Translate this page into:
Generalized papular and sclerodermoid eruption: Scleromyxedema
2 Sisli Etfal Training and Research Hospital, Dermatology and Venerology Clinic, Istanbul, Turkey
Correspondence Address:
Ilknur Kivanc Altunay
Sisli Etfal Training and Research Hospital, Dermatology and Venerology Clinic, Sisli - 343 77, Istanbul
Turkey
| How to cite this article: Serdar ZA, Altunay IK, Yasar SP, Erfan GT, Gunes P. Generalized papular and sclerodermoid eruption: Scleromyxedema. Indian J Dermatol Venereol Leprol 2010;76:592 |
Abstract
Scleromyxedema (SM) is a rare chronic progressive and highly intractable cutaneous disease with unknown etiology, affecting both genders equally between 30 and 50 years. The disease is characterized with mucin deposits in the skin and/or other organs. In fact it is a clinicopathological subset of lichen myxedematosus (LM) according to a new classification. Sclerodermiform plaques and lichenoid papules are characteristic cutaneous lesions. An elevation of IgG λ (lambda) chain exists in most cases and extracutaneous involvement occurring with variable systemic findings is also detected. Generalized form is quite difficult to treat and may even be fatal. Herein, we present a male patient with typical features of generalized papular and sclerodermoid LM variety and with benign outcome by isotretinoin.Introduction
Scleromyxedema (SM), which is characterized by generalized lichenoid papules or scleroderma like lesions, is a rare disorder of connective tissue. It is considered among the lichen myxedematosus (LM) or the papular mucinosis group of cutaneous disorders and also referred to as "generalized lichen myxedematosus." [1],[2],[3]
The classification of these group disorders has been more recently updated by Rangioletti. LM [1] has been considered to have three main clinicopathological subsets as generalized, local and atypical or intermediate varieties in this new classification. While localized LM has limited cutaneous involvement and more benign course, generalized LM may show variable extracutaneous involvements. Localized LM may not require therapy and even can be regressed spontaneously. However, generalized form is quite refractory to various therapies. Actually, both the skin and the other organs are prone to be involved extensively in this variety of LM, leading significant morbidity. [1],[2],[3],[4],[5]
Generalized papular and sclerodermoid eruption, namely scleromyxedema, is defined by a triad of specific histopathological features that include mucin deposition, fibrosis and fibroblast proliferation, monoclonal gammopathy and the absence of thyroid disorder. [1],[2],[5] The patient presented herein had generalized papular and sclerodermoid lesions, monoclonal gammopathy, and characteristic histopathologic findings in the skin biopsies. He received systemic isotretinoin and showed significant improvement in six months of the therapy.
Case Report
A 54-years-old male patient presented to us with complaints of edema on his face and eyes, and swelling on the whole body. Swelling was apparent on the ears. It started on the knees approximately 1 year earlier, but it regressed during the subsequent months and papular lesions developed on the neck, arm, and the whole body together with swelling on the face approximately for 5 months. Family history was unremarkable.
General physical examination was normal. Dermatological examination revealed diffuse erythema on the face, induration, coarsening, and grooving both in the forehead lines and in lateral portions of the chin. These changes on the face conformed to lion-like appearance (leonine facies, leontiasis) [Figure - 1]. Diffuse, flesh-colored, waxy firm papules in a millimetric diameter were seen in the nuchal region, neck, lower and upper extremities, wrists and ears [Figure - 2]. The coarsening of the skin folds and diffuse erythema were apparent on the back [Figure - 3].
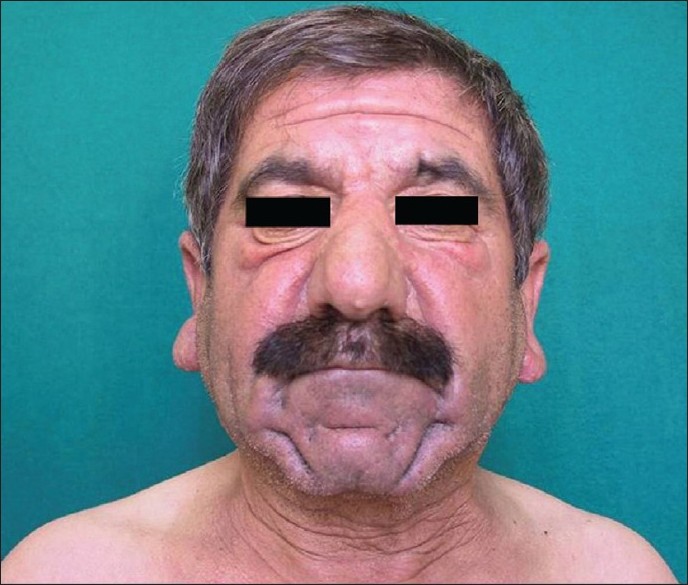 |
| Figure 1 : The patient's facial appearance. Leonine face-like appearance is noteworthy |
 |
| Figure 2 : The coarsening of the skin folds and erythema of the right arm skin |
 |
| Figure 3 : Retroauricular mucinous papules |
In the histopathological examination of the biopsies taken from the dorsal part of the hand and the back, regular appearance in stratum corneum and epidermis, edema of the papillary dermis and the flattening of the retes were observed. Basophilic substance deposits were seen between collagen bundles and they were more dense within the papillary dermis and the reticular dermis. The proliferation of irregularly arranged fibroblasts was present. In the histopathological examination conducted with PAS-Alcian Blue staining, local deposition of mucin was detected in the upper and mid-reticular dermis [Figure - 4].
