Translate this page into:
Tuberous sclerosis with portal vein thrombosis, protein C and S deficiency
Correspondence Address:
Biju Vasudevan
Department of Dermatology and Venereology, Base Hospital, Delhi Cantt, New Delhi - 110 010
India
| How to cite this article: Vasudevan B, Sawhney M, Radhakrishnan S, Shilpa G. Tuberous sclerosis with portal vein thrombosis, protein C and S deficiency. Indian J Dermatol Venereol Leprol 2007;73:412-414 |
Abstract
A 29-year-old lady with a bad obstetric history and portal vein thrombosis, presented to the Skin OPD for facial lesions. On examination, angiofibromas on face, shagreen patch and periungual fibromas were observed. She also had dental pits and a retinal hamartoma. Investigations revealed hamartomas in the brain and kidney. Hematological work-up showed protein C and S deficiency with Factor V Leiden positivity. Except for the cutaneous symptoms, the patient did not have any clinical manifestations in other organs affected by tuberous sclerosis. A similar association of tuberous sclerosis with protein C deficiency has been reported in only one case in literature.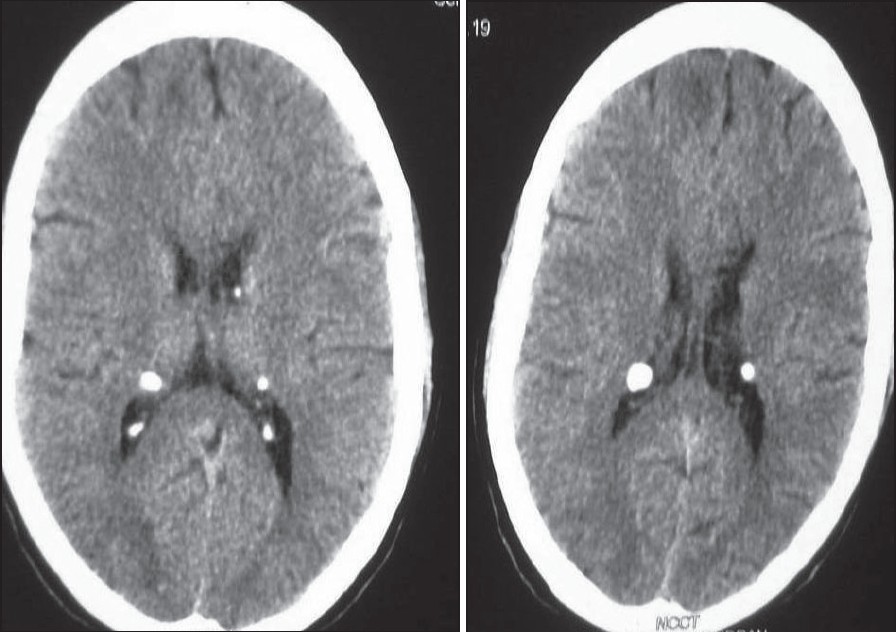 |
| Figure 3: Calcifi ed subependymal nodules on CT scan of brain |
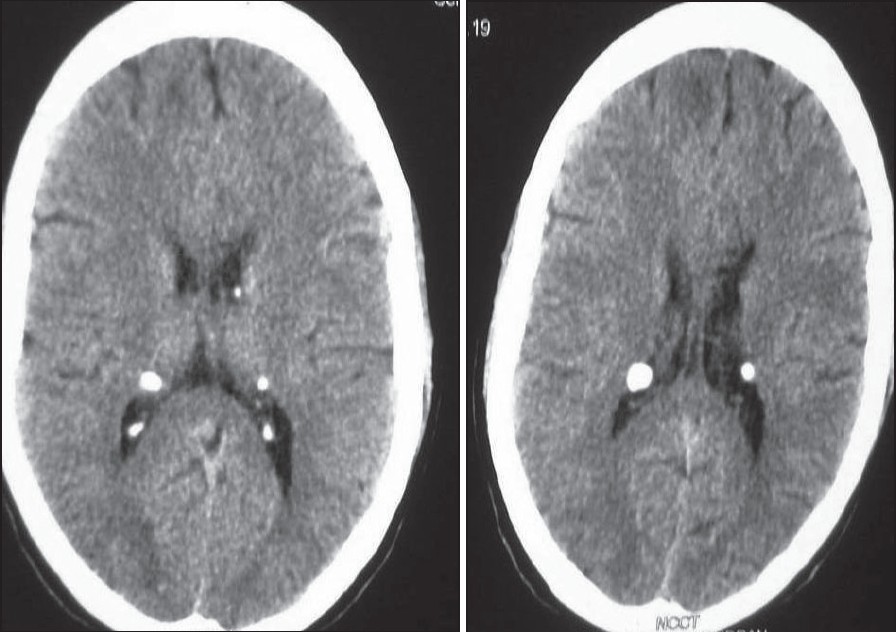 |
| Figure 3: Calcifi ed subependymal nodules on CT scan of brain |
 |
| Figure 2: Dental pits |
 |
| Figure 2: Dental pits |
 |
| Figure 1: Angiofi bromas of face |
 |
| Figure 1: Angiofi bromas of face |
Introduction
Tuberous sclerosis (TS) is an autosomal dominant inherited syndrome of high penetrance characterized by the presence of hamartomas in multiple organ systems. At least 60% of cases represent new mutations. [1] Disorders of the coagulation pathway protein C and S deficiency are genetic disorders characterized by an increased tendency for thrombosis and cause portal vein thrombosis. Association of TS with portal vein thrombosis and protein C deficiency is very rare. To the best of our knowledge, only a single case has been reported. Herein, we present a lady with TS along with protein C and S deficiency with a bad obstetric history.
