Translate this page into:
Family vitiligo impact scale: A scale to measure the quality-of-life of family members of patients with vitiligo
Corresponding author: M. Ramam, Department of Dermatology and Venereology, All India Institute of Medical Sciences, New Delhi, India. mramam@hotmail.com
-
Received: ,
Accepted: ,
How to cite this article: Agrawal S, Satapathy S, Gupta V, Sreenivas V, Khaitan BK, Ramam M. Family vitiligo impact scale: A scale to measure the quality-of-life of family members of patients with vitiligo. Indian J Dermatol Venereol Leprol 2022;88:32-9.
Abstract
Background:
Vitiligo places a significant psycho-social burden on caregivers and family members.
Aims:
The aim of the study was to develop and preliminarily validate a scale to measure the psychosocial impact of vitiligo on adult family members.
Methods:
Themes that emerged from qualitative interviews and a focus group discussion with family members were used to generate items for a preliminary scale, followed by pre-testing and scale development. The new scale was then tested with two comparator scales and a global question.
Results:
A preliminary scale with 32 items was pilot tested on 30 participants. Following this, the scale was condensed to 16 items in 12 domains that were administered to 159 participants. Scale scores ranged from 0 to 48 with a mean of 19.75 ± 12.41. The scale had excellent internal consistency with Cronbach’s alpha coefficient of 0.92 (0.70–0.95) and also showed good test-retest reliability at two weeks (r = 0.946). The scale showed criterion, convergent and known group validity.
Limitations:
It was conducted in a large teaching hospital which may have resulted in selection of patients with persistent or progressive disease and more worried family members. Vitiligo is highly stigmatized in our country and the performance of the scale may need to be evaluated in other communities and cultures as well where stigma is less oppressive.
Conclusion:
Family Vitiligo Impact Scale appears to be an easy-to-complete, reliable and valid instrument to measure the psychosocial impact of vitiligo in family members of patients. It may be useful as an outcome measure in both clinical and research settings.
Keywords
Family quality of life
psychosocial impact
scale development
vitiligo
Plain Language Summary
Vitiligo leads to white patches on the skin and this causes significant psychological and social distress. Family members of the affected person may also be distressed and this has not received much attention. We talked to family members to identify what they were concerned about and used this information to develop a questionnaire consisting of 16 questions called the Family Vitiligo Impact Scale. This questionnaire was used to evaluate the impact of vitiligo in 159 family members and compared to two other questionnaires that assess the impact of any illness (Family Strain Questionnaire-Short Form) and skin disease in general (Family Dermatology Life Quality Index). We found that the Family Vitiligo Impact Scale is a reliable and valid measure of the impact of vitiligo on family members. It can be used both for research and for identifying family members who require help for their distress.
Introduction
Vitiligo is often associated with a significant impairment in quality of life because of the cosmetic disfigurement, social stigma, unpredictable course and variable response to treatment.1 Patients having vitiligo report a sense of humiliation, embarrassment, low self-esteem, social anxiety, isolation and depression.2,3
The psycho-social burden of the disease is not restricted to patients but is borne by family members as well. The psychosocial impact of chronic illnesses on family members and caregivers has been studied in several diseases such as psoriasis,4,5 atopic dermatitis,6,7 alopecia areata,8 ichthyosis,9 and epidermolysis bullosa10 and scales have been developed to measure the family impact of these diseases. Although instruments such as vitiligo-specific health-related quality of life intrument11 and Vitiligo Impact Scale-2212 have been developed to measure the quality of life of patients with vitiligo, no instrument is available to assess the impact on family members.
Aims and objective
The aim of the study was to develop and preliminarily validate a scale to measure the psychosocial impact on adult family members of patients with vitiligo.
Methods
Study design and inclusion-exclusion criteria
Items were generated using qualitative study methods. Adult family members of patients with vitiligo living in the same household, having a close relationship, and who accompanied them for treatment, were included in the study. Subjects were excluded if the patient or the family member had another significant physical or psychological illness, disability, or any other chronic skin disease. All participants provided written informed consent and the study was approved by the Ethics Committee at our institute.
