Translate this page into:
Type I hypersensitivity to Parthenium hysterophorus in patients with parthenium dermatitis
Correspondence Address:
C R Srinivas
Department of Dermatology, PSG Hospitals, Peelamedu, Coimbatore - 641 004
India
| How to cite this article: Lakshmi C, Srinivas C R. Type I hypersensitivity to Parthenium hysterophorus in patients with parthenium dermatitis. Indian J Dermatol Venereol Leprol 2007;73:103-105 |
Abstract
Background: Parthenium dermatitis is a major problem in urban and rural India. Patients with severe allergic rhinitis due to exposure to pollens of parthenium are reported to have parthenium specific IgE and IgG antibodies. Parthenium induces contact dermatitis by Type IV hypersensitivity and allergic rhinitis by Type-I hypersensitivity. Aims: The study was undertaken to detect Type-I and Type-IV hypersensitivity amongst patients with parthenium dermatitis. Methods: Fourteen patients with clinical features of parthenium dermatitis who patch tested positive to parthenium were included in the study. Patch testing was done by standard method and results interpreted as recommended by the ICDRG. Serum IgE was determined by chemiluminescence immuno assay system (CLIA). Prick testing was performed and interpreted by standard method. Results: Twelve out of the 14 patients included, showed a positive prick test. Serum IgE was elevated in all patients to varying degrees (mean IgE-1279.9 IU/ml; N - up to 100 IU/ml). Conclusion: The positive patch test, prick test and elevated serum IgE suggest that both Type-I and Type-IV hypersensitivity may play a role in the induction and perpetuation of parthenium dermatitis in most patients. To date, delayed hypersensitivity was thought to be solely responsible for parthenium dermatitis. This study suggests that a combined type-I and type IV hypersensitivity mechanisms may be operational.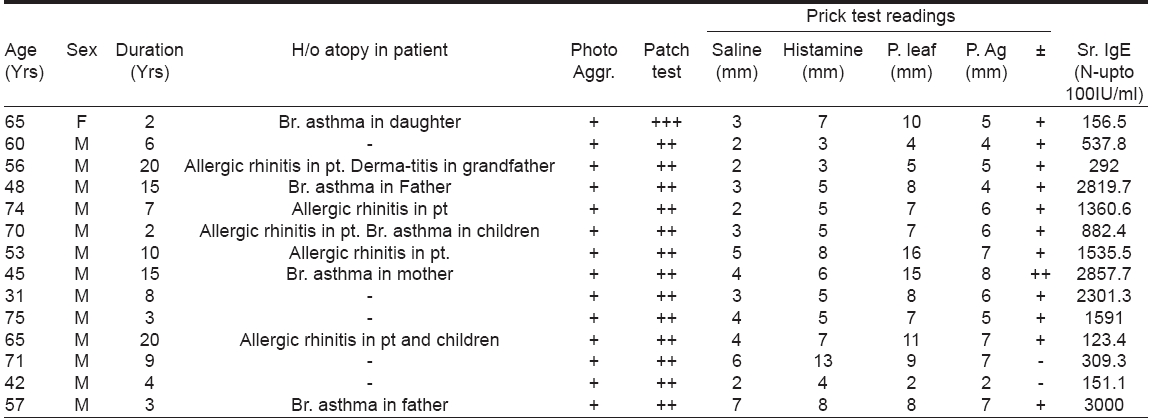
INTRODUCTION
Parthenium dermatitis is a widespread and distressing dermatosis in rural and urban India caused by the air borne allergen of the Compositae weed Parthenium hysterophorus . [1] The disease occurs in sensitized individuals and is thought to be mediated by delayed hypersensitivity (Type IV). Allergic rhinitis due to air borne pollen of parthenium mediated by type-I hypersensitivity has been reported. [2] In this study, patients with parthenium dermatitis were tested for Type-I hypersensitivity. The atopic immune system is characterized by the ability to generate IgE antibodies in response to inhaled or ingested allergens, resulting frequently in a raised total serum IgE. [3] Exacerbation of skin lesions of atopic patients is reported after aeroallergen contact. [4] We postulate that Type I mediated hypersensitivity to Parthenium hysterophorus is common in patients of parthenium dermatitis.
METHODS
Fourteen patients with clinical features of parthenium dermatitis who patch tested positive to parthenium were included in the study. Patients on antihistamines were prick tested only after the drug was withdrawn for 3 days. Patients on immunosuppressants were also included for prick and patch testing. Patients with active liver, renal disease, other photosensitivity disorders, those on photosensitizing drugs and pregnant and lactating females were excluded from the study. A history of atopy in the patient or in the family members was also inquired into.
Patch testing was done using Finn chambers with parthenium antigens (supplied by Systopic Labs©, New Delhi), parthenium leaf and saline. Saline served as the negative control. The reading was taken on Day 2 and Day 4 and the results interpreted as recommended by the ICDRG.
