Translate this page into:
Keloidal granuloma faciale with extrafacial lesions
Correspondence Address:
Rajesh Verma
Department of Dermatology, Venereology and Leprosy, Command Hospital, Pune
India
| How to cite this article: Verma R, Das A L, Vaishampayan S S, Vaidya S. Keloidal granuloma faciale with extrafacial lesions. Indian J Dermatol Venereol Leprol 2005;71:345-347 |
Abstract
Granuloma faciale (GF) is a rare cutaneous disorder characterized by one to several soft, erythematous to livid papules, plaques or nodules, usually occurring on the face. Extrafacial lesions are uncommon. A 52-year-old lady with multiple asymptomatic, variously sized brownish-black colored, firm, sharply circumscribed plaques resembling keloids on both cheeks and extrafacial lesions on the right arm and the right breast is presented for its unusual keloidal appearance and typical histopathological findings. She failed to respond to oral dapsone 100 mg daily administered for 3 months. Local infiltration of triamcinolone combined with cryotherapy led to only partial flattening of the lesions. All the skin lesions were excised surgically followed by flap transfer grafting on both cheeks. The cosmetic outcome was highly satisfactory.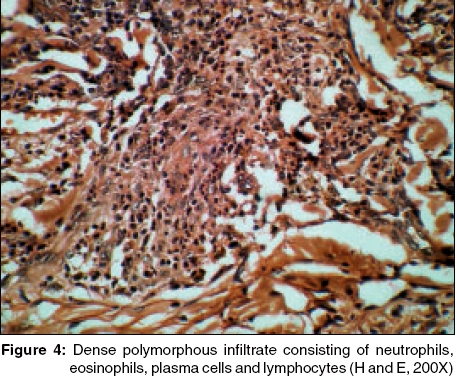 |
 |
 |
 |
 |
 |
 |
 |
Introduction
Granuloma faciale (GF) is an uncommon benign chronic skin disease of unknown origin characterized by single or multiple, soft, erythematous to livid papules, plaques or nodules usually occurring on the face, often with follicular accentuation and superficial telangiectasias.[1] The lesions may be asymptomatic or be associated with mild pruritus or a stinging sensation. The term granuloma faciale was first coined by Pinkus in 1952.[2] The sites of predilection are the sides of nose (30%), tip of the nose (7%), preauricular area (22%), cheeks (22%), forehead (15%) and helix of the ear (4%).[3] Extrafacial or disseminated GF has been reported but is very rare . [4],[5],[6],[7],[8],[9],
Case report
A 52-year-old lady presented with multiple asymptomatic, variably sized, brownish-black colored, firm, sharply circumscribed plaques varying in size from 5 mm to 4 cm over both the cheeks [Figure - 1], pinna of the left ear, right upper arm [Figure - 2] and right breast of 4 years′ duration. The initial lesion developed on the left cheek. The course of the disease was gradually progressive, with development of new lesions on the right cheek, left ear lobule, right arm and right breast in that order. The follicular openings over these were exaggerated. The lesion on the left cheek showed a central depression, giving an annular appearance. There was no systemic involvement. The clinical differential diagnoses considered were keloid, discoid lupus erythematosus, nodular sarcoidosis, cutaneous leishmaniasis, granuloma annulare and erythema elevatum diutinum.
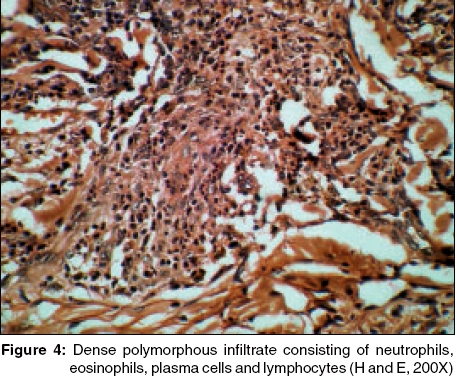
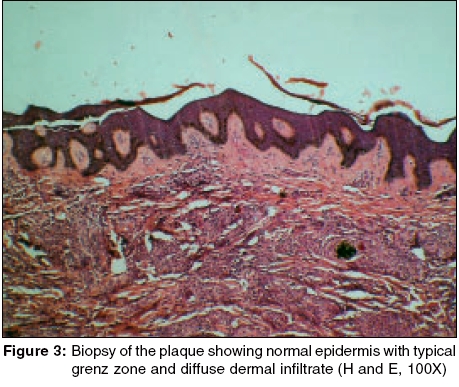
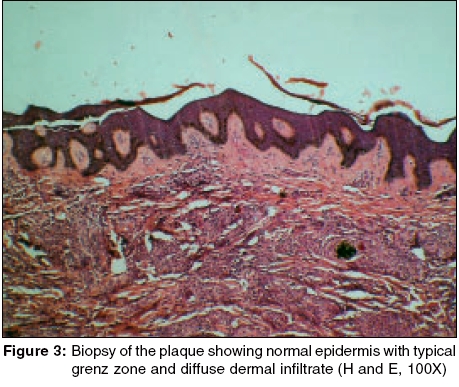
Routine hematological investigations, urinalysis and all other biochemical parameters were within normal limits. Skin biopsies were obtained from the left pinna and the right arm. Histopathological studies of the facial and extrafacial lesions showed similar characteristics. The epidermis was unremarkable. There was a narrow grenz zone of uninvolved dermis between the epidermis and the dense dermal accumulation of an inflammatory infiltrate [Figure - 3] comprising of neutrophils, eosinophils, monocytes and lymphocytes, thereby confirming the diagnosis of granuloma faciale [Figure - 4].
