Translate this page into:
Primary nonessential cutis verticis gyrata with acne keloidalis nuchae
Corresponding author: Dr. Varadraj Pai, Department of Dermatology, Goa Medical College, Goa, India. docpai@rediffmail.com
-
Received: ,
Accepted: ,
How to cite this article: Nachinolcar SN, Pai V, Shukla P, Muthuprabhakaran K. Primary nonessential cutis verticis gyrata with acne keloidalis nuchae. Indian J Dermatol Venereol Leprol, doi: 10.25259/IJDVL_1050_19
Abstract
Cutis verticis gyrata is a rare disorder characterized by redundant skin forming deep furrows and convolutions. It has been associated with several systemic and cutaneous disorders. We report a case of primary non-essential cutis verticis gyrata in association with acne keloidalis nuchae in a schizophrenic patient.
Keywords
Acne keloidalis nuchae
cutis verticis gyrata
schizophrenia
Introduction
Cutis verticis gyrata, also known as cutis verticis plicata, “bulldog or corrugated scalp,” is a rare benign cutaneous disorder characterized by raised folds and furrows resembling sulci and gyri of the brain.1
It may be classified into primary (essential and nonessential) and secondary variants. Primary cutis verticis gyrata is rare, characterized by the absence of neurological and ophthalmological changes any other known etiology. Secondary disease may result from several dermatological conditions.2
Acne keloidalis nuchae is an idiopathic chronic granulomatous condition involving the nape of neck or occipital scalp, predominantly affecting young adult males.3
Here, we report an uncommon case of primary non-essential cutis verticis gyrata in a young adult male in association with acne keloidalis nuchae.
Case Report
A 35-year-old male presented with thickened skin over his scalp and history of purulent discharge over the back of scalp for last 20 and 10 years respectively. There was no history of trauma or irritation prior to of skin thickening. The patient reported treatment with fluvoxamine and olanzapine for schizophrenia since last 15 years. No neurological or ophthalmological complaints were elicited.
Examination revealed multiple convoluted anteroposterior folds over the parieto-occipital area which were soft in consistency and could not be flattened on pressure. Hair was normal over the area [Figure 1]. Additionally, we observed an irregular, well-defined plaque, over the occipital region, approximately 4 × 10 cm. The surface demonstrated multiple skin colored to erythematous papules to and few pustules covered with crusting and minimal yellowish discharge along with occassional tufted hair follicles [Figure 2]. On dermoscopy, perifollicular pustules and tufted hair were seen