Recruitment of subjects
A total of 220 subjects were recruited at different stages of scale development from among family members who accompanied patients with vitiligo to skin outpatient department and pigmentation clinic at the All India Institute of Medical Sciences, New Delhi [Figure 1]. We included 31 subjects for item generation, 30 for the pilot study and 159 for final scale testing.

- Flow chart depicting different phases of scale development
Item generation
Twenty three in-depth key interviews and one focus group discussion with eight family members of patients with vitiligo were conducted using semi-structured guides by two skilled interviewers and a trainee dermatologist. Participants were chosen by purposive sampling to select those who would be able to articulate their feelings and thoughts about the disease. The interviews were carried out till every question in the guide was covered and the interviewee had nothing more to say.
The interviews and focus group discussion were digitally recorded and transcribed verbatim. Content analysis was done by one of us (SA) initially and was further checked and re-coded by three independent clinical psychologists till saturation and agreement on final sub-themes and domains were reached.13
One hundred and twenty three subthemes were generated to categorize the collected data into broader themes and domains and 116 items were generated from these sub-themes. The draft scale was pruned by an expert group of three dermatologists, a clinical psychologist and a dermatology trainee at several stages to yield a preliminary scale with 32 items.
Pilot testing
The preliminary scale was administered to 30 family members and feedback was sought regarding thoroughness, readability, length and ease of understanding by one-on-one interviews. Statistical analysis was done to determine inter-item correlation and Cronbach’s alpha coefficient.
Final scale
The final selection of items for the scale was based on statistical results of pilot testing and expert feedback. Redundant questions, questions with low item-test correlation (<0.3) and questions with response of “0” or those left unanswered were excluded and some questions were reframed for readability and comprehension.
Preliminary validation: psychometric properties
The final scale was administered to a separate cohort of 159 family members along with two comparator scales, Family Dermatology Life Quality Index,14 and Family Strain Questionnaire-Short Form.15 In addition, family members responded to a global question on “How much does your family member’s vitiligo affect your life?” in a 4-point response format (0: Not at all, 1: A little, 2: A lot and 3: Very much).
Twenty of these subjects were administered the scale again, along with two comparator scales, after two weeks to ascertain test-retest reliability.
A linguistically validated Hindi translation of Family Dermatology Life Quality Index was obtained from authors of the questionnaire.
A Hindi translation of Family Strain Questionnaire-Short Form is not available and we prepared it using the following methodology: two independent translators translated the questionnaire from English to Hindi, discussed their translations and agreed on a common translation. A third and fourth translator independently back translated the Hindi language version back into English. The back translations were reviewed and an optimal Hindi version was finalized.
Factor analysis
Exploratory factor analysis with varimax rotation and Kaiser normalization was performed to determine the factor structure of the scale. Factor loading cutoff of 0.40 and Eigenvalue >0.80 was adopted for fixing the number of factors.
Validity
We assessed the criterion validity by correlating the final scale scores with the global question, which served as the gold standard, using Spearman’s rank correlation. Convergent validity of the scale was tested by correlating final scale scores with comparator scales Family Strain Questionnaire-Short Form and Family Dermatology Life Quality Index, assuming that final scale scores measured impact similar to the generic scales. Known-group/construct validity for the scale was estimated by testing a number of a priori assumptions which were that female family members, less educated family members and mothers would have a higher score indicating a higher psychosocial impact. We also assumed that the scores would be higher in family members of female patients with vitiligo, those who had progressive and extensive disease, vitiligo on exposed/visible sites, non-segmental vitiligo, had undertaken dietary restrictions in response to disease and had a higher self-reported psychosocial impact.
Internal consistency
The final scale was evaluated for internal consistency using Cronbach’s alpha coefficient and internal structure validity using inter-item correlation matrix.