Serum IgE was measured during the active phase of the disease by the chemi-luminescence immuno assay system (CLIA) (ADVIA Centaur© -USA)
Prick testing was done as described below. The immediate reaction was read at 15 minutes; although the late phase reaction (LPR) was not measured, it was observed in 4 hospitalized patients at 48 hours.
Prick test material
- The test solutions were aqueous allergen extracts supplied by Creative Drug Industries (Allergology Division, Navi Mumbai) containing 50% glycerin as stabilizing factor and preserved with 0.4% phenol with their strengths expressed in Protein Nitrogen Units (PNU) and for food series expressed in weight by volume (W/V).
- A blood lancet (MEDI point©, USA) was used for prick testing. The lancet is made of steel with a 1 mm tip and has a shoulder to prevent deeper penetration into the dermis.
Prick testing was done with parthenium leaf, parthenium antigen extract (containing 500 P NU), glycerinated saline as negative control and histamine 0.1% W/V as positive control. Flexor surface of forearm and arm were selected as the test sites.
Interpretation of results was by quantitative assessment by measuring the maximum wheal diameter at 15 minutes. To avoid the chance of a false positive reaction, only values equal to or greater than that of the reading elicited by histamine were considered positive.
RESULTS
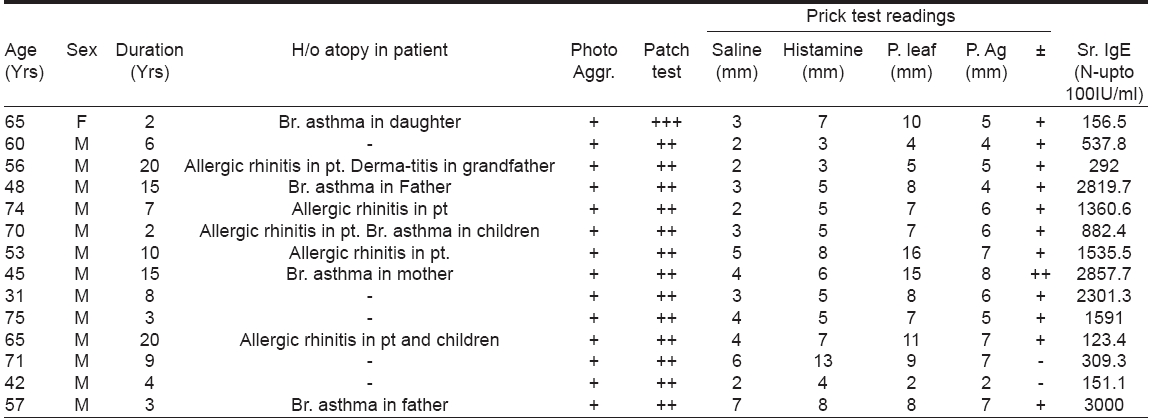
Out of the 14 patients, all (13 male; 1 female) were above the age of thirty. Twelve patients showed a positive prick test, serum IgE was elevated in all patients to varying degrees [Table - 1]. Mean serum IgE was 1279.9 IU/ml (normal - up to 100 IU/ml). Out of the 14 patients included in the study, 9 fulfilled Hanifin and Rajka′s criteria for atopic dermatitis.
DISCUSSION
The weed, Parthenium hysterophorus causes various patterns of dermatitis including air-borne contact dermatitis (ABCD), photodermatitis, atopic dermatitis, actinic reticuloid, exfoliative dermatitis and also photosensitive lichenoid dermatitis. [5],[6],[7]
To date, allergic contact dermatitis (Type IV Coombs and Gell hypersensitivity) is thought to be solely responsible for parthenium dermatitis. [1] Srirama Rao et al found the air borne pollen of Parthenium hysterophorus to be responsible for allergic rhinitis in 42.5% of patients. They concluded that this was caused by induction of immediate hypersensitivity (Type-I) that was demonstrated with positive skin prick tests and IgE and IgG antibodies specific for parthenium pollen allergens. [2] We postulate that a combined Type I and Type IV hypersensitivity is operational in the perpetuation of parthenium dermatitis as evidenced by a positive prick and patch test to parthenium in 12 out of 14 patients included in our study.