Case Report
A 29-year-old lady, born to nonconsanguineous parents, who was a known case of portal vein thrombosis (PVT), presented to the skin outpatient department with a history of red raised lesions on the face since the age of 8 years. The lesions had developed after an episode of measles, were nonitchy, painless and persistent. There was no history of seizures, hematemesis, breathlessness or urinary complaints. She was educated till 10 th standard. There was no history of similar complaints in her family. She gave history of six abortions and one preterm triplet delivery, none of whom survived for more than a week. She had an episode of severe pain in the abdomen one and a half years back, wherein CT-Scan of abdomen revealed massive splenomegaly with portal vein thrombosis. Upper GI endoscopy showed Grade III x4 esophageal varices suggesting portal hypertension. Splenectomy was performed. However, linorenal shunt was deferred, as there were multiple small collaterals and cavernoma at splenic hilus. The varices were ligated. Postoperatively, the patient was asymptomatic and was on oral propranolol 20 mg twice daily and oral sorbitrate 10 mg twice daily.
Examination revealed multiple angiofibromas presenting as discrete, firm, reddish-brown papules on face, retroauricular region, neck and upper chest [Figure - 1]; erythematous to skin colored, flat-topped smooth plaques over forehead, back and left thigh; skin colored, soft and pedunculated tags in right axilla; a solitary flat topped, skin to yellow colored plaque measuring 10 x 6 cm on the lower back consistent with shagreen patch and smooth, flesh colored periungual fibromas (Koenen′s tumors) on proximal nail folds of right index and middle fingers. Dental pits were present on the upper incisors [Figure - 2]. Eye examination showed a retinal hamartoma in the right eye. Ultrasound of abdomen revealed multiple small renal angiomyolipomas and CT scan of brain showed multiple calcified subependymal nodules [Figure - 3]. Heart and lungs were normal.
Hematological investigations showed platelet count of 16 lakh per centimeter, hemoglobin 10.2 gm% and total leukocyte count of 14,100/mm 3 . Protein C activity in the blood was 56% (normal range = 70-130%), Protein S was 42% (normal range = 65-140%) and Factor Va Leiden was positive. Investigations concerning thrombotic state including urine hemosiderin, lupus anticoagulant, Ham′s test, sucrose lysis and ACA were negative. Other investigations showed Factor VIII = 80%, Fibrinogen = 273 mg/dL, APTT = 35/36 s and PT = 14/15 s. Color Doppler flow imaging showed portal vein thrombosis with cavernous transformation of portal vein, multiple collaterals around gall bladder wall along with retroperitoneal and perigastric collaterals.