Statistical analysis
Statistical analysis was carried out using Stata version 14.2 (Stata Corp. 2011. Stata Statistical Software: Release 14.2. College Station, TX: Stata Corp LP.) and SPSS (SPSS Inc. Released 2008. SPSS Statistics for Windows, Version 17.0. Chicago: SPSS Inc.)
Results
Item generation and preliminary scale development
Of the 67 family members screened, 31 family members consented to participate in the first phase of the study. We carried out one-on-one in-depth key interviews with 23 family members of 23 patients and focus group discussion with eight family members of five patients who included parents and siblings. They revealed several concerns such as emotional stress, worry, sadness, preoccupation with disease and anxiety about the future. The treatment of vitiligo was reported to be cumbersome and costly requiring regular follow-up and multiple visits to the doctor because of its prolonged and unpredictable course. Parents were worried about their child’s education and future and distressed about the emotional burden faced by the child. A leading concern was anticipated difficulties in marriage, not only of the vitiligo-affected person but also of other unaffected family members.
One hundred and twenty three sub-themes were identified from transcripts of interviews and focus group discussion and were categorized into 17 broad domains after content analysis by three independent clinical psychologists. A brief thematic network representing different domains and sub-themes is shown in Figure 2. Based on the verbatim statements, 116 items/questions were generated and some redundant sub-themes were eliminated. Of the 17 domains, four domains associated with occupation, household chores, leisure and physical health were clubbed into one domain “functionality.” Two domains of spousal inter-personal relationship and spousal-disclosure difficulty were also merged into one. Hence, a total of 116 items/questions were generated and were clubbed into 13 broad domains: impact on affect, treatment adherence, functionality, social impact, disease understanding, behavior, coping mechanism, spousal