Sensitization to allergen in Type I hypersensitivity can occur through skin contact, ingestion, injection and inhalation. [8] Although the serum half-life of IgE is only a few days, mast cells may remain sensitized by IgE for up to 3 months. [8] Generation of IgE antibodies in response to inhaled or ingested allergens is the hallmark of the atopic immune system, resulting frequently in increase of total serum IgE (seen in 80% of patients with atopic dermatitis). [3] In our study, out of 14 patients, 9 fulfilled Hanifin and Rajka′s criteria for atopic dermatitis. All patients showed variable elevation of serum IgE. A history of atopy in 9 out of 14 patients is surprising. Improved diagnostic and data collecting procedures have reported a rising prevalence of atopic dermatitis,however a real increase in the prevalence is also reported. [9]
The patch test detects delayed hypersensitivity while the skin prick test (SPT) detects immediate hypersensitivity. A positive SPT comprises 2 responses- an immediate reaction seen within 15-20 minutes characterized by wheal and flare and a delayed reaction or the late phase reaction (LPR) which occurs at about 5-6 hours and may persist for 1-2 days. It presents as a nodule which is painful rather than itchy but clinically can present as dermatitis. Preformed inflammatory mediators stored in the mast cell granules are responsible for the immediate reaction. [8] The LPR is mediated by newly formed mast cell mediators in concert with other inflammatory cells (eosinophils, neutrophils, lymphocytes). These mechanisms may be involved in the pathogenesis of parthenium dermatitis. IgE mediated late phase reaction (LPR) has been proposed as the link between immediate hypersensitivity and the development of atopic eczematous skin which histologically more closely resembles delayed type hypersensitivity reaction. [10]
Combined immediate-delayed reactions i.e., a combination of type I and type IV reactions occurring in concert in the same patient may be responsible for the perpetuation of the dermatitis. In atopics, aeroallergens that penetrate the skin may attach to IgE - bearing Langerhans cells, IgE bearing dendritic cells in the dermis and IgE bearing mast cells and elicit a combined immediate- delayed reaction. [11] Although it is known that the same chemical can cause both irritant and allergic contact dermatitis it needs to be understood that the same chemical can cause combined Type I and Type IV hypersensitivity. Various animal and vegetable proteins and enzymes can cause immediate and delayed-type allergic dermatitis. [4] Immediate and delayed contact sensitivity to some plants and flowers e.g. chrysanthemum have been described presenting as chronic hand dermatitis. [12]
We postulate that a combined immediate and delayed hypersensitivity mechanism may be similarly operational in the initiation and perpetuation of parthenium dermatitis and that it may also induce exacerbation of lesions of sensitized subjects with atopic diathesis. Awareness about the role of immediate hypersensitivity will improve effective management of parthenium dermatitis. However, a confounding factor in the present study was the large proportion of patients with atopic background. Hence, our findings need to be confirmed by further studies with non-atopic controls.
| 1. |
Lonkar A, Nagasampage BA, Narayanan CR, Landge AB, Sawaikar DD. An antigen from Parthenium hysterophorus Linn. Contact Dermatitis 1976;2:151-4.
[Google Scholar]
|
| 2. |
Sriramarao P, Nagpal S, Rao BS, Prakash O, Rao PV. Immediate hypersensitivity to Parthenium hysterophorus. II. Clinical studies on the prevalence of Parthenium rhinitis. Clin Exp Allergy 1991;21:55-62.
[Google Scholar]
|
| 3. |
Friedmann PS, Holden CA. Atopic dermatitis. In: Rooks textbook of dermatology. Burns T, Breathnach S, Cox N, Griffiths C, editors. Blackwell-Science: USA; 2004. Vol 1, p. 18.1-18.31.
[Google Scholar]
|
| 4. |
Iris Ale S, Maibach HI. Contact urticaria and Hand eczema. In: Hand eczema. Menne T, Maibach HI, editors. 2nd ed. Boca Raton. CRC Press, LLC: Florida; 2000. p. 387-405.
[Google Scholar]
|
| 5. |
Bajaj AK. Contact Dermatitis. In: Valia RJ, editor IADVL Textbook and Atlas of Dermatology. Bhalani Publishing House: Mumbai; 2001. Vol 1, p. 470-1.
[Google Scholar]
|
| 6. |
Shenoi SD, Srinivas CR. Changing clinical patterns of Parthenium dermatitis. Contact Dermatitis 1997;37:128.
[Google Scholar]
|
| 7. |
Verma KK, Sirka CS, Raman M, Sharma VK. Parthenium dermatitis presenting as photosensitive lichenoid eruption: A new clinical variant. Contact Dermatitis 2002;46:286-9.
[Google Scholar]
|
| 8. |
Coico R, Sunshine G. Benjamini E, editors. Hypersensitivity reactions type I In: Immunology a short course, 5th ed. Wiley Liss: New Jersey; 2003. p. 199-211.
[Google Scholar]
|
| 9. |
Carr RD, Berke M, Becker SW. Incidence of atopy in the general population. Arch Dermatol 1964;89:27-32.
[Google Scholar]
|
| 10. |
Gleich GJ. The late phase of the immunoglobulin E-mediated reaction: A link between anaphylaxis and common allergic disease? J Allergy Clin Immunol 1982;70:160-9.
[Google Scholar]
|
| 11. |
Bruynzeel-Koomen C. IgE on Langerhans cells: New insights into the pathogenesis of atopic dermatitis. Dermatologica 1986;172:181-3.
[Google Scholar]
|
| 12. |
Tanaka T, Moriwaki SI, Horio T. Occupational dermatitis with simultaneous immediate and delayed allergy to chrysanthemum. Contact Dermatitis 1987;16:152-4.
[Google Scholar]
|
Fulltext Views
3,273
PDF downloads
2,469