along with interspersed whitish areas [Figure 3]. Histopathology revealed Dermal fibrosis with chronic inflammatory infiltrate [Figure 4]. Computerized tomography of brain was unremarkable. Serum testosterone and free insulin concentration were within normal limits. Based on above findings, we made a diagnosis of primary non-essential cutis verticis gyrata with acne keloidalis nuchae in a schizophrenic patient.

- Multiple convoluted folds over the scalp
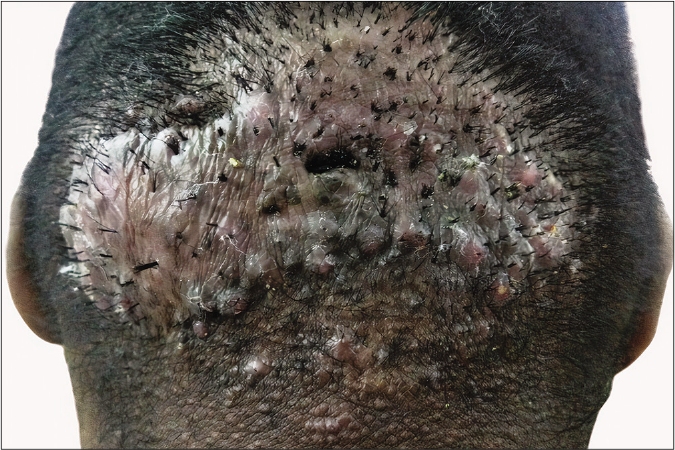
- Erythematous papules to pustules with a few hair tufts
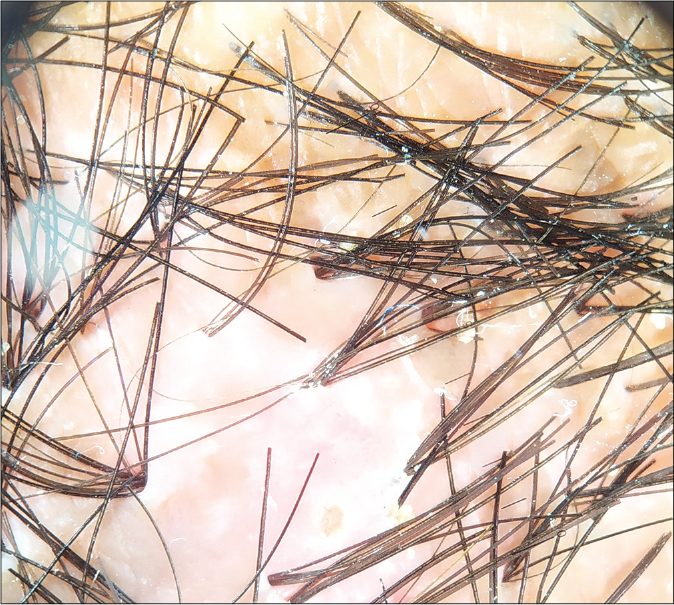
- Dermoscopic image showing perifollicular pustules and tufted hair (×10, polarized light, Heine Delta 20)
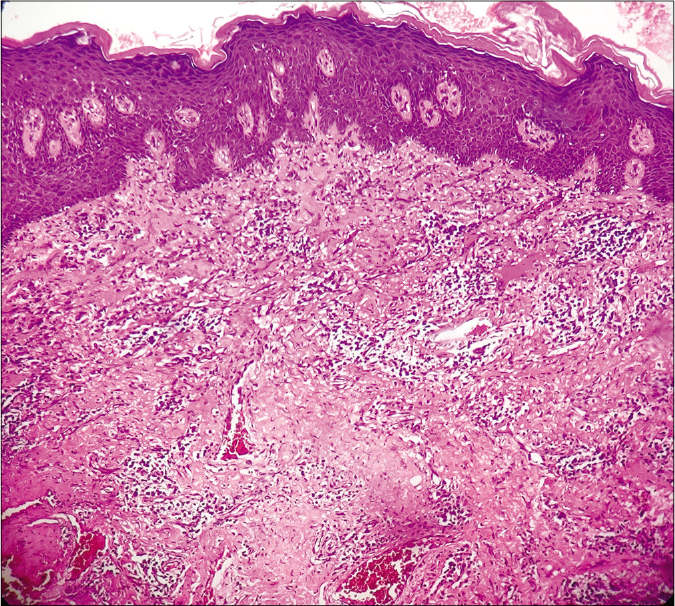
- Dermis shows fibrosis with chronic inflammatory infiltrate H and E ×200
The patient was treated for acne keloidalis nuchae with appropriate systemic and topical antibiotics followed by intralesional triamcinolone (once a month) and cryotherapy. The patient reported clinical improvement after about eight weeks of treatment [Figure 5].

- Clinical response after 8 weeks of treatment
Discussion
Cutis verticis gyrata was originally described in 1837 by Jean-Louis-Marc Alibert, the term being proposed by Unna in 1907.2 In 1984, it was classified into primary essential (no other abnormality associated) and primary non-essential which can be associated with ophthalmologic abnormalities (cataract, strabismus, blindness and retinitis pigmentosa), central nervous system (mental deficiency, cerebral palsy, epilepsy and schizophrenia), cranial (microcephaly) abnormalities and deafness. The latter has been also called as cutis verticis gyrata and mental retardation or cutis verticis gyrata-intellectual disability syndrome.4
The etiology of primary essential cutis verticis gyrata is unclear. A hormonal cause has been postulated in primary non-essential cutis verticis gyrata as it occurs predominantly in men post puberty and may disappear after castration due to increased peripheral utilization of testosterone.5,6 In our patient, we detected pre-pubertal onset and disease was associated with schizophrenia suggestive of primary non-essential cutis verticis gyrata.
Secondary cutis verticis gyrata may be associated with inflammatory or neoplastic scalp disorders such as eczema, psoriasis, folliculitis, impetigo, erysipelas and pemphigus or other pathologies including hamartomas, nevi, acromegaly and pachydermoperiostosis.7 Our case had concomitant acne keloidalis nuchae; however, it developed after cutis verticis gyrata, thus, ruling out the latter gyrata occurring secondary to an inflammatory condition of the scalp.