relationship, familial conflicts, child’s academic functioning, disclosure difficulty, financial burden and cognition. This draft scale was further pruned by two dermatologists and one clinical psychologist to 40 questions by clubbing together those questions that reflected similar sub-themes or core issues and removing those that were redundant. The questions were then triaged by three independent dermatologists and principal investigator into those that must be kept, may be kept or must be deleted and a ranking list of domains was created based on the number of questions selected in each domain and thus, a preliminary scale with 32 questions was made.
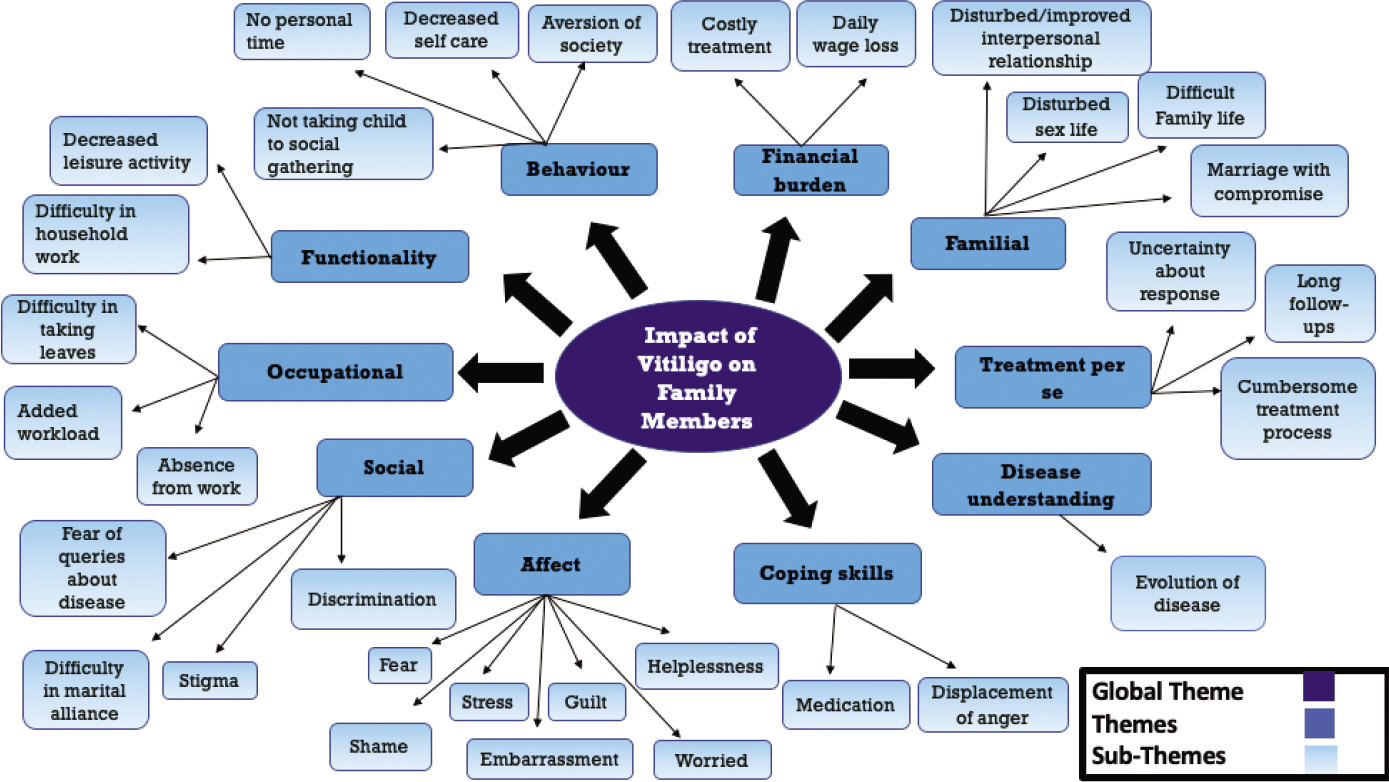
- Thematic network showing different domains and items. (This figure is representational and does not include all 13 domains)
Pilot testing
The preliminary scale was administered to a separate cohort of 30 family members whose ages ranged from 25 to 55 years (mean ± SD: 37.2 ± 8.1 years). There were 19 males and 11 females who included 14 fathers, ten mothers, three husbands, one wife and two brothers. The duration of vitiligo in patients ranged from six months to 12 years (mean ± SD: 3.57 ± 2.82 years). The internal consistency of preliminary scale was high with a Cronbach’s alpha coefficient16 of 0.90 and inter-item correlation for all items was between 0.15 and 0.45. Based on the results of pilot test and the expert opinion of three clinical dermatologists and one clinical psychologist, one domain was removed and 16 questions were finally chosen that best reflected the psychosocial impact of vitiligo among family members.
Final scale
The final scale with 16 items belonged to 12 broad domains: disease understanding (item 14), treatment (item 11), social impact (item one, two and 12), impact on affect (item four and ten), financial burden (item six), functionality, physical (item three and 13), functionality, occupational (item five), functionality, leisure (item eight), familial conflicts (item 15), cognition (item nine), affected family member’s functioning (item seven) and interpersonal relationship (item 16) [Figures 3 and 4].

