Occasional residual follicles with dendritic network were observed. The monoclonality of bcl-6 was positive in a majority of B cells, while that of bcl-2 was negative. Staining for Mum-1 showed nuclear positivity in a minority of B cells. A diagnosis of PCFCL was made in view of the extent of the lesions and the patient refused radiotherapy; interferon alpha-2a (IFN- -2a) was administered intramuscularly at a dose of 4.5 × 10 6 IU three times a week for 3 months. The lesions completely disappeared at the end of the treatment with no side effects [Figure - 4].
 |
| Figure 1: Sharply demarcated, erythematous papules and nodules on the scalp |
 |
| Figure 2: Papules and nodules on the scalp |
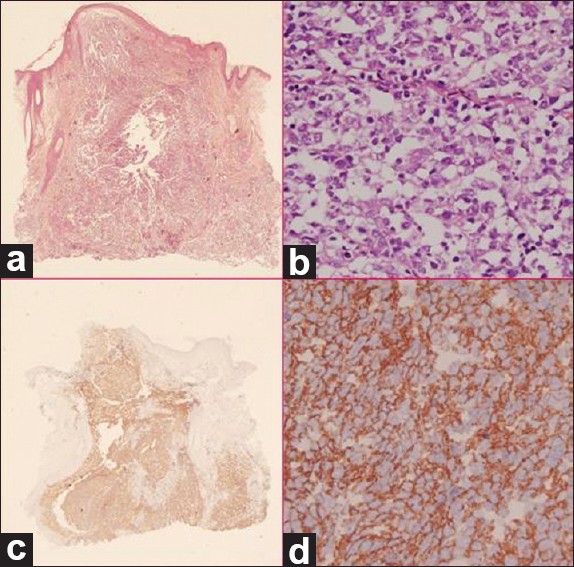 |
| Figure 3: (a) A dense lymphoid infiltrate in papillary dermis extending into the deep dermis infiltration (H and E, ×2). (b) Closer view of lymphoid infiltrate (H and E, ×40). (c) CD20+ B lymphocytes interspersed with small T lymphocytes (×2). (d) Closer view of CD20+ immunostaining (×40) |
 |
| Figure 4: Complete clinical cure after INF-α treatment |
Discussion
PCFCL is recognized as a subtype of primary cutaneous B-cell lymphomas consisting of neoplastic B cells with the morphologic and immunophenotypic characteristics of follicle center cells - usually a mixture of centrocytes (small and large cleaved follicle center cells) and variable numbers of centroblasts (large noncleaved follicle center cells with prominent nucleoli). [1],[2] PCFCL generally presents with localized disease and rarely disseminates to extracutaneous sites. It affects older adults with a slight male predilection and presents clinically with solitary or grouped erythematous papules, plaques and tumors, usually nonulcerated. Lesions are located mostly on the scalp, forehead, and trunk. [1],[3] In our patient, multiple asymptomatic red-brown nodules were located on the scalp with no involvement of any other sites.
Histopathology shows nodular to diffuse infiltrates consisting of centrocytes, centroblasts, and small lymphocytes that can extend down to the subcutaneous fat. The epidermis and papillary dermis are usually not involved. PCFCL may display a follicular, a follicular and diffuse, or diffuse growth pattern. Predominantly, a follicular pattern with germinal center formation can be observed. Occasionally, a diffuse pattern may be seen. In most cases, there is a narrow grenz zone of separation from the overlying epidermis. Neoplastic follicles show a relatively monomorphic cellular composition. [1],[3],[4] The neoplastic follicle center cells express both B-cell-associated antigens CD20 and CD79a as well as the nuclear protein bcl-6. Tumor cells infrequently express CD10 and most cases do not express bcl-2 or show faint bcl-2 staining in a minority of cases. [2],[5] Molecular genetic studies showed that the interchromosomal (14:18) translocation is extremely uncommon in PCFCL, which is characteristically found in systemic follicular lymphomas. [3],[6],[7] However, the presence of t(14:18) and bcl-2 expression is reported in a significant minority of PCFCLs with a follicular growth pattern. [8] In our patient, histopathological and immunohistochemical features supported the diagnosis of PCFCL with a follicular growth pattern showing a weak CD10 staining along with the presence of bcl-6 and occasional network of follicular dendritic cells in the background. [4]
An association with Borrelia burgdorferi, hepatitis C, or human herpesvirus 8 has been described in sporadic patients but does not seem to be a major etiological factor for PCFCL. [9] In our patient, the serological tests for these infections were negative. PCFCL has a very good prognosis, with a 5-year survival greater than 95%, regardless of the pattern of growth. [4] PCFCL must be distinguished from primary cutaneous marginal zone B-cell lymphoma that may present with solitary or multifocal papules, plaques, or nodules localized on the trunk or extremities. [1] Our patient had negative staining for bcl-2, which may serve as a useful adjunct to differentiate PCFCL from primary cutaneous marginal zone B-cell lymphoma.