Acne keloidalis nuchae, also called folliculitis keloidalis nuchae, is one of the chronic forms of scarring folliculitis commonly involving African males. The inciting agents appear to be multifactorial with various factors such as androgens, inflammation, infection, trauma, genetics and ingrown hairs.8
Acne keloidalis nuchae predominantly involves males, suggesting a direct or indirect role of androgens. It is rare before puberty and rarely develops after 55 years. Inflammation is central to the pathogenesis and the potential antigens include sebum, desquamated keratinocytes, Demodex, normal skin flora and their metabolic by-products. These antigens along with chronic irritation from shirt collars, caps, helmets and wooden combs have been implicated in the pathogenesis of acne keloidalis nuchae.3
The reasons for the localization of acne keloidalis nuchae to the nuchal and occipital areas are unclear. This may occur due to increase in mast cells and dermal papillary dilatation friction from scalp skin folds in this region and possibly obesity.3,9 Association of acne keloidalis nuchae with cutis verticis gyrate is not clear and could be mutually exclusive. However, an endocrine basis may be postulatedas the role of androgens and male preponderance is common in both conditions. Furthermore, the accumulation of secretions in skin folds might have triggered acne keloidalis nuchae in our case.
Cutis verticis gyrata has been associated with acromegaly. Although growth hormone and Insulin-like growth factor 1 levels could not be assessed due to financial constraints, absence of furrowing of facial skin or clinically evident enlargement of bones normal visual field examination and computerized tomography of brain was noted. Pachydermoperiostosis is characterized by the presence of digital clubbing, pachyderma and periosteal hypertrophy which were absent in our patient.10-12
The role of certain drugs such as antiepileptic drugs and cyclosporine, in the etiology of acne keloidalis nuchae has been reported in literature.13 Therefore, the etiologic role of fluvoxamine or olanzapine cannot be ruled out.
The treatment for primary cutis verticis gyrata may be symptomatic or surgical. Local scalp hygiene is important to avoid secretion accumulation, maceration, unpleasant odor and also prevent secondary infections. Surgical options such as total resection of the lesion and grafting, placement of tissue expander in healthy skin and later grafting and partial resection of an abundant portion of the lesion are available.2,5 Treatment of acne keloidalis nuchae includes local hygiene measures, potent topical steroids, intralesional triamcinolone, cryotherapy, systemic therapy like oral tetracycline and retinoids, 1064 nm Nd:YAG or 810 nm diode lasers and surgical excision in unresponsive cases.3
Conclusion
This case has been reported due to rarity of association between cutis verticis gyrata and acne keloidalis nuchae.
Acknowledgment
The authors would like to thank the department of oral and maxillofacial pathology, Goa Dental College, for the histopathology pictures.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- A rare association of scleromyxedema with cutis verticis gyrata. Indian Dermatol Online J. 2016;7:186-9.
- [CrossRef] [PubMed] [Google Scholar]
- Primary essential cutis verticis gyrata-case report. An Bras Dermatol. 2014;89:326-8.
- [CrossRef] [PubMed] [Google Scholar]
- Acne keloidalis nuchae: Prevalence, impact, and management challenges. Clin Cosmet Investig Dermatol. 2016;9:483-9.
- [CrossRef] [PubMed] [Google Scholar]
- Essential primary cutis verticis gyrata, Treatment with the scalp reduction procedure. Arch Dermatol. 1984;120:1480-3.
- [CrossRef] [Google Scholar]
- Cutis verticis gyrata In: Stat Pearls. Treasure Island, FL: Stat Pearls Publishing; 2019.
- [Google Scholar]
- An endocrinological study of patients with primary cutis verticis gyrata. Acta Derm Venereol. 1993;73:348-9.
- [Google Scholar]
- Is cutis verticis Gyrata-Intellectual Disability syndrome an underdiagnosed condition? A case report and review of 62 cases. Am J Med Genet A. 2017;173:638-46.
- [CrossRef] [PubMed] [Google Scholar]
- Summary of North American hair research society (NAHRS)-sponsored workshop on cicatricial alopecia, Duke University Medical Centre, February 10 and 11, 2001. J Am Acad Dermatol. 2003;48:103-10.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical biochemistry and morphological features of acne keloidalis in a black population of acne keloidalis in a black population. Int J Dermatol. 1993;32:714-6.
- [CrossRef] [PubMed] [Google Scholar]
- Cutis verticis gyrata associated with acromegaly. N Engl J Med. 2019;380:e31.
- [CrossRef] [PubMed] [Google Scholar]
- Acromegaly presenting as cutis verticis gyrata. Int J Dermatol. 2008;47:164.
- [CrossRef] [PubMed] [Google Scholar]
- Pachydermoperiostosis mimicking acromegaly: A case report. Indian Dermatol Online J. 2018;9:182-4.
- [Google Scholar]
- Acne keloidalis-like lesions on the scalp associated with antiepileptic drugs. Int J Dermatol. 1990;29:559-61.
- [CrossRef] [PubMed] [Google Scholar]