- Family vitiligo impact scale with response categories (English)
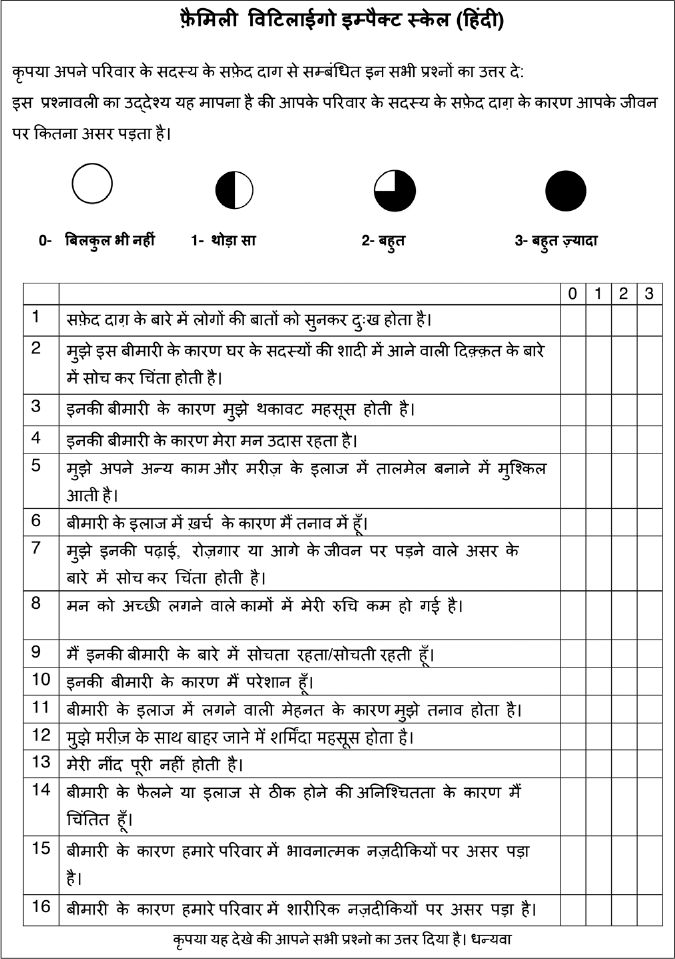
- Family vitiligo impact scale with response categories (Hindi)
Socio-demographic profile of the sample
The final psychometric analysis was carried out on 159 adult family members of 159 patients with vitiligo. There were 98 (62%) males and 61 (38%) females with a mean age of 37.2 ± 11.7 years. There were 46 (28.9%) fathers, 35 (22%) mothers, 19 (12%) spouses, 32 (20.1%) siblings, 14 (8.8%) children, seven (4.4%) uncles and aunts and four (2.5%) grandparents. Five (3.1%) family members had received primary education while the other 154 had middle school or higher education [Table 1].
| Age | Range: 3–73, mean(±SD): 19.92(±13.81) years | ||
|---|---|---|---|
| Gender | |||
| Male | 61(38%) | ||
| Female | 98(62%) | ||
| Duration | Range: One month-24years, mean(±SD): 4.47±(4.16) years | ||
| Type | |||
| Non-segmental | 141(88.7%) | Acrofacial | 94(66.6%) |
| Generalized | 35(24.8%) | ||
| Focal | 9(6.3%) | ||
| Mucosal | (0.7%) | ||
| Segmental | 13(8.1%) | ||
| Mixed | 5(3.1%) | ||
| Disease activity | |||
| Progressive | 79(50.3%) | ||
| Non-progressive | 80(50.3%) | ||
| BSA(%) | |||
| ≤1 | 77(48.4%) | ||
| 2–5 | 64(40.2%) | ||
| >5 | 18(11.3) | ||
| Site of involvement | |||
| Visible | 130(82%) | ||
| Exclusively covered | 29(18%) |
Language of the scale
One hundred and forty eight family members responded in Hindi and 11 in English.
Scale scores
Family Vitiligo Impact Scale scores ranged from 0 to 48 with a mean of 19.75 ± 12.41. The most commonly affected domain was social in 148 (93.1%) family members which included items related to feeling sad on hearing social responses/ queries about disease, effects of disease on marriages in the family and feeling embarrassed on going out with the patient to social events. The next most affected domains were affect in 138 (86.8%) family members, followed by cognition in 135 (84.9%), disease understanding in 129 (81.1%) and academic performance of affected family member in 124 (77.8%). The domain of interpersonal relationship was least affected 43 (27%). The mean Family Dermatology Life Quality Index score was 9.44 ± 7.08 (0-30) and mean Family Strain Questionnaire-Short Form score was 14.72 ± 7.23 (0-30). Only 3.8% of respondents scored 0 and 1.9% showed maximum score of 48, suggesting no significant floor or ceiling effects shown by the scale.