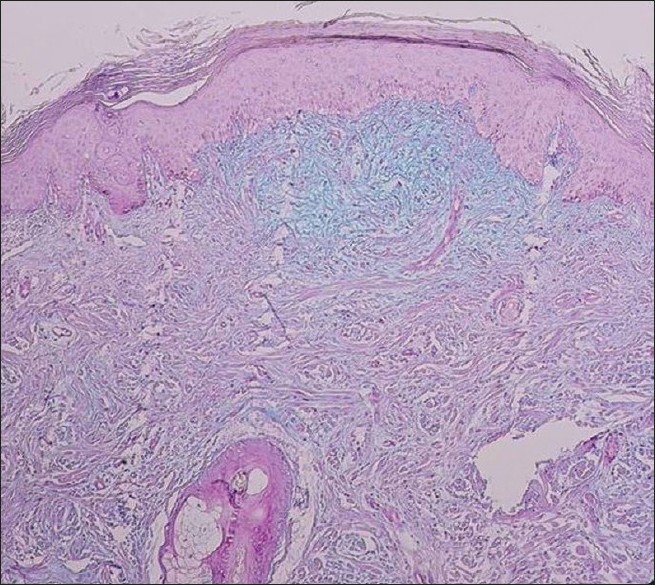 |
| Figure 4 : Histopathologic appearance of the lesional skin: mucin deposition and fibroplast proliferation in the upper and mid-dermis (H and E, ×100) |
In laboratory investigation, complete blood count, complete urine analysis and routine blood biochemistry results were within normal limits. No pathologic cells were determined in peripheral blood smear. Bone marrow biopsy was also normal. Erythrocyte sedimentation rate, C-reactive protein, anti-HIV, hepatitis B and C serology disclosed normal results. Serum total protein, albumin, IgA, IgM, IgG levels, thyroid function tests did not show any abnormal finding but mild elevation in light chain of IgG λ (2.66g/L N: 0.90-2.10 g/L) in the serum electrophoresis.. No pathology was found in flow-cytometric analysis which was applied for differential diagnosis from cutaneous lymphoma. The results of craniography and of abdominal ultrasonography were all evaluated to be normal.
No organ involvement was determined in the patient with physical, laboratory, and radiographic examinations. The diagnosis of scleromyxedema was finally made. Isotretinoin treatment with a dose of 60 mg/day was started. At follow-ups in the third and the sixth months, marked regression in erythema and induration and limited reduction in the number of papules were determined. The treatment of the patient (no adverse effect was detected during therapy) was discontinued at the end of sixth months. At this time, serum electrophoresis was redone and quantitative value of light chain of IgG λ was determined to regress to 2.15 g/L. The patient was in follow-up for a likelihood of development of multiple myeloma; however, we could not see him a few months later. He did not come to visits.
Discussion
Scleromyxedema is a generalized and sclerodermoid form of lichen myxedematosus. It usually affects middle-aged people and equal numbers of women and men. Diagnostic criteria are as follows: [1],[2],[3],[4],[5],[6] (1) generalized papular and sclerodermoid eruption, (2) mucin deposition, fibroblast proliferation and the presence of fibrosis histopathologically, (3) paraproteinemi, i.e. monoclonal gammopathy (typically IgG λ), and (4) the absence of thyroid function disorder.