Current first-line therapeutic modalities include radiotherapy and surgical excision if single or localized lesions are present. Alternative therapies in cases where radiotherapy or surgical removal is not suitable include IFN-α and anti-CD20 antibody. [10] Since IFN-α has an antitumor activity and our patient had scattered lesions on the scalp and refused radiotherapy, a systemic IFN-α-2a was considered as an alternative therapeutic approach. IFN-α, a cytokine crucial for the innate immune response, also demonstrates an antitumor activity. IFNs are capable of modulating a variety of cellular responses, including cell cycle progression and apoptosis. Interferon alfa is a rapid and potent inducer of apoptosis. It also induces cell cycle arrest and inhibits cell growth. Cell growth inhibitory effect of IFN-α has been suggested to be of major importance in antitumor activity. [11],[12] In our patient, complete clinical cure was achieved with systemic IFN-α-2a and there was no sign of recurrence after 1 year of follow-up.
| 1. |
Willemze R, Jaffe ES, Burg G, Cerroni L, Berti E, Swerdlow SH, et al. WHO-EORTC classification for cutaneous lymphomas. Blood 2005;105:3768-85.
[Google Scholar]
|
| 2. |
Burg G, Kempf W, Cozzio A, Feit J, Willemze R, S Jaffe E, et al. WHO/EORTC classification of cutaneous lymphomas 2005: Histological and molecular aspects. J Cutan Pathol 2005;32:647-74.
[Google Scholar]
|
| 3. |
Goodlad JR, Krajewski AS, Batstone PJ, McKay P, White JM, Benton EC, et al. Primary cutaneous follicular lymphoma: A clinicopathologic and molecular study of 16 cases in support of a distinct entity. Am J Surg Pathol 2002;26:733-41.
[Google Scholar]
|
| 4. |
Cerroni L, Arzberger E, Pütz B, Höfler G, Metze D, Sander CA, et al. Primary cutaneous follicle center cell lymphoma with follicular growth pattern. Blood 2000;95:3922-8.
[Google Scholar]
|
| 5. |
Hoefnagel JJ, Vermeer MH, Jansen PM, Fleuren GJ, Meijer CJ, Willemze R. Bcl-2, Bcl-6 and CD10 expression in cutaneous B-cell lymphoma: Further support for a follicle centre cell origin and differential diagnostic significance. Br J Dermatol 2003;149:1183-91.
[Google Scholar]
|
| 6. |
Mirza I, Macpherson N, Paproski S, Gascoyne RD, Yang B, Finn WG, et al. Primary cutaneous follicular lymphoma: An assessment of clinical, histopathologic, immunophenotypic, and molecular features. J Clin Oncol 2002;20:647-55.
[Google Scholar]
|
| 7. |
Child FJ, Russell-Jones R, Woolford AJ, Calonje E, Photiou A, Orchard G, et al. Absence of the t(14;18) chromosomal translocation in primary cutaneous B-cell lymphoma. Br J Dermatol 2001;144:735-44.
[Google Scholar]
|
| 8. |
Lawnicki LC, Weisenburger DD, Aoun P, Chan WC, Wickert RS, Greiner TC. The t(14;18) and bcl-2 expression are present in a subset of primary cutaneous follicular lymphoma: Association with lower grade. Am J Clin Pathol 2002;118:765-72.
[Google Scholar]
|
| 9. |
Lorenzo C, Gatter K, Kerl H. An illustrated guide to skin lymphoma. Massachusetts: Blackwell Publishing; 2004. p. 91-9.
[Google Scholar]
|
| 10. |
Senff NJ, Noordijk EM, Kim YH, Bagot M, Berti E, Cerroni L, et al. European Organization for Research and Treatment of Cancer and International Society for Cutaneous Lymphoma consensus recommendations for the management of cutaneous B-cell lymphomas. Blood 2008;112:1600-9.
[Google Scholar]
|
| 11. |
Sangfelt O, Erickson S, Castro J, Heiden T, Einhorn S, Grandér D. Induction of apoptosis and inhibition of cell growth are independent responses to interferon-alpha in hematopoietic cell lines. Cell Growth Differ 1997;8:343-52.
[Google Scholar]
|
| 12. |
Sangfelt O, Erickson S, Grander D. Mechanisms of interferon-induced cell cycle arrest. Front Biosci 2000;5:D479-87.
[Google Scholar]
|
Fulltext Views
5,081
PDF downloads
2,026