Factor analysis
Sample size was adequate as indicated by Bartlett’s test of sphericity (0.00) and Kaiser-Meyer-Olkin measure of sampling adequacy (0.92). The scale exhibited one dominant factor accounting for 48.8% of the common variance indicating that a single total score of the final scale could be used to determine the psychosocial impact. Three major domains were identified based on factor loading of items with standard regression coefficients of more than 0.3. Three main factors with eigenvalues greater than 1.0 emerged and were included as scale domains and these three factors together accounted for 65.9% of the common variance, which was higher than the minimum recommendation (50%) for a stable factor solution as shown in Figure 5.

- Scree plot showing eigenvalues against each factor, showing one dominant factor
Although there was one dominant factor in the factor loading, three domains were found to be statistically and clinically relevant to a decision for mental health referral, if required. They were labeled as social impact, which loaded three items (people’s reaction and effect on marriages and cognition), emotional impact which loaded seven items (affect, child’s functioning, disease uncertainty, treatment and financial burden) and well-being which loaded six items (physical health, impact on leisure and social gatherings and impact of relationship) as shown in Table 2. The factor loading scores of all items in final scale were between 0.15 and 0.45 indicating that none of the items were redundant and all items contributed to measurement of impact.
| Family Vitiligo Impact Scale Items | Component | ||
|---|---|---|---|
| Emotional impact | Well-being | Social Impact | |
| People’s reaction | 0.853 | ||
| Effect on marriage | 0.738 | ||
| Physical health | 0.552 | 0.349 | |
| Affect | 0.532 | 0.528 | |
| Burden of care | 0.593 | 0.442 | |
| Financial burden | 0.562 | 0.399 | |
| Child’s functioning | 0.746 | ||
| Leisure | 0.526 | 0.534 | |
| Cognition | 0.530 | 0.624 | |
| Affect | 0.659 | 0.439 | |
| Treatment per se | 0.567 | 0.550 | |
| Embarrassed on going out | 0.858 | ||
| Physical health | 0.451 | 0.601 | |
| Disease uncertainty | 0.731 | ||
| Familial conflicts | 0.715 | ||
| Inter personal relationship | 0.827 | ||
Psychometric properties of the scale
Test-retest reliability
The mean scale scores at baseline and at two weeks in 20 patients were 22.8 and 21.35, respectively; the difference was not statistically significant. (P = 0.128, Pearson’s correlation coefficient = 0.946).
The internal consistency of the total scale was high with Cronbach’s alpha coefficient of 0.9257. The inter-item correlation was higher than 0.3 in all items, indicating that all questions contributed to the construct of the scale. The internal consistency for all 16 items ranged from 0.9229 for item eight to 0.9292 for item 1. The Cronbach’s coefficients for the three identified domains were 0.9257, 0.9261 and 0.9254, respectively, thus remaining unchanged, item and domain wise.
Validity
Criterion validity was demonstrated by positive correlation of scale scores with global question response scores (Spearman rank correlation r = 0.848, P < 0.001). Scale scores showed significant positive correlation with both Family Dermatology Life Quality Index scores (r = 0.685) and Family Strain Questionnaire-Short Form scores (r = 0.596, P = 0.001) suggesting convergent validity.
The mean scale scores were lower for better-educated family members (39 ± 6.63 vs. 13.8 ± 9.41, P < 0.001) and in family members of patients who did not undertake dietary modifications (21.67 ± 11.80 vs. 16.90 ± 12.84, P = 0.01), were older (<five years 10.5 ± 12.2 vs. >20 years 16.4 ± 11.3, P = 0.004) and had vitiligo for a longer duration (<five years 21 ± 12.7 vs. >ten years 13.5 ± 12.0, P = 0.048). Mean scores were significantly higher when patients had vitiligo on visible areas (20.81 ± 12.46 vs. 15 ± 12.21, P = 0.02). Scores were also higher when the affected patient had progressive disease, extensive disease and a higher self-reported psychosocial burden but the differences were not significant. Parents had a significantly higher mean score than spouses (22.1 ± 2.2 vs. 15.3 ± 11.7, P = 0.03).