The pathogenesis of scleromyxedema is exactly unknown. [3] Although increased mucin production by fibroblasts seems to be apparent, the trigger factor for abnormal mucin production is unclear. Monoclonal gammopathy of IgG with λ light chain is common and this abnormality has been considered as a fibroblast stimulant factor. Yet, the role of serum paraprotein in the pathogenesis remains to be elucidated. [5],[6],[7]
The disease may be associated with many systemic disorders. Spectrum of extracutaneous involvement is very wide and changes from dermato-neuro syndrome to renal, pulmonary, and cardiovascular system disorders and even to dermatological disorders such as psoriasis. [4],[5],[7] Monoclonal gammopathy with elevated light chain of serum IgG λ is a common finding observed in more than 80% of patients. [2],[7],[8] Other isotypes of immunoglobulins such as IgG-κ, biclonal IgG/IgA, or polyclonal hypergammaglobulinemia may also be found. [8] Lin et al. has reported that IgG kappa light chain is a predominant immunoglobulin accounted for paraproteinemia. [9] It is reported that mild plasmocytosis might be present in bone marrow and multiple myeloma can develop. Nevertheless, the possibility of progression to multiple myeloma is less than 10%. [1]
The disease is typically chronic and progressive. Although spontaneous improvement may occur, it is extremely rare. Additionally, there are localized and self-healing variants. These variants may occasionally have internal organ involvements and are to be closely followed as they may later develop generalized disease. [2],[10]
Many different agents also including chemotherapeutics are used in treatment. However, the data that related the efficacy of these agents are insufficient, and in fact most of agents are considered to be inefficient. Topical and intralesional hyaluronidase, corticotropin, topical/intralesional/systemic corticosteroid, PUVA, electron beam therapy, plasmapheresis, extracorporeal photochemotherapy, dermabrasion, IVIG therapy, topical dimethyl sulfoxide, a combination of vincristine, idarubicin and dexamethasone with thalidomide (VID schema) have been suggested as therapeutic options even though they do not treat the underlying disease. [7],[8],[9],[10],[11],[12] In fact, melphalan as a cyto-reductive chemotherapeutic agent has been considered to be a first-line therapy for decades. [8],[12] However, some implications in 30% of deaths secondary to its induction of septic complications and hematologic malignancies exist. [8] Autologous peripheral blood stem cell transplantation has been reported to produce dramatic results in some patients [8],[13] Retinoids exert their effects by inhibiting fibroblast proliferation and thus mucin production. [14] Still, therapeutic results from these agents are variable; some patients have good outcome and others do not have. [6],[9],[10],[14] We preferred isotretinoin as therapeutic agent for our patient, both because it was a more manageable drug for us and the patient did not have any internal organ involvement. Although it appears to be successful as a therapeutic agent initially, we cannot know if the disease recurs in the future or the effect is constant.
In conclusion, we think that it is important to collect data of the cases with scleromyxedema because of their variable clinical presentations and different therapeutic outcomes.
| 1. |
Rongioletti F. Lichen myxedematosus (papular mucinosis): new concepts and perspectives for an old disease. Semin Cutan Med Surg 2006;25:100-4.
[Google Scholar]
|
| 2. |
Cokonis Georgakis CD, Falasca G, Georgakis A, Heymann WR. Scleromyxedema. Clin Dermatol 2006;24:493-7.
[Google Scholar]
|
| 3. |
Sperber BR, Allee J, Jamed WD. Self healing papular mucinosis. J Am Acad Dermatol 2004;50:121-3.
[Google Scholar]
|
| 4. |
Lύn YC, Wang HC, Shen JL. Scleromyxedema: an experience using treatment with systemic corticosteroid and review of the published work. J Dermatol 2006;3:207-10.
[Google Scholar]
|
| 5. |
Heymann WR. Scleromyxedema. J Am Acad Dermatol 2007;57:890-1.
[Google Scholar]
|
| 6. |
Hisler BM, Sovaj LB, Hashimoto K. Improvement of scleromyxedema associated with isotretinoin therapy. J Am Acad Dermatol 1991;24:854-7.
[Google Scholar]
|
| 7. |
Pomann JJ, Rudner EJ. Scleromyxedema revisited. Int J Dermatol 2003;42:31-5.
[Google Scholar]
|
| 8. |
Laimer M, Namberger K, Massone C, Koller J, Emberger M, Pleyer L, et al. Vincristine, idarubicin, dexamethasone and thalidomide in scleromyxedema. Acta Dermato Venereol 2009;89:631-5.
[Google Scholar]
|
| 9. |
Lin YC, Wang HC, Shen JL. Scleromyxedema: an experience using treatment with systemic corticosteroiΊd and review of the published work. J Dermatol 2006;3:207-10.
[Google Scholar]
|
| 10. |
Weenig RH, Pittelkow MR. Scleredema and scleromyxedema. In: Wolff K, Goldsmith LA, Katz SI, Gύlchrest BA, Paller ES, Leffell DJ, editors. Fitzpatrick's Dermatology in Medicine. 7th ed. New York: McGraw-Hill; 2008. p. 1562-6.
th ed. New York: McGraw-Hill; 2008. p. 1562-6.'>[Google Scholar]
|
| 11. |
Efthimiou P, Blanco M. Intravenous gammaglobulin and thalidomide may be an effective therapeutic combination in refractory scleromyxedema: case report and discussion of the literature. Semin Arthritis Rheum 2008;38:188-94.
[Google Scholar]
|
| 12. |
Meigel W. Mucinoses. In: Burgdorf WH, Plewig G, Wolf HH, Landthaler M, editors. Braun Falco's Dermatology. 3. th ed. Munich: Springer; 2009. p.1263-73.
th ed. Munich: Springer; 2009. p.1263-73.'>[Google Scholar]
|
| 13. |
Lacy MQ, Hogan WJ, Gertz MA, Dispenzieri A, Rajkumar V, Hayman S, et al. The successful treatment of scleromyxedemawith autologous peripheral blood stem cell transplantation. Arch Dermatol 2005;141:1277-82.
[Google Scholar]
|
| 14. |
Milam CP, Cohen LE, Fenske NA, Ling NS. Scleromyxedema: therapeutic response to isotretinoin in three patients. J Am Acad Dermatol 1988;19:469-77.
[Google Scholar]
|
Fulltext Views
4,068
PDF downloads
2,747