Discussion
Tuberous sclerosis complex (TSC) is a multisystem autosomal dominant disorder with an approximate incidence of 1:10,000-50,000 and characterized pathologically by the presence of hamartomas in multiple organ systems. Hamartomatous lesions can develop in almost any organ except skeletal muscle. [2] The TSC results from mutations in one of two genes, TSC1 (encoding hamartin) or TSC2 (encoding tuberin). [3] The classic triad of epilepsy, low intelligence and adenoma sebaceum (Epiloia) is observed in less than 50% of patients. [4] Additional major features of the disease include dermatologic manifestations, renal angiomyolipomas and pulmonary lymphangiomyomatosis. Our case did not have any manifestations of TSC except for classical cutaneous signs in spite of having hamartomas in multiple organs. Protein C is a potent thrombin-dependent anticoagulant enzyme whose function is to inactivate coagulation cofactors V and VIa and to stimulate fibrinolysis. [5] Hereditary protein C deficiency is inherited as an autosomal dominant trait and is a risk factor for venous thrombosis. The prevalence of protein C deficiency has been estimated to about 0.2% of the general population. Protein S, a vitamin K-dependent physiological anticoagulant, acts as a nonenzymatic cofactor to activated protein C in the proteolytic degradation of factor Va and factor VIIIa. Decreased levels or impaired function of protein S, which is also dominantly inherited, leads to decreased degradation of factor Va and factor VIIIa and an increased propensity to venous thrombosis. The coexistence of a deficiency of anticoagulant proteins, antithrombin or Factor V Leiden greatly increases the risk of thrombosis.
Associations of TS that have been reported include polycystic kidney disease, pancreatic islet cell tumors, insulinoma, multiple endocrine neoplasia and congenital lymphedema. [6],[7],[8] There does not appear to be an established link between TS and protein C deficiency. The former is linked to markers on chromosome 9, whereas the gene for protein C has been isolated and assigned to chromosome 28. [9] Some women may have fetal loss as the only manifestation of protein S deficiency, as noticed in the present case.
A solitary case of a 51-year-old Caucasian woman with TS, portal vein thrombosis and esophageal varices associated with protein C deficiency has been reported. She had adenoma sebaceum, moderate hepatosplenomegaly and renal angiomyolipoma. All investigations to identify the underlying thrombotic state were normal except for a low level of protein C with activity of 53%. [10] Our patient, in addition, also had protein S deficiency with Factor V Leiden positivity and history of six abortions with a preterm triplet, none of whom survived. This case of TS has been reported for the very rare associated above conditions and the absence of symptoms of TS despite the presence of hamartomas in multiple organs. The patient is presently on anticoagulants with regular follow-up.
Acknowledgement
We acknowledge Department of Pathology, Army Hospital, R and R for hematological investigations and Department of Gastroenterology, Army Hospital, R and R for Clinical support.
| 1. |
O'Callaghan FJ. Tuberous sclerosis. BMJ 1999;318:1019-20.
[Google Scholar]
|
| 2. |
Webb DW, Fryer AE, Osborne JP. Morbidity associated with tuberous sclerosis: A population study. Dev Med Child Neurol 1996;38:146-55.
[Google Scholar]
|
| 3. |
Crino PB, Nathanson KL, Henske EP. The tuberous sclerosis complex. N Engl J Med 2006;355:1345-56.
[Google Scholar]
|
| 4. |
Gomez MR. Criteria for diagnosis in tuberous sclerosis. In : Gomez MR. editor. Tuberous sclerosis. 2 nd ed. New York: Raven Press; 1988. p. 9-19.
[Google Scholar]
|
| 5. |
Clouse LH, Comp PC. The regulation of hemostasis: The protein C system. N Engl J Med 1986;314:1298-304.
[Google Scholar]
|
| 6. |
Kim H, Kerr A, Morehouse H. The association between tuberous sclerosis and insulinoma. AJNR Am J Neuroradiol 1995;16:1543-4.
[Google Scholar]
|
| 7. |
Ilgren EB, Westmoreland D. Tuberous sclerosis: Unusual association in four cases. J Clin Pathol 1984;37:272-8.
[Google Scholar]
|
| 8. |
Voudris KA, Skardoutsou A, Vagiakou EA. Tuberous sclerosis and congenital lymphedema. Pediatr Dermatol 2003;20:371-3.
[Google Scholar]
|
| 9. |
Rocchi M, Roncuzzi L, Santamari R, Aehidio N, Dente L, Romeo G. Mapping through somatic cell hybrids and C-DNA probes of protein-C to chromosome 2, factor X to chromosome 13 and alpha I-acid glycoprotein to chromosome 9. Hum Genet 1986;74:30-3.
[Google Scholar]
|
| 10. |
Okafor B, Dawson P, Murray-Lyon IM, Reynolds KW, Samson D. Extrahepatic portal hypertension protein C deficiency and tuberous sclerosis. J R Soc Med 1991;84:751-2.
[Google Scholar]
|
Fulltext Views
1,927
PDF downloads
952