Scale cutoff score
A receiver operating characteristic curve of Family Vitiligo Impact Scale scores against scores of Family Strain Questionnaire-Short Form [Figure 6] was plotted. A cutoff score of >9 on Family Strain Questionnaire-Short Form indicates a clinically significant psychosocial impact that may require further evaluation and counseling and this corresponded to a score of >13 on Family Vitiligo Impact Scale (sensitivity 84% and specificity 87.5%).17
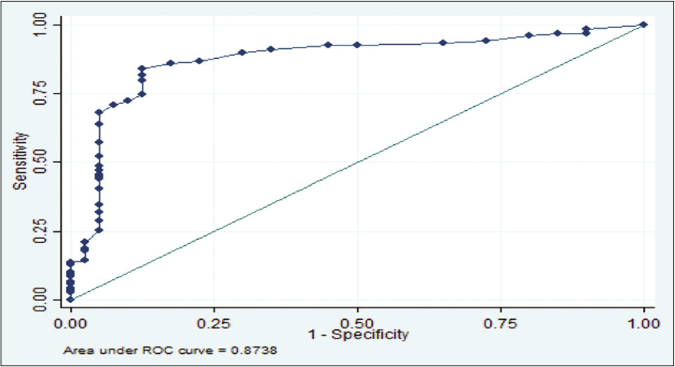
- Receiver operating characteristic curve of Family Vitiligo Impact Scale versus Family Strain Questionnaire-Short Form: Area under the curve is 0.87; (sensitivity: 84% and specificity: 87.5%)
Discussion
Scales to measure the impact on family members are available for skin diseases in general15 and for specific diseases such as psoriasis,4,5 atopic dermatitis,6,7 and ichthyosis.9 Previous studies using a generic scale have documented the psychosocial impact of vitiligo in family members18-20 but there is no disease-specific scale for this purpose.
We developed and preliminarily validated an instrument for adult family members of patients with vitiligo. Exploratory factor analysis revealed three distinctive factors and a single total Family Vitiligo Impact Scale score was used to indicate clinically significant psycho-social impact. The scale had excellent internal consistency (Cronbach’s alpha coefficient of 0.9257) and good test-retest reliability at two weeks (r = 0.946).
We observed that the social domain was most affected among family members (93.1%) somewhat similar to the findings of Eghlileb et al.4 who evaluated different ways in which psoriasis affected the lives of 28 relatives and 35 spouses of 65 patients. They reported that the social lives of 35 (55%) family members were affected. The much higher social burden in vitiligo highlights the distinctively different order of stigma and discrimination associated with vitiligo as compared to other skin diseases.
We found significantly higher scores for our scale in those family members who were less educated although other workers found higher education associated with greatet psycho-social impact18. This was probably because education helps facilitate better understanding of disease course and treatment response leading to a reduction in anxiety. Mothers had higher scores than fathers, spouses and other relatives, as also noted by Amer et al.19 probably due to a greater emotional attachment to children. Scale scores were higher when patients had vitiligo on exposed sites leading to greater social stigma, as also observed by Gahalaut et al.20 With increased duration of disease, there was a decrease in scores attributable to the family learning to adjust and acquiring the necessary coping skills. Scores were also higher when the affected patient avoided certain foods as part of treatment regimen, probably reflecting concern about a member having to forgo foods that are part of the family's normal diet.
Limitations
Our study had some limitations. It was conducted in a large teaching hospital which may have resulted in selection of patients with persistent or progressive disease and more worried family members. Husbands were under-represented in the study as some women wanted to keep the disease a secret from their spouse and extended family. Vitiligo is highly stigmatized in our country and the performance of the scale may need to be evaluated in other communities and cultures where stigma is less oppressive.