She was administered oral dapsone 100 mg daily for 3 months with no response. Local infiltration of triamcinolone acetonide 20 mg/ml combined with cryotherapy repeated at weekly intervals for 6 weeks led to only partial flattening of the lesions. Finally, the lesions on both cheeks were excised followed by grafting by a reconstructive surgeon. The excised tissue was subjected to histopathological examination and it reconfirmed the diagnosis of GF. The patient was satisfied with the cosmetic outcome. Follow up after 10 weeks of surgery revealed the development of a fresh nodule over the right cheek at the margin of operation scar. It was managed with intralesional infiltration of triamcinolone acetonide with satisfactory results.
Discussion
The lesions of GF usually involve the nose, forehead or cheeks.[2] Extrafacial involvement is rare and has been reported to involve the back, arms, chest, shoulders and thighs. [4],[5],[6],[7],[8],[9], Our case had involvement of the right arm and right breast in addition to the facial lesions. The keloidal appearance of the lesions in our patient was quite striking and has not been reported. Similarly, involvement of the ear lobule has not been reported. The histopathological findings of facial and extrafacial lesions revealed the typical features of GF.
There are both clinical and histological similarities between extrafacial GF and erythema elevatum diutinum (EED), and some authors suggest an association between the two conditions.[10] However, the symmetrical and acral involvement clinically, as well as the absence of Grenz zone with notable fibrosis histologically, helps distinguish EED from GF.
GF is notoriously resistant to treatment. Many different medical therapies, including topical or intralesional corticosteroids, dapsone, antimalarials, isoniazid, clofazimine and topical nitrogen mustard, have been tried with variable results. A variety of surgical procedures, like surgical excision, dermabrasion, argon laser, pulsed dye laser,[11] carbon dioxide laser, electrosurgery and cryotherapy,[12] have been used for the management of GF. Our patient failed to respond to dapsone and intralesional corticosteroids combined with cryotherapy; hence she was managed with surgical excision followed by grafting with highly satisfactory results. She is under regular follow up to detect any relapse of the skin lesions.
| 1. |
Pedace FJ, Perry HO. Granuloma faciale: a clinical and histopathologic review. Arch Dermatol 1966;94:387-95.
[Google Scholar]
|
| 2. |
Pinkus H. Granuloma faciale. Dermatologica 1952;105:85-99.
[Google Scholar]
|
| 3. |
Sears JK, Gitter DG, Stone MS. Extrafacial granuloma faciale. Arch Dermatol 1991;127:742-3.
[Google Scholar]
|
| 4. |
Rusin LJ, Dubin HV, Taylor WB. Disseminated granuloma faciale. Arch Dermatol 1976;112:1575-7.
[Google Scholar]
|
| 5. |
Castano E, Segurado A, Iglesias L, Lopez-Rios F, Rodriquez-Peralto JJ. Granuloma faciale entirely in an extrafacial location. Br J Dermatol 1997;136:978-9.
[Google Scholar]
|
| 6. |
Konohana A. Extrafacial granuloma faciale. J Dermatol 1994;21:680-2.
[Google Scholar]
|
| 7. |
Roustan G, Sanchez YE, Salas C, Simon C. Granuloma faciale with extrafacial lesions. Dermatology 1999;198:79-82.
[Google Scholar]
|
| 8. |
Castelleno-Howard L, Fairbee SI, Hogan DJ, Fenske NA, Messina JL. Extrafacial granuloma faciale: report of case and response to treatment. Cutis 2001;67:413-5.
[Google Scholar]
|
| 9. |
Zagari O. Disseminated granuloma faciale. Int J Dermatol 2004;43:210-2.
[Google Scholar]
|
| 10. |
Ackerman AB, Mones JM, Petronic-Rosic V. Ackerman's Resolving quandaries in dermatology, pathology, and dermatopathology. New York: Ardor Scribendi; 2001.
[Google Scholar]
|
| 11. |
Welch JH, Schroeder TL, Levy ML. Granuloma faciale in a child successfully treated with the pulsed dye laser. J Am Acad Dermatol 1999;41:351-3.
[Google Scholar]
|
| 12. |
Dowlati B, Firooz A, Dowlati Y. Granuloma faciale: successful treatment of nine cases with a combination of cryotherapy and intralesional corticosteroid injection. Int J Dermatol 1997;36:548-51.
[Google Scholar]
|
Fulltext Views
2,880
PDF downloads
2,152