Conclusion
Family Vitiligo Impact Scale appears to be an easy to complete, reliable and valid instrument to measure the psychosocial impact of vitiligo in family members of patients. Scores may help guide clinicians in providing early psycho-social support and education and identify those requiring referral to a psychiatrist/psychologist.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Vitiligo: A comprehensive overview Part I. Introduction epidemiology, quality of life, diagnosis, differential diagnosis, associations, histopathology, etiology, and work-up. J Am Acad Dermatol. 2011;65:473-91.
- [CrossRef] [PubMed] [Google Scholar]
- Childhood vitiligo and tacrolimus: Immunomodulating treatment for an autoimmune disease. Arch Dermatol. 2003;139:651-4.
- [CrossRef] [PubMed] [Google Scholar]
- Dermatology specific quality of life in vitiligo patients and its relation with various variables: A hospital based cross-sectional study. J Clin Diagn Res. 2014;8:YC01-3.
- [CrossRef] [PubMed] [Google Scholar]
- The psoriasis family index: Preliminary results of validation of a quality of life instrument for family members of patients with psoriasis. Dermatology. 2009;219:63-70.
- [CrossRef] [PubMed] [Google Scholar]
- FamilyPso-a new questionnaire to assess the impact of psoriasis on partners and family of patients. J Eur Acad Dermatol Venereol. 2017;31:127-34.
- [CrossRef] [PubMed] [Google Scholar]
- The quality of life of parents of children with atopic dermatitis: Interpretation of PIQoL-AD scores. Quality of Life Res. 2005;14:2235-45.
- [CrossRef] [PubMed] [Google Scholar]
- The family impact of childhood atopic dermatitis: The Dermatitis Family Impact Questionnaire. Br J Dermatol. 1998;138:107-13.
- [CrossRef] [PubMed] [Google Scholar]
- Alopecia areata is associated with impaired health-related quality of life: A survey of affected adults and children and their families. J Am Acad Dermatol. 2018;79:556-8.
- [CrossRef] [PubMed] [Google Scholar]
- Family burden in inherited ichthyosis: Creation of a specific questionnaire. Orphanet J Rare Dis. 2013;8:28.
- [CrossRef] [PubMed] [Google Scholar]
- Development and validation of an epidermolysis bullosa family/parental burden score. Br J Dermatol. 2015;173:1405-10.
- [CrossRef] [PubMed] [Google Scholar]
- Development and validation of a vitiligo-specific quality-of-life instrument (VitiQoL) J Am Acad Dermatol. 2013;69:e11-8.
- [CrossRef] [PubMed] [Google Scholar]
- Measurement properties of the Vitiligo Impact Scale-22 (VIS-22), a vitiligo-specific quality-of-life instrument. Br J Dermatol. 2014;171:1084-90.
- [CrossRef] [PubMed] [Google Scholar]
- A hands-on guide to doing content analysis. Afr J Emerg Med. 2017;7:93-9.
- [CrossRef] [PubMed] [Google Scholar]
- The Family Dermatology Life Quality Index: Measuring the secondary impact of skin disease. Br J Dermatol. 2007;156:528-38.
- [CrossRef] [PubMed] [Google Scholar]
- Family strain questionnaire-short form for nurses and general practitioners. J Clin Nurs. 2010;19:275-83.
- [CrossRef] [PubMed] [Google Scholar]
- Applied Logistic Regression In: Wiley Series in Probability and Statistics (2nd ed). New York: John Wiley and Sons Inc; 2000.
- [Google Scholar]
- Quality of life in family members of vitiligo patients: A questionnaire study in Saudi Arabia. Am J Clin Dermatol. 2013;14:489-95.
- [CrossRef] [PubMed] [Google Scholar]
- Hidden victims of childhood vitiligo: Impact on parents' mental health and quality of life. Acta Derm Venereol. 2015;95:322-5.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of occurrence of vitiligo in children over quality of life of their families: A hospital-based study using family dermatology life quality index. Indian J Paediatr Dermatol. 2018;19:21-5.
- [CrossRef] [Google Scholar